OSTEOPETROSIS
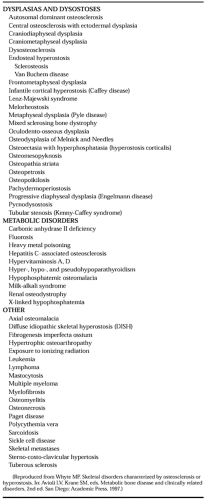
Osteopetrosis (marble bone disease) is one of many disorders that cause high bone mass (Table 66-1).6 Two principal forms are well characterized: an autosomal dominant (benign) type with few or no symptoms, and an autosomal recessive (malignant) type that is typically fatal during the first decade of life if untreated.8,9 Both of these forms of osteopetrosis have been genetically mapped,10,11 but the gene defects are partly known. An intermediate form of osteopetrosis also exists; it is inherited as an autosomal recessive trait and presents during childhood with some of the clinical manifestations of the malignant type, but its impact on life expectancy is unclear.12 Also, an autosomal recessive syndrome of osteopetrosis with renal tubular acidosis and cerebral calcification is seen; this form is due to an inborn error of metabolism characterized by deficiency of the carbonic anhydrase II (CA II) isoenzyme.13 At least nine forms of osteopetrosis are found in humans; most have a genetic basis.8,9,14
All forms of osteopetrosis in humans result from a failure of osteoclasts to resorb skeletal tissue, including the cartilage deposited during endochondral bone formation (primary spongiosa).15 The precise cause of osteoclast malfunction is understood only for CA II deficiency, for which several mutations in the CA II gene have been characterized,13 and for a subset of patients with malignant osteopetrosis who have defects in a gene that encodes a vacuolar proton pump.13a A considerable variety of defects in osteoclast formation and function will likely be found to explain these clinically and genetically heterogeneous conditions,8,9,15,16 for which animal models increasingly provide insight concerning potential etiology and pathogenesis.17,18
In the malignant form of osteopetrosis, symptoms begin during infancy.19 Often, an early observation is nasal stuffiness attributable to malformation of paranasal and mastoid sinuses. Subsequently, patients fail to thrive and often develop palsies of the facial, optic, or oculomotor nerves from compression by narrow cranial foramina; delayed dentition; bone fragility; and infection with spontaneous bruising and bleeding secondary to myelophthisic anemia with extramedullary hematopoiesis.8,9
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree