44.1
Introduction to eating disorders
Eating disorders (EDs) are psychiatric disorders associated with both physical and psychosocial morbidity, with the highest prevalence in young adult and adolescent women . This set of disorders presents a challenge for researchers and clinicians as social, psychological, and biological processes seem to contribute to their etiology and also render them particularly difficult to treat. The Diagnostic and Statistical Manual for Mental Health Disorders Fifth Edition (DSM-5) recognizes a number of EDs, including anorexia nervosa (AN), bulimia nervosa (BN), OSFED (other specified feeding or EDs), and BED (binge ED) .
44.1.1
General clinical features
AN and BN share a common core psychopathology associated with the overvaluation of shape and weight and a distinct drive for thinness . Whereas healthy individuals assess their self-worth, performance, and success based on a wide variety of domains, including relationships, parenting skills, work, or sporting ability, individuals with AN and BN focus mostly on their shape and weight . In the case of AN, these individuals restrict food intake to achieve a low body weight, often developing from a fear of being fat or a desire to be thin, accompanied by anxiety around body shape or weight . In the case of BN, individuals try to control their weight by restricting food intake, accompanied by binge eating and purging, using laxatives, through vomiting or the use of diuretics . In addition, both AN and BN patients often have a distorted view of their body image, often seeing themselves as “fat” even if at low or normal weight that may contribute to maintaining their ED behaviors . BED has recently been included in the DSM-5 as an ED in its own right and is characterized by binge eating episodes in the absence of purging behaviors .
OSFED in the DSM-5 category replaces a category formally called ED not otherwise specified in the DSM-IV that captures feeding or EDs of clinical severity that do not meet the diagnostic criteria for AN, BN, or BED (or feeding disorders, including avoidant/restrictive food intake disorder, pica, or rumination disorder). OSFED includes atypical AN and BN (limited frequency or duration of the disorder), BED (low frequency and limited duration), purging disorder (PD) (characterized by purging behaviors in the absence of fasting or binge eating), and night eating syndrome (NES) .
44.1.2
Anorexia nervosa
AN is a psychiatric condition characterized by concerns with body weight and shape, accompanied by weight loss or a severely low body weight achieved by restricting caloric intake or skipping meals or by compensatory methods, including vomiting or misuse of medication (including taking laxatives, diuretics, or slimming medications) . The DSM-5 defines the necessary criteria for the classification of AN as (1) a significantly low body weight in the context of age, sex, developmental trajectory, and physical health; (2) an intense fear of fatness that is maintained even when the individual is underweight; (3) an undue influence of body weight and shape on self-evaluation, which often is maintained despite low weight and the concerns of others. The DSM-5 defines two subtypes of AN, according to the methods employed to maintain low weight: (1) AN of the restricting type (AN-R), when the individual achieves and maintains a low weight simply by restricting caloric intake and (2) AN of the binge–purge type (AN-BP), if the individual engages in instances of binge eating and/or purging episodes (defined as vomiting or misuse of medication) to lose weight and compensate for caloric intake . AN has been reported in 0.2%–1% of adolescents and young adult women, and the teenage years are a particularly common time for the onset of this disorder . Of note, 5%–15% of individuals with AN are male.
44.1.2.1
Medical complications
The physical symptoms of AN are secondary to a state of malnutrition, and many are reversed with recovery from the ED, with the apparent exception of reduced bone mineral density (BMD) . The majority of these physical symptoms are dependent on both the severity and duration of the disorder and thus may vary between individuals .
Low BMD for age and secondary osteoporosis are common in AN associated with a significant increase in risk for bone fractures, which can lead to both pain and disability . Low body weight and lean mass, associated hypoestrogenemia (as indicated by the presence of amenorrhea and menstrual dysfunction) and other hormonal abnormalities negatively impact bone in this condition . Evidence suggests that weight gain and/or menstrual recovery (in those that are amenorrheic) do not always substantially increase BMD or reduce the risk of fractures, and long-lasting reductions in BMD and increases in fracture risk persist despite full recovery from AN , indicating that an adequate understanding of this condition is essential when considering possible therapies .
44.1.3
Bulimia nervosa
Individuals with BN exhibit excessive concern over weight and shape, and BN is characterized by recurrent episodes of binge eating followed by compensatory behaviors (e.g., vomiting and misuse of medication) in order to control body weight and shape . A low body weight is not a requirement for a diagnosis of BN.
The DSM-5 criteria for BN list the following: (1) engaging in recurring binge eating episodes, defined as the consumption of an unusually large amount of food in a short period of time while experiencing a sense of loss of control over the amount of food eaten (i.e., not being able to stop eating even if wanting to); (2) the binge eating episode is followed by compensatory behaviors to avoid gaining weight; compensatory behaviors are defined as vomiting, inappropriate use of medications (i.e., laxatives, diuretics, water pills, enemas, and diet pills), fasting, or exercising excessively; (3) binge eating episodes are followed by inappropriate compensatory behaviors that occur once a week for at least 3 months; (4) the individual places an undue influence on weight and shape on self-evaluation; and (5) this disturbance does not occur only during episodes of AN . This condition is seen in 1%–2% of older adolescents and young adult women .
44.1.3.1
Medical complications
In the case of BN, physical consequences may be minor unless there is a high frequency of purging, which may result in an electrolyte imbalance, decaying of teeth and a risk to cardiac function .
44.1.4
Binge eating disorder
The DSM-5 introduced BED as a distinct ED diagnosis. In DSM-5 an individual is diagnosed with BED if (1) in the absence of compensatory behaviors they engage in binge eating episodes, defined (similarly to BN), as consuming a large amount of food in a short period of time accompanied by a sense of loss of control over the amount of food eaten; (2) during these episodes the individual eats more quickly than usual until uncomfortably full, when not physically hungry, experiencing feelings of guilt, or embarrassment that often leads to eating in secret; (3) the disorder is associated with significant distress; and (4) these episodes occur at least once a week for a minimum of 3 months .
44.1.4.1
Medical complications
There is limited evidence regarding the physical consequences of BED that may include weight gain, and in the case of patients with obesity, comorbidities of obesity such as diabetes, hyperlipidemia, obstructive sleep apnea, polycystic ovary syndrome, asthma, and certain forms of cancer .
44.1.5
Other specified feeding or eating disorders
In DSM-5, “OSFED” include a mixture of disorders , including subthreshold EDs and EDs that do not fall within the categories of AN, BN, and BED . Examples of OSFED include atypical AN and BN (low frequency or limited duration), PD, and NES . OSFED is not limited to these examples and includes individuals with heterogeneous ED presentations.
44.1.6
Eating disorders and bone health
Both adolescents and adults with EDs can develop low bone density and increased fracture risk, with long and debilitating consequences. Current recommendations for the improvement of bone health are limited to weight gain and menstrual recovery with just a few pharmaceutical options available .
44.1.6.1
Bone health in anorexia nervosa
AN has been associated with low BMD, impaired bone structure, and an increased risk of bone fractures . Contributors to impaired bone health include low body weight, associated menstrual dysfunction, and other hormonal alterations . AN patients are seven times more likely to have bone fractures than age-matched healthy women , and in a community sample of adult women with AN, 93% and 38% had BMD 1 and 2.5 standard deviation (SD) below the population mean respectively, at one or more skeletal sites . Adolescents with AN are also at high risk for low BMD, with one study reporting that approximately 50% had BMD 1 SD below the mean at one or more skeletal sites . Furthermore, approximately 30% of adolescent girls and adult women with AN report sustaining a fracture . Of note, both subtypes of AN, the restricting subtype (AN-R) and the binge–purge subtype (AN-BP), are associated with reductions in spine BMD, and increased fracture risk, compared to controls . Onset of AN during adolescence is particularly worrisome because of its deleterious impact on peak bone mass accrual. In fact, studies suggest that onset of AN during adolescence is associated with lower BMD than when onset occurs in adult life despite a similar duration of illness or amenorrhea .
44.1.6.2
Bone health in bulimia nervosa
Several studies have now investigated bone health in BN with conflicting results. Whereas Newman and Halmi found no difference in BMD in patients with BN and healthy controls , Newton et al. reported that patients with BN had significantly lower BMD Z -scores at the lumbar spine in comparison to healthy controls . Due to the limited sample sizes in clinical studies and the lack of population-based studies investigating bone health in BN, it is not possible to estimate the prevalence of low bone density in individuals with BN. However, it is evident that this represents a population potentially at risk for low BMD and increased risk of fractures, justifying further investigation.
44.2
Assessment of bone outcomes in eating disorders, including the use of novel techniques
44.2.1
Assessment of areal bone density, hip structural analysis, trabecular bone score, and vertebral fracture analysis using dual-energy X-ray absorptiometry
The most common method used to assess bone health in EDs is DXA (dual-energy X-ray absorptiometry). DXA scanning allows assessment of bone area (BA), bone mineral content (BMC), and areal BMD (aBMD), which is affected by body size, with shorter individuals being reported to have artifactually low aBMD . This is particularly important to take into consideration in patients whose puberty has been delayed due to early onset of AN, resulting in shorter stature than expected for age . Bone mineral apparent density (BMAD) is a size-adjusted measure of BMD calculated using established formulas and may be used in such instances . There are also concerns regarding DXA BMD measurements being impacted by intra- versus extraosseous fat such that loss in BMD following weight loss may be underestimated and an increase in BMD following weight gain may be overestimated.
In both adults and adolescents with AN, low BMD at various sites does not always correlate with fracture occurrence . Bone structure and geometry can provide information beyond that provided by a DXA scan, and in addition to BMD, bone microarchitecture and its mechanical load distribution are important determinants of bone strength. However, DXA now allows reporting of hip structural analysis (HSA) that reflects the structural geometry of the proximal femur at specific locations (narrow neck, intertrochanteric region, and femoral shaft) . In AN, most HSA-derived parameters are impaired compared to controls . In addition, adult women with AN have decreased resistance to axial (cross sectional area (CSA)) and bending loads (Z) compared with controls . These differences persist after adjusting for lean mass.
Trabecular bone score (TBS) provides evidence of the bone texture and can also be reported from a DXA scan. It provides a textural index of gray level variations from one pixel to the adjusted pixels in the lumbar spine DXA image. TBS is related to three-dimensional (3D) characteristics of bone, including trabecular number and separation, and is not a direct measure of bone microarchitecture . TBS was found to be significantly lower in adolescents with AN compared to healthy controls and correlated with age, body mass index (BMI), BMD measurements of the lumbar spine and total body, BMAD, and BMAD Z -scores in AN .
Vertebral fracture assessment (VFA) is now possible on some DXA devices that allow lateral spine imaging. It is associated with lower radiation exposure compared to spine radiographs (≈42 μSv vs ≈97 μSv) and allows for simultaneous assessment of BMD and fracture risk. VFA has been scarcely used within the ED population. However, in one study of 68 adolescent AN patients who had VFA as part of a DXA scan, 5.9% were found to have a mild (Stage 1) vertebral fracture .
44.2.2
Assessment of volumetric bone mineral density, bone size and structure using high resolution peripheral quantitative computed tomography
The assessment of volumetric BMD (vBMD), bone size, and structure may explain fracture risk independent of aBMD and also minimize the influence of fat distribution on BMD assessment . The primary tools for assessing vBMD and bone structure are quantitative computed tomography (QCT) and high-resolution peripheral QCT (HR-pQCT). QCT allows assessment of both bone geometry and vBMD and has been reported to account for differences in bone strength in postmenopausal women, even when DXA showed no significant difference in aBMD . Furthermore, HR-pQCT allows assessment of bone microarchitecture. Finite element models of bone can be created from in vivo 3D QCT and HR-pQCT images to provide an estimation of bone strength.
At the distal radius, girls with AN have lower total and trabecular vBMD, lower cortical area and thickness, and increased cortical porosity and trabecular separation compared with controls, as assessed using HR-pQCT . Failure load and stiffness, estimated by microfinite element analysis (FEA), are 15% and 16% lower at the distal radius in adolescent girls with AN, indicative of reduced bone strength. This effect remained after adjusting for bone age, height, and radial aBMD . In addition to these changes, deficits in cortical thickness and trabecular number have been reported in adults with AN at the distal radius, with cortical deficits being related to the age of onset of the ED . Furthermore, flat-panel volume computed tomography (CT) can assess trabecular structure, including apparent bone volume fraction, apparent trabecular thickness, and apparent trabecular number, all of which have been found to be significantly lower at the distal radius in adult women with AN compared to healthy controls .
At the distal tibia, a weight-bearing site, adolescents with AN have greater cortical porosity, lower total and cortical vBMD, a lower cortical area, thickness, trabecular number and strength estimates in comparison to healthy controls. Within AN, strength estimates at the distal tibia were associated with aBMD, vBMD, bone size, and microarchitectural parameters measured by HR-pQCT . Future research should aim to also investigate failure load and stiffness using FEA at the distal tibia versus the distal radius in individuals with AN in order to compare the effect of AN on weight- and nonweight-bearing sites.
Milos et al. found significant differences in apparent trabecular bone fraction (BV/TV), apparent trabecular number, apparent trabecular thickness, and cortical thickness at the ultradistal radius, all indicators of bone strength, between adult women with AN and controls . In addition, HR-pQCT measurements of total and cortical vBMD and cortical thickness (but not trabecular measures) were associated with age at AN onset. These data suggest that a younger age at AN onset mostly affects cortical bone, specifically at the ultradistal radius. Milos et al. examined the impact of an increase in BMI in individuals with AN over a 2-year follow-up period on bone endpoints and reported an initial decrease in spine BMD at the 12-month follow-up visit followed by an increase to baseline by the 24-month follow-up visit. Changes in total and trabecular vBMD and cortical thickness at the ultradistal radius followed a similar pattern, suggesting that despite weight regain, bone regain at different locations may require varying periods of time .
Frølich et al. found an impairment in cortical thickness and estimated failure load, which were more pronounced at the tibia, a weight-bearing site, compared to the radius in adults with AN . Furthermore, weight-bearing exercise may influence cortical thickness at weight-bearing sites, with DiVasta et al. reporting that exercise effects on cortical BMC, cross-sectional area, and thickness Z -scores, measured by pQCT scanning, did not differ in adolescent girls with AN versus healthy adolescents . However, trabecular and cortical vBMD Z -scores differed between groups at any given exercise level. Thus exercise may impact the size of the cortex in AN.
Estimated vertebral strength, derived from integral vBMD values from QCT scanning, is lower in low-weight women with AN compared to controls, and intermediate in atypical AN . Both measures were associated positively with BMI and inversely with the duration of amenorrhea. Another study assessed vertebral bone texture using a low-dose single-section quantitative CT of the L4 vertebral body with use of a calibration phantom and reported altered bone texture in adult women with AN that was associated with lowest lifetime body weight and the duration of amenorrhea .
44.3
Factors related to the development of low bone density in patients with eating disorders
44.3.1
Changes in body composition and energy status
44.3.1.1
Low body mass index
It is evident that AN presents a significant risk factor for low BMD at all sites, whereas many studies investigating BMD in BN remain inconclusive. An apparent difference between these EDs is the severely low body weight and low BMI observed in both adolescents and adults with AN. A low BMI is an independent risk factor for low BMD at all sites , and evidence suggests that this damage is not fully reversible even when a healthy BMI is attained . Both low body weight and reduced lean body mass are important determinants of the deleterious bone outcomes in AN , and both the restricting (AN-R) and binge–purge subtypes (AN-BP) are associated with reduced spine BMD and increased fracture risk compared to controls .
An increase in BMI and menstrual recovery are important predictors of increases in BMD at all sites in AN, resulting in mean annual increases in BMD of 3.1% at the spine and 1.8% at the hip in adults . However, when AN occurs in adolescents, BMD following recovery from AN may not be comparable to the BMD of healthy controls because bone accrual rates remain suboptimal despite recovery . Thus adolescent onset AN is likely to be associated with lower peak bone mass acquisition that in turn predisposes these women to lower BMD throughout adult life .
Of note, some (but not all) studies have reported lower spine BMD in normal-weight BN patients compared to their healthy counterparts, suggesting that weight loss alone may not explain the harmful effects of an ED, specifically AN, on bone health . Limited research examining bone outcomes in BN and other EDs limits our current understanding of the effect of ED behaviors such as purging, binging, and misuse of medication, including laxatives and diuretics, on BMD in individuals with a healthy BMI.
44.3.1.2
Lower fat mass
Lower fat mass (particularly lower subcutaneous fat) may contribute to impaired bone outcomes in EDs. Fat mass is an indicator of energy stores, and subcutaneous fat is also a source of leptin secretion, a hormone with bone anabolic effects. Higher fat mass is associated with higher BMD at the anterior–posterior and lateral spine in adults , and with higher lumbar spine BMD in adolescents with AN .
44.3.1.3
Lower lean mass
Higher lean mass is protective of bone, likely because the pull of muscle of bone has bone anabolic effects . Lean mass correlates with BMD at multiple sites and also with measures of bone microarchitecture in adolescents with AN , and lean mass in combination with the duration of AN is reported to be among the strongest predictors of BMD at all skeletal sites in adult women .
44.3.1.4
Increased marrow adipose tissue
Recent studies have moved to assessing nontraditional fat stores in AN, including marrow adipose tissue (MAT) and cold-activated brown adipose tissue (BAT). The relationship between MAT and other fat depots is complex and is likely to moderate metabolic homeostasis, hematopoiesis, and osteogenesis . The complex relationship between osteoblasts and adipocytes, which arise from the same stromal progenitor stem cells within bone marrow, will likely provide an insight into the pathogenesis of increased fracture risk in both EDs and obesity.
The differentiation of this common stromal progenitor stem cell in bone marrow (and MAT) into either an osteoblast or adipocyte depends on the marrow energetic and hormonal milieu. MAT is higher in adult women with AN compared to controls and is associated with lower BMD measures . Recent studies indicate that a higher degree of bone marrow fatty acid saturation may impact BMD deleteriously in AN, given negative associations of marrow fat saturation with BMD in this group . Women with AN have higher total femoral marrow fat than controls, but marrow fat composition is comparable in the two groups.
44.3.1.5
Lower cold-activated brown adipose tissue
Women with AN have low cold-activated BAT that may be an adaptive mechanism to reduce energy expenditure in this state of energy deficit. Young women with higher BAT have higher BMD and lower preadipocyte factor-1 (Pref-1) (a negative regulator of osteoblastogenesis in the marrow) compared with women with lower BAT . Given that women with AN have higher Pref-1 levels than controls, which correlate inversely with bone density , BAT may be involved in the regulation of stem cell differentiation toward the bone lineage at the expense of adipogenesis .
44.3.1.6
Resting energy expenditure
Bone is an endocrine organ , and bone acquisition is believed to be closely linked to the regulation of glucose metabolism and energy expenditure. Because bone remodeling is energetically costly for the body, it is logical that it should be affected by the energy status of an individual . Thus states of low energy availability (either from reduced energy intake or increased energy expenditure or both) would be associated with low bone density because energy stores are preserved for the most essential of body functions, This is supported by the observation that individuals with AN demonstrate an association between energy status and bone mass acquisition .
Resting energy expenditure (REE) has been linked to bone remodeling, glucose homeostasis, and adipokines, highlighting the importance of preventing energy deficiency in order to limit hormonal alterations and disruptions in bone mineralization in AN . REE correlates positively with aBMD at most sites in AN patients, though in one study, these findings were specific to AN-R, but not AN-BP patients. The authors proposed that bone findings may have been confounded by body weight, age, and hormonal contraceptive use . Furthermore, in AN patients, REE has been reported to correlate positively with markers of bone formation [osteocalcin (OC) and N-terminal propeptide of type 1 collagen (P1NP)] and negatively with the marker of bone resorption [C-telopeptide (CTX)]. This suggests that energy status is an important determinant of bone turnover in AN patients. Finally, a higher REE/fat-free mass ratio has been related to a higher metabolic rate in low-body-weight individuals, which could be explained by a lower fat-free mass and a greater proportion of tissues with a high-metabolic rate .
44.3.2
Changes in macro- and micronutrients concentration
44.3.2.1
Macronutrient concentration
Adolescents and adults with EDs have altered nutritional intake, either leading to lower fat, carbohydrate, and protein intake, as in the case of the severe caloric restriction of AN, or sporadic binge-eating in BN, with evidence suggesting that carbohydrate craving triggers binge eating ; no evidence has been found for chronic energy deprivation or malnutrition in BN . In AN, lower fat intake is associated with lower fat mass and a resulting lower REE, likely an adaptive mechanism to preserve energy for vital functions. Individuals with AN have similar energy expenditure as constitutionally lean individuals, despite having lower energy intake . Although macronutrient intake has not been directly associated with BMD in EDs, when adolescent girls with AN were followed over a 6–12-month period, BMI at follow-up was associated positively with percentage of total calories obtained from fat, including monounsaturated and polyunsaturated fatty acids at 6 or 12 months, and inversely with the percentage of total calories obtained from carbohydrates and proteins . With BMI known to be the strongest predictor of recovery of bone mass in EDs , macronutrients may have an indirect effect on bone through their effect on BMI.
44.3.2.2
Micronutrient intake
As discussed earlier, the intake of fat, including saturated and unsaturated fat, is typically lower in AN compared to healthy controls. Furthermore, individuals with AN typically have a higher intake of soluble and insoluble fiber, oxalates and phytates , which could reduce the absorption of other nutrients. When 30 women with AN completed a 1-month diet history alongside an age-matched group of healthy controls, over half of the women with AN did not meet the recommended dietary allowance for vitamin D, calcium, folate, vitamin B12, zinc, magnesium, and copper . Low calcium levels have been associated with hypogonadal states known to affect bone metabolism, and the homeostasis of calcium supply and renewal may be disrupted in AN due to long-term malnutrition . Further, optimal vitamin D intake is necessary for optimal calcium absorption, and Vitamin D receptors are also closely linked to osteoblast function . However, as with macronutrients, specific micronutrients have not been directly linked to a reduction in BMD in AN. Vitamin intake from dietary supplements, including vitamin D and calcium, is often higher in AN compared to healthy controls, possibly due to recommendations from clinicians and increased education regarding the risk of low BMD from malnutrition in AN. One study by Giollo et al. found that hypovitaminosis D counteracts the efficacy of weight restoration in adults with AN, likely because of an increase in bone resorption mediated by secondary hyperparathyroidism . Thus while vitamin D or calcium deficiency typically does not contribute to low BMD in AN, administration of vitamin D and calcium supplements should be recommended in those with low baseline levels of vitamin D, as these micronutrients may mediate the effect of weight gain on BMD.
44.3.3
Excessive exercising
The positive effects of exercise on bone accrual and bone strength, and the protective effects of exercise on fracture risk, have been well documented in healthy individuals . However, the effect of exercise on bone health in EDs is less certain. Weight-bearing exercise is typically considered to be protective to bone mass ; however, high-intensity exercise may worsen the energy deficit state in AN and is a risk factor for fractures.
Many definitions exist of excessive exercise, centering on the concept of high-intensity exercise that goes beyond that required for health, and may even be harmful. A recent review of the literature has suggested that three dimensions of excessive exercise are important to consider, including the frequency and volume of exercise, obligatory exercise, and motivation for exercise . Competitive sports and high-intensity exercise may precede dieting in as many as 50% of the ED patients , and excessive exercise is one of the strongest predictors of poor outcomes in ED patients .
Although there is limited evidence for the role of exercise (or excessive exercise) in the relationship between EDs and bone health, recently published guidelines on the subject suggest that exercise of any form should be avoided in underweight individuals with an ED in order to optimize weight gain and protect against fractures . However, one study has reported that exercise is protective against loss of BMD at weight-bearing sites in women with both AN and BN , although distinctions between the type of exercise and the extent to which this exercise is “excessive” are lacking.
44.3.4
Hormonal changes
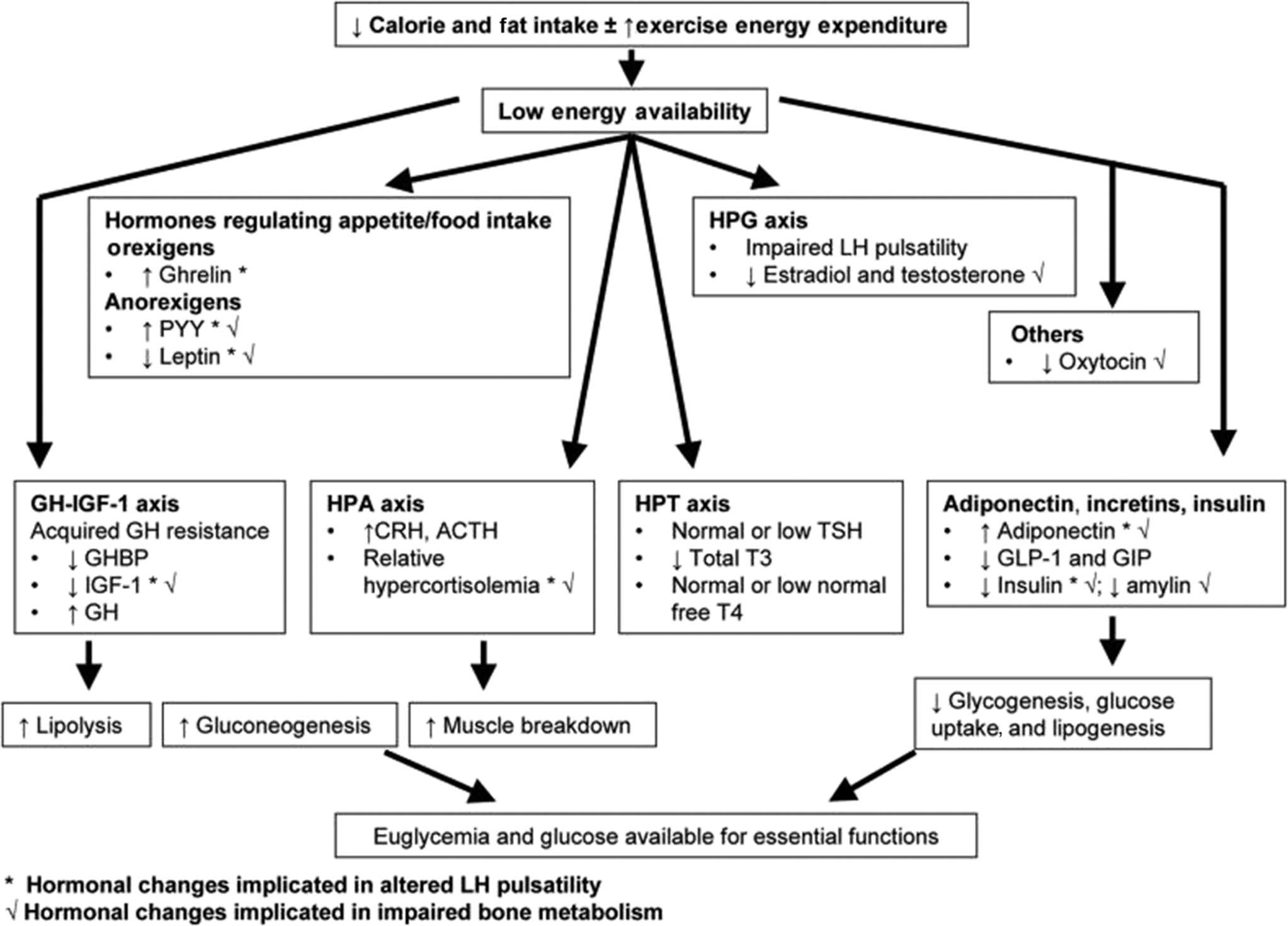
In addition to weight loss, bone is affected by the various neuroendocrine alterations observed in women with EDs ( Fig. 44.1 ).
44.3.4.1
Hypothalamic–pituitary–gonadal axis
Amenorrhea has now been removed from the revised DSM-5 criteria for the diagnosis of AN; however, hypothalamic amenorrhea is still common in adolescents and adult women with AN. Suppression of the hypothalamic–pituitary–gonadal (HPG) axis preserves energy in a state of undernutrition by preventing energy being diverted toward reproduction and maintenance of a growing fetus . As a result, serum levels of estradiol and testosterone are lower in adults and adolescents with AN than in healthy controls. Although AN is commonly associated with hypothalamic amenorrhea, AN and EDs in general are associated with a spectrum of menstrual dysfunction, including oligomenorrhea , anovulatory eumenorrhea, and luteal phase defects. Amenorrhea in EDs is associated with low energy availability, low fat mass, and altered secretion of neuroendocrine hormones that may also impact gonadotrophin secretion. Hormones such as insulin-like growth factor 1 (IGF-1) and leptin, commonly associated with stimulation of the HPG axis, are decreased in AN . Similarly, hormones such as cortisol (discussed next) and ghrelin have an inhibitory effect on the HPG axis and are increased in AN .
In AN, lower estradiol levels, later age of menarche, and a longer duration of amenorrhea predict lower BMD . Estrogen is antiresorptive and reduces osteoclast activity by decreasing the secretion of receptor activator of nuclear factor-κB ligand (RANKL) and inflammatory cytokines and increasing the secretion of osteoprotegerin (OPG), a cytokine receptor of the tumor necrosis factor receptor . Estrogen may also increase bone formation by inhibiting sclerostin and Pref-1, which otherwise inhibit osteoblast differentiation . However, oral estrogen administration as ethinyl estradiol (with a progestogen as in a combined oral contraceptive pill) does not improve BMD in adults and adolescents with AN . This lack of efficacy of oral ethinyl estradiol in improving BMD in AN has been attributed to (1) the suppressive effect of the medication on hepatic IGF-1 secretion because of its hepatic first-pass effects, as well as (2) the nonphysiologic form of estrogen used in these oral preparations (ethinyl estradiol as opposed to 17-β estradiol). Consistent with this, an 18-month study in adolescents demonstrated significant increases in spine and hip BMD in girls with AN randomized to physiologic estrogen replacement as the 100 mcg 17-β estradiol patch (given with cyclic progesterone) compared to placebo .
Testosterone can impact bone through its aromatization to estradiol, and also directly through androgen receptors on bone. Low testosterone levels in AN are associated with low BMD, and increases in testosterone with weight regain are an important predictor of increases in BMD in adolescents with AN . Adult women with AN similarly have lower testosterone levels than normal-weight controls, associated with lower BMD measures . However, administration of transdermal testosterone (to reach testosterone levels within the upper half of normal range for adult women) does not increase BMD in adult women with AN . In contrast, another ovarian hormone, dehydroepiandrosterone (DHEA), was reported to improve femoral cross-sectional BA, section modulus, and cortical thickness (measured by HSA) and maintain BMD Z -scores in young women with AN when given with oral estrogen–progesterone combination pills . However, other studies have reported no differences in DHEA levels in girls with AN versus controls . Bone resorption is higher in adult amenorrheic women with AN than in postmenopausal women known to also have low serum estrogen levels , which suggests that low levels of sex hormones alone cannot explain the changes in bone turnover observed in AN.
44.3.4.2
Hypothalamic–pituitary–adrenal axis
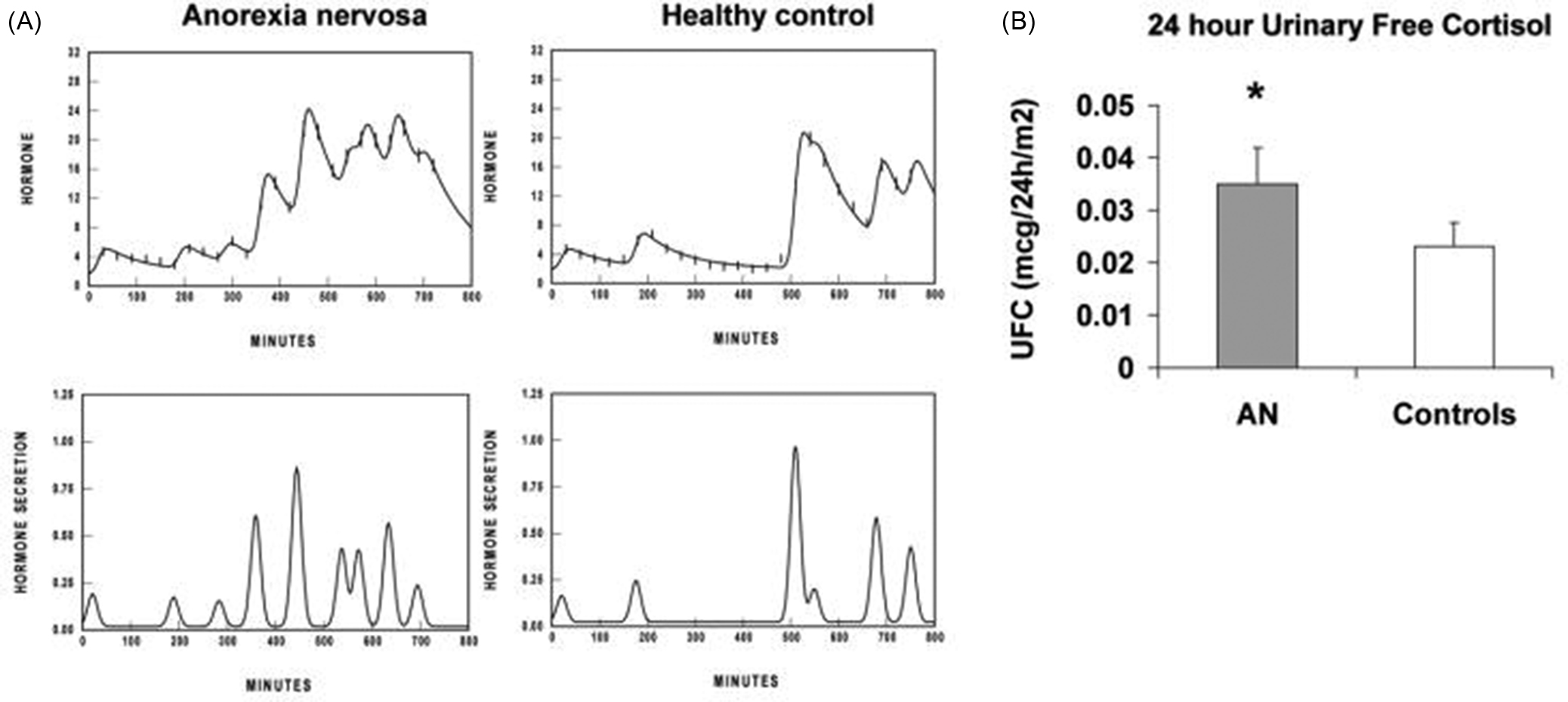
AN is associated with relative hypercortisolemia in both adults and adolescents ( Fig. 44.2 ). However, in AN, hypercortisolemia is not associated with Cushingoid features, and the cortisol level rarely exceeds twice the upper limit of the normal range . Hypercortisolemia inhibits bone formation, has an inhibitory effect on the HPG and growth hormone (GH)–IGF-1 axes, impairs calcium absorption from the gut and the renal handling of calcium, inhibits OPG, and increases RANKL secretion. In AN the increase in cortisol is believed to be an adaptive mechanism to maintain euglycemia in a state of malnutrition and low energy availability, as the highest cortisol levels are observed in those with the lowest BMI, fat mass, and fasting glucose and insulin levels . Recent research has suggested that hypercortisolemia in AN is a state-dependant phenomenon, as an enhanced cortisol awakening response was observed in acute but not weight-restored adult AN patients . Hypercortisolemia has been widely linked to bone loss in those with Cushing’s syndrome and likely contributes to low BMD in AN as suggested by inverse associations with levels of bone formation markers . Data are conflicting regarding the effect of cortisol on weight and body composition in AN, both of which can impact BMD . In one study, higher baseline cortisol levels in adolescents with AN were associated with greater increases in fat mass and with menses resumption . In contrast, increased corticotrophin-releasing hormone (CRH) secretion in AN is reported to be anorexigenic and contributes to the severity of weight loss in AN, independent of BMI . In addition, increased ghrelin secretion in AN may stimulate increased secretion of CRH, adrenocorticotropic hormone, and cortisol . Relative hypercortisolemia in AN has not been found to contribute to a Cushingoid state (in contrast to pathological hypercortisolemia), and thus no pharmacological approaches have been investigated to address hypercortisolemia in AN.
44.3.4.3
Hypothalamic–pituitary–thyroid axis
Changes in the hypothalamic–pituitary–thyroid axis in AN are associated closely with malnutrition and weight loss and are commonly treated indirectly through weight gain. Levels of triiodothyronine (total T3) are low in AN, consistent with a low REE, which enables an individual to conserve energy for vital functions. Lower T3 levels are associated with lower leptin and higher ghrelin and cortisol levels in AN . Free thyroxine (T4) levels vary depending on the severity of AN, while thyroid-stimulating hormone levels are typically normal or low normal .
44.3.4.4
Growth hormone–insulin-like growth factor-1 axis
AN is associated with a nutritionally acquired GH resistance, with lower IGF-1, yet higher GH concentrations than observed in controls. The state of GH resistance is consequent to reduced expression of the GH receptor, as evidenced by reduced circulating levels of GH-binding protein, the cleaved extracellular component of the GH receptor . Higher GH concentrations are associated with lower BMI, fat mass, and IGF-1 levels, and higher FGF-21 (fibroblast growth factor 21), a hormone produced in the liver that may play a role in the mechanism of GH resistance in AN . The higher GH concentrations are overall believed to a consequence of lower glucose and IGF-1 levels (from reduced negative feedback), and higher FGF-21 and ghrelin levels (a GH secretagogue). In AN, as with hypercortisolemia, higher GH concentrations are believed to be adaptive, as increased GH promotes gluconeogenesis by increasing substrate availability through lipolysis. Weight gain leads to a normalization of GH secretion and GH-binding protein concentrations, consistent with the hypotheses that GH resistance is an adaptation closely linked to the individual’s nutritional status .
Lower IGF-1 levels correlate with lower levels of bone formation markers and lower BMD, and endogenous IGF-1 levels predict measures of bone microarchitecture independent of BMI in women with AN . Administration of recombinant human IGF-1 (rhIGF-1) increases levels of bone formation markers in adolescents and adults and increases BMD in adults with AN when given with a combined oral estrogen–progesterone pill . Further, FGF-21 levels are inversely associated with trabecular number and estimates of radial bone strength (stiffness and failure to load) in AN .
44.3.4.5
Appetite-regulating hormones
Appetite-regulating hormones such as leptin (an anorexigenic hormone), ghrelin (orexigenic), and peptide YY (PYY; anorexigenic), that are known to have an impact on bone, are reported to be altered in AN. Leptin is reduced in both AN and BN but higher in BED than healthy controls . As leptin was reduced in both underweight AN and normal-weight BN, but not in overweight BED, factors other than BMI must play a role in the altered leptin levels among EDs . Furthermore, ghrelin levels are higher in AN versus controls , and in AN-BP versus AN-R , although this finding has not been replicated in later research . A positive association has been reported between fasting concentrations of ghrelin and the frequency of purging in bulimic women . PYY is increased in both AN and BN, with levels remaining elevated in both groups following inpatient therapy , and also in normal-weight BN abstinent from pathological eating behavior for 1 month in comparison to healthy controls . This suggests that increased PYY may be a long-lasting consequence of both AN and BN. Whereas the increase in ghrelin and decrease in leptin are likely adaptive in AN to optimize caloric intake by increasing orexigenic and decreasing anorexigenic stimuli, this does not explain the higher PYY levels (which is anorexigenic) in AN.
Leptin and ghrelin are believed to be bone anabolic, whereas PYY inhibits osteoblast differentiation. In healthy adolescents, higher serum ghrelin concentrations predict higher BMD. However, this association is not observed in AN, suggesting a possible resistance to ghrelin in AN . Lower leptin and higher PYY levels are associated with lower levels of bone turnover markers and lower BMD . The relationship between BMD and ghrelin, leptin and PYY has not yet been investigated in BN participants.
44.3.4.6
Other hormones and neurotransmitters
Oxytocin (OT) is a hypothalamic hormone released from the pituitary gland that has previously been associated with lactation, parturition, and pair bonding in rodent models . OT is now known to have both anorexigenic and bone anabolic effects and is involved in energy homeostasis . Lower oxytocin levels in AN are associated with lower BMD and low fat mass, possibly mediated via estrogen. Lower estradiol levels in AN may impair oxytocin secretion by osteoblasts, another mechanism whereby bone metabolism may be impaired in AN .
Serotonin (5-HT) receptors are found on osteoblasts, osteoclasts, and osteocytes , and an inverse relationship is reported between serum serotonin levels and femoral neck, total, and trabecular vBMD in healthy women . AN patients are known to suffer from serotonergic hyperactivity associated with dysphoric mood linked to restrictive eating behavior. Decreased serotonin levels in AN may be consequent to a limitation of carbohydrate intake, and low central serotonin levels in BN participants are associated with blunted satiety responses to food. In a cross-sectional analysis of serum serotonin, BMD, and bone metabolism markers, a negative relationship was noted between serum serotonin and bone turnover markers in individuals with AN , with the relationship between serotonin and bone health in BN not yet investigated, suggesting that this warrants further study. Finally, longer use of selective serotonin reuptake inhibitors in AN has been associated with lower BMD measures, even after controlling for duration of disease and duration of amenorrhea .
44.3.5
Impact on surrogate markers of bone turnover
Surrogate (or biochemical) markers of bone turnover provide evidence for the rate of bone formation and bone resorption, indicating an overall rate of bone turnover, which can be associated with BMD at appendicular and axial sites . The kinetics of bone loss in EDs, specifically AN, is characterized by intense and early bone loss, with demineralization of bone detected as early as 6–12 months after disease onset , and BMD Z -scores of <−2 detected as early as 12 months following diagnosis of AN . Surrogate markers of bone turnover can detect the earliest changes in bone metabolism prior to the onset of osteoporosis. Commonly reported bone formation markers include OC, bone-specific alkaline phosphatase (BSAP), and P1NP. Commonly reported bone resorption markers include deoxypyridinoline (DPYRX), CTX, and N-telopeptide (NTX). Adolescents with AN have lower levels of biochemical markers of both bone formation and resorption indicating a coupled decrease in bone turnover. This is in contrast to the increased bone resorption typically expected in conditions of estrogen deficiency. Conversely, adult women with AN have decreased bone formation and increased bone resorption markers (consistent with the state of estrogen deficiency), indicating an uncoupling of bone turnover, associated with reductions in BMD . Decreased bone formation in both adults and adolescents with AN is likely a consequence of low levels of IGF-1, leptin and oxytocin, and high levels of cortisol and PYY.
The system of RANKL/RANK/OPG might play an important role in osteoclast differentiation, activation, and action . OPG and soluble RANK ligand (sRANKL) levels and their ratio provide evidence for the ongoing drive for bone resorption. RANKL is secreted by stromal precursor cells and osteoblasts, and these cells also secrete OPG, the soluble decoy receptor for RANKL . RANK is expressed on both osteoclasts and osteoclast precursors, and when RANKL binds to RANK, osteoclast activation reduces osteoclast apoptosis, thus increasing bone resorption. OPG, in contrast, by binding to RANKL prevents it from binding to RANK and thus reduces osteoclast activation and function and increases osteoclast apoptosis, leading to decreased bone resorption. Therefore the lower the ratio of OPG to sRANKL, the greater the drive for bone resorption. Transforming growth factor β (TGF-β1), a multifactorial cytokine, correlates positively with the OPG/sRANKL ratio. In AN, OPG and sRANKL levels are elevated, but the ratio of OPG to sRANKL is reduced . TGF-β1 secretion is reduced in AN, which may compromise the mechanism compensating for bone remodeling in this population . Further, estrogen deficiency can result in a lowering of this ratio and likely drives the increased bone resorption state observed in amenorrheic adults with AN. However, it is unclear why bone resorption is reduced in adolescents with AN. Of note, omentin-1, secreted by visceral adipose tissue, is increased in girls with AN and has recently been suggested to exert a negative effect on bone remodeling , independent of menstrual status. This effect is greater in younger, premenarcheal girls , and may explain the reduced bone turnover state in adolescents with AN. Data are currently lacking on omentin-1 levels in adult women with AN. No studies to date have linked biochemical markers of bone turnover in EDs with fracture occurrence.
44.4
Recommendations for the management of low bone density in eating disorders
44.4.1
Weight gain and recovery of bone mineral density in anorexia nervosa
Weight gain and menstrual recovery are the strongest predictors of increases in BMD in AN . However, numerous studies suggest that there may be long-term consequences relating to low BMD in individuals with AN, particularly when it onsets in the adolescent years and leads to a lower peak bone mass . For this reason, identification of low BMD at an early stage of an ED and treatments to optimize bone accrual in patients with EDs are of critical importance. Although weight gain and menstrual recovery increase BMD, significant deficits persist compared to healthy controls at the hip, femoral neck, and spine . As weight gain is linked to increased intake of macronutrients and micronutrients such as calcium, vitamin D, and vitamin K , disentangling the independent effects of increased BMI versus nutritional status on BMD in EDs is of interest. A better understanding of these relationships is necessary to effectively treat persistently underweight patients.
Biochemical markers of bone turnover increase in adolescents with AN during weight gain, and this increase predicts a significant increase in BMD 6-months later . In 35 AN patients (mean age 20.6±5.8 years), BMD was measured by QCT at treatment start (T0) and following weight recovery and regular menses (T1). A positive relationship was seen between final BMI and final BMD at the lumbar spine (L4) when the period (T1-T0) was more than 11 months, but not when the time period was ≤11 months . These data are promising and indicate that weight gain and menstrual recovery are strong predictors of increased BMD. However, data are lacking regarding the effects of weight gain and menstrual recovery in adolescents on bone geometry, microarchitecture, and bone strength estimates, known to be strong predictors of fracture risk.
44.4.2
Nutritional supplementation
44.4.2.1
Calcium
In women with AN, calcium homeostasis may be disrupted by prolonged malnutrition . However, results are conflicting regarding calcium metabolism in ED, with several studies suggesting that individuals with AN are not calcium or vitamin D deficient . Calcium supplements are commonly prescribed to individuals with AN in order to encourage nutritional rehabilitation; however, no increase in BMD was observed in adolescent girls with AN receiving calcium supplementation . Furthermore, a metaanalysis found no association between calcium intake and fracture risk in healthy adults . As individuals with AN are often not calcium deficient because of intake of calcium supplements, the effect of calcium supplementation versus calcium intake from food sources on BMD should be of particular interest for future investigation in patients with EDs.
44.4.2.2
Vitamin D
Vitamin D supplements have not been found to increase BMD in individuals with EDs to the level of healthy controls . However, there is a positive correlation between serum 25-hydroxy-vitamin D below 50 nmol/L and spine BMD Z -scores in adult women with AN, with increased alkaline phosphatase levels suggesting an adaptive osteoblastic reserve . Furthermore, supplementation of vitamin D3 (0.5 μg/day) did stabilize BMD in adult women with AN, suggesting that vitamin D3 should be prescribed in the early stages of EDs to prevent bone loss .
44.4.3
Pharmacological therapies for osteoporosis in eating disorders
44.4.3.1
Bisphosphonates
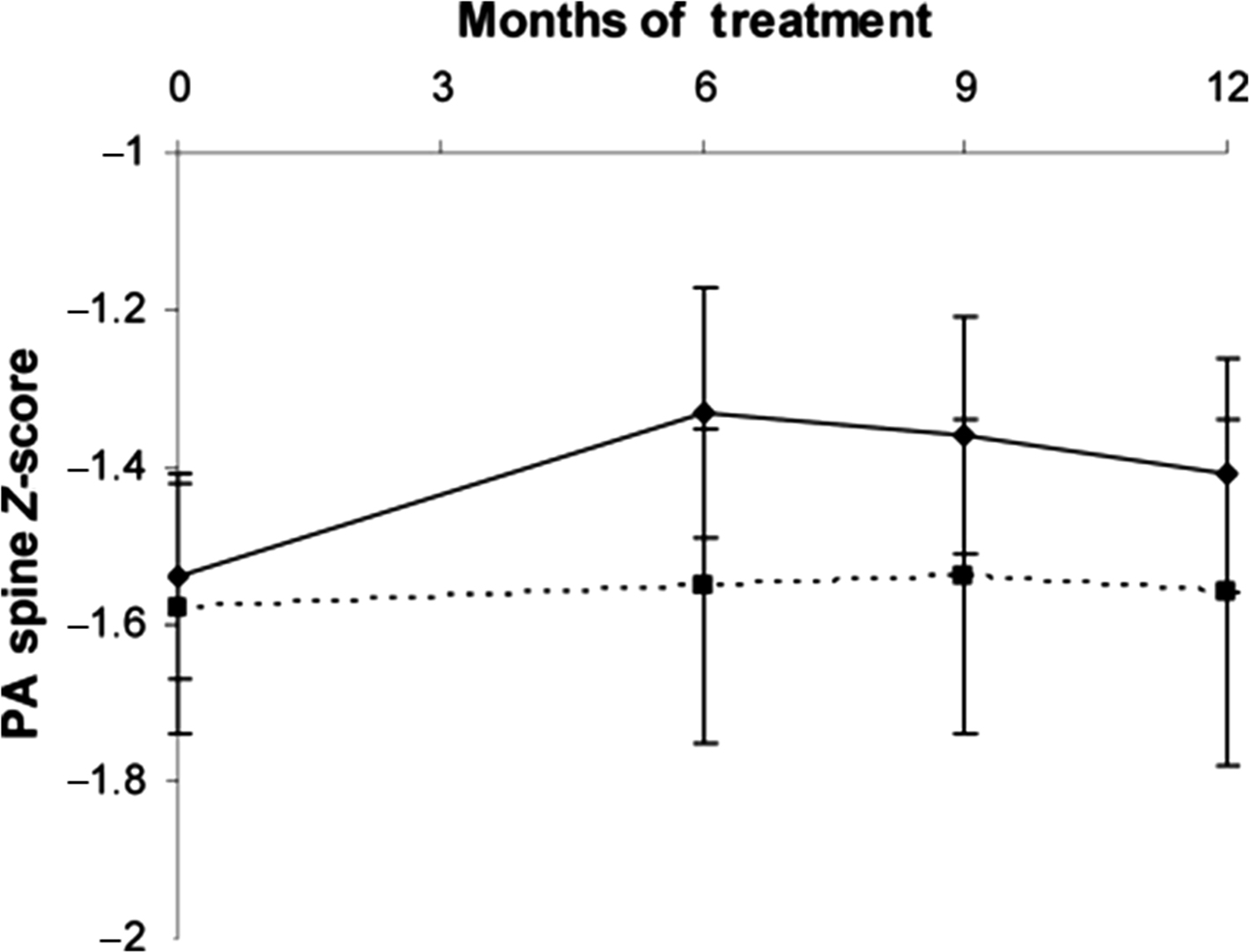
Bisphosphonates and teriparatide (TPT) are approved for the treatment of postmenopausal osteoporosis , and a few studies have examined the effect of these drugs on bone endpoints in AN. In one study of 77 adult women with AN, 1-year treatment using risedronate decreased CTX, a bone resorption marker, by 41%, increased posteroanterior spine BMD by 3.2%, and total hip BMD, by 1.9% ( Fig. 44.3 ). In contrast, a randomized controlled trial of alendronate versus placebo in adolescents with AN found no effect of alendronate at the spine compared to placebo, though a small positive effect was noted at the femoral neck . The lack of effect observed in adolescents with AN could be because (1) bisphosphonates act by reducing bone turnover, and bone turnover is typically suppressed in adolescents with AN (in contrast to adults, who have increased levels of bone resorption markers), or (2) because girls in both trial arms gained a significant amount of weight (13.5% for the intervention group vs 16.2% in the control group). With weight gain known to be the strongest predictor of recovery of bone mass in EDs, it is possible that the effect of weight gain was greater than the effect of bisphosphonate therapy on BMD, overpowering the detectable response to alendronate in this trial.