Overview of the Clinical Manifestations of Hypothyroidism
Michael T. McDermott
Introduction
Hypothyroidism is a disorder in which the thyroid gland is unable to synthesize and secrete sufficient amounts of thyroid hormone to meet the requirements of the brain and peripheral tissues. Primary hypothyroidism refers to thyroid failure that results from disease of the thyroid gland itself; this condition accounts for over 99% of all cases of hypothyroidism (1). Central hypothyroidism is the term for thyroid failure caused by pituitary or hypothalamic disorders that result in deficient pituitary production of thyroid-stimulating hormone (TSH) (1,2). Overt hypothyroidism describes moderate-to-severe thyroid failure resulting in high serum TSH levels associated with low serum concentrations of total thyroxine (T4) or free T4. Subclinical hypothyroidism refers to mild thyroid failure in which serum TSH levels are moderately increased but serum total T4 and free T4 values remain within the population reference range (3). The incidence of hypothyroidism is estimated to be 4 to 5 per 1000 population per year for women and 0.6 to 0.9 per 1000 population per year for men (4,5). The prevalence of overt hypothyroidism is approximately 1% to 2% in women and 0.1% in men (5,6,7,8); subclinical hypothyroidism is more common, being reported in 4% to 10% of various populations (5,6,7,8,9,10,11,12,13) and in up to 18% of the elderly (9,10,11,12,13). Approximately 5% to 18% of patients with subclinical hypothyroidism progress to overt hypothyroidism each year (4,12,13,14,15). Risk factors for this progression include higher baseline serum TSH levels, positive antithyroid antibodies and a history of treatment with radioactive iodine or external beam radiation (16,17). However, many individuals with subclinical hypothyroidism remain stable for years and some even regress back to normal thyroid function (16,17,18,19).
Symptoms and Signs
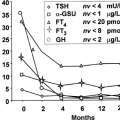
The clinical manifestations of hypothyroidism result primarily from deficient thyroid hormone action at the tissue level. Since thyroid hormone has receptors in and important physiologic effects on most of organs and tissues of the body, the clinical features of thyroid hormone deficiency are quite diverse and often involve multiple systems (7,20,21,22,23,24). The most commonly reported symptoms and signs of overt primary hypothyroidism are shown in Table 39.1. Elderly patients with hypothyroidism have been reported to experience prominent fatigue and weakness but other classical symptoms and signs occur less commonly than in younger individuals (25). System and organ specific features are discussed in more detail below and in subsequent chapters. Depending on the specific etiology, thyroid palpation may reveal a gland that is enlarged (goiter), firm, granular in texture, tender, normal, small or absent. The manifestations of central hypothyroidism are usually similar to those of primary hypothyroidism but tend to be less severe (2). However, because this condition results from pituitary or hypothalamic disease, the clinical picture may be dominated by pituitary mass effects such as headaches, visual field defects, extraocular muscle palsies, and hypopituitarism. Routine laboratory abnormalities commonly seen in hypothyroidism include macrocytic anemia, hyponatremia, hyper-cholesterolemia, and elevated serum creatine kinase (CK) levels. Specific hormone abnormalities that are characteristic of primary hypothyroidism are elevated serum TSH concentrations (overt and subclinical hypothyroidism) and subnormal values of total T4 and/or free T4 (overt hypothyroidism only). In contrast central hypothyroidism is characterized by low total T4 and/or free T4 levels associated with TSH values that are low, normal or sometimes mildly elevated (2).
Table 39.1 Common Clinical Symptoms and Signs of Overt Hypothyroidism | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
Cardiovascular System (See Chapter 40)
Hypothyroidism is a known risk factor for cardiovascular disease (26,27,28). The development of atherosclerosis is likely due largely to the dyslipidemia (7,29) and hypertension (30) that result from thyroid hormone deficiency. Arterial stiffness (31), increased systemic vascular resistance (28,32), and increased carotid intima-medial thickness (33) have all been linked to thyroid failure. Myocardial dysfunction, both systolic and diastolic, also occurs with hypothyroidism (27,28,34,35,36,37,38,39,40,41); there are well-described reports of hypothyroidism associated congestive heart failure, particularly in individuals with severe thyroid hormone deficiency (42). Pericardial effusions, though usually small and of little significance, have been identified in up to 50% of studied patients with thyroid gland failure (43,44,45,46); pericardial tamponade is rare but has been reported (47). The cardiovascular manifestations of hypothyroidism are discussed in detail in a separate chapter.
Pulmonary System
Hypothyroid patients may have multiple ventilatory and respiratory abnormalities, including central and/or obstructive sleep apnea, CO2 retention, hypoxemia, increased alveolar-arterial (A-a) oxygenation gradients, and decreased CO2 diffusing capacity (DLCO) (48,49,50,51,52). Proposed mechanisms for these conditions include impaired hypoxic and hypercapnic ventilatory drives, upper airway obstruction from soft-tissue enlargement or goiter, respiratory muscle weakness, decreased
chest wall compliance, decreased lung compliance, increased capillary permeability and pleural effusions (43,53,54,55,56,57,58,59,60,61,62,63,64,65,66). Difficulty weaning hypothyroid patients from assisted ventilation is another associated complication (67). The pulmonary manifestations of hypothyroidism are discussed in detail in a separate chapter.
chest wall compliance, decreased lung compliance, increased capillary permeability and pleural effusions (43,53,54,55,56,57,58,59,60,61,62,63,64,65,66). Difficulty weaning hypothyroid patients from assisted ventilation is another associated complication (67). The pulmonary manifestations of hypothyroidism are discussed in detail in a separate chapter.
Infectious Complications
Increased susceptibility to infections of the respiratory tract, urinary tract, and skin have been reported in patients with hypothyroidism (68,69,70). Although not well understood, this propensity for infections may relate to alterations of respiratory function or cough, bladder dysfunction, impaired cutaneous blood flow, and abnormalities of circulating and tissue phagocytic cell function (68,69,70). While infection appears to be more common, animal studies suggest that hypothyroidism can impair the febrile response (71), and thereby possibly impede the recognition of some infections in hypothyroid patients.
Musculoskeletal System
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree