PEARLS
❖ Thirty percent of all geriatric patients/clients consult their physicians because of musculoskeletal problems.
❖ Therapists need to assess the cause of strength declines (eg, neuromuscular, cardiovascular, joint swelling, joint changes) and treat the strength decrease accordingly.
❖ Treatment suggestions for flexibility decrements in older adults are to heat the muscle, gently stretch the muscle, reinforce the stretch by doing functional activities, and cool the muscle down in the lengthened position.
❖ Normal changes of the spine include less flexibility in the soft tissues, decreased mineralization of bones, osteophyte formation, and disc space narrowing.
❖ Osteoporosis is no longer considered an inevitable consequence of aging.
❖ Osteopenia refers to metabolic bone diseases that are characterized by x-ray findings of a subnormal amount of mineralized bone mass.
❖ Aging causes a decrease in motion of almost all of the body joints. Nevertheless, the older person can maintain independence. Osteoporosis, arthritis, fractures, and many other pathologies respond favorably to exercise and rehabilitation programs.
Approximately 30% of all geriatric patients consult their physicians because of musculoskeletal problems.1 Therefore, it appears that orthopedics are a primary concern to geriatric therapists working with older adults. This chapter explores the changes with age in the musculoskeletal system. Pathologies specific to an older population are discussed. Then, a joint-by-joint approach is taken that examines the evaluation and treatment of orthopedic conditions in older adults.
STRENGTH
Numerous studies cite the loss of strength with age.2–4 The greatest loss of strength appears to be related to the selective loss of type II muscle fibers, which is thoroughly discussed in Chapter 3 of this text. Other variables can lead to strength loss. Sedentary lifestyle and lower levels of physical activity certainly head the top of this list.4 A decrease in cardiovascular endurance results in less stamina even during activities of daily living. This sets the stage for progressive loss in overall strength. Poor nutrition can change the metabolic efficiency of energy exchange at the level of the sarcolemma. A decrease in activity also leads to a diminished neuromuscular connection whereby transmission of nerve impulses to the muscle is slowed and the strength of the impulse lessened. Inhibition of muscle contraction is the consequence of the presence of edema, often seen in older adults with arthritic changes or injury in the joints.5 All of these variables will lead to a loss in overall muscular contraction strength. The clinical implications of these changes are that increasing activity could potentially reverse these strength changes. It has been demonstrated that greater time spent in light-intensity activity and lower sedentary times were associated with lower body mass index. These results are consistent with the hypothesis that replacing sedentary activities with light-intensity activities could lead to lower body mass index levels and obesity prevalence and higher levels of strength and endurance among the population of older adults.4 Some other hypothetical examples might be as follows5:
❖ If the decrease in strength is due to cardiovascular inefficiency leading to poor nutrient exchange, then an increase in activity level above rest would increase blood flow to the muscle and positively affect the health of the muscle tissue.
❖ If the loss of strength is due to a decrease in the efficiency of the neuromuscular junction contact, exercise has been shown to improve nerve conduction velocities, reaction times, and strength of muscle contraction.4
❖ If the decrease in strength is due to swelling (ie, reflex inhibition due to joint distention), then the swelling and subsequent strength loss can be alleviated by using modalities and anti-inflammatory medication prior to joint strength training.
Other major reasons for the decline in strength with age are pathological in nature, all of which appear to be more prevalent in older adults. An example of this is polymyalgia rheumatica, a systemic inflammatory disease of multiple joints that causes swelling, pain, and weakness.6 Systemic rheumatologic problems such as rheumatoid arthritis (RA) and lupus, like polymyalgia rheumatica, will diminish activity level secondary to pain and inflexibility and lead to a progressive loss in muscular strength. Parkinson disease and cerebrovascular accidents, as well as other neurologic pathologies, can result in strength loss because of tone changes and the quality of muscle contraction. The presence of underlying pathology in addition to normal changes in muscle strength with age should be considered in the evaluation and intervention of older individuals. See Appendix A for evidence-based evaluation and treatment ideas.
FLEXIBILITY
Another major area of function change with age is flexibility. As a person ages, the muscles become more rigid and tend to become less flexible. There is a higher proportion of type I muscle fibers, making the muscle a stabilizer instead of the fast-reacting muscle.7 There is also a decrease in elastin and an increase in collagen of the muscle tissue, further affecting the flexibility of muscle tissue (see Chapter 3).
In addition to these changes in muscle tissue, all connective tissues are affected by changes in elastin and collagen as described in detail in Chapter 3. The cartilage breaks down, restricting joint mobility. Tendons and ligaments become more rigid and less resilient to length changes, often resulting in injury. Flexibility into extension is most often lost in older adults.8,9 Postural changes from kyphosis of the thoracic spine lead to flexed positions of all of the lower extremity joints, which may result in irreversible soft tissue contractures if not attended to by the therapist. The presence of contractures requires special consideration in older persons. To get the best results, prolonged static stretching preceded by a heat modality is often needed to restore flexibility of collagenous tissue. Functional activities that incorporate elongated muscle positions are also helpful in regaining flexibility.9
It must be recognized that once a contracture occurs in older adults, it takes longer to achieve the benefits of a stretching program. The prevention of contractures in the first place is the best mode of intervention. Encouraging extension-strengthening exercises, positioning to facilitate extension, postural and balance exercises, proper nutrition, and hydration will help to establish healthy and flexible muscle tissue in the older adult. The key phrase here is “extension equals function.”8 See Appendix B for evidence-based evaluation and treatment ideas.
Posture
The third area of orthopedic functional change is posture. The classic “senile posture,” which is flexed, is certainly not an inevitable consequence of aging. However, in the presence of osteoporosis, compression wedge fractures of the thoracic vertebrae and compression fractures in the lumbar vertebrae result in characteristic postural changes. As note d in Figure 11-1, normal posture, with a plumb line running from the ear to the ankle, should fall through the following:
❖ The middle of the earlobe
❖ The middle of the acromion process
❖ The middle of the greater trochanter
❖ Posterior to the patella but anterior to the center of the knee joint
❖ Slightly anterior to the lateral malleolus
The most common posture changes with age, as depicted in Figure 11-2, include a forward head, rounded shoulders, decreased lumbar lordosis, and increased flexion in the hips and knees.9 There are some variations in the way in which posture is evaluated; as discussed in Chapter 9 with progressive postural changes, modification of postural status is often more easily assessed using the middle of the lateral malleolus as the starting point and going up the kinetic chain. Treatment for postural changes in older adults is to concentrate on extension throughout the kinetic chain. Stretching and flexibility exercises should be used for any of the body parts that have deviated from the norm. Strengthening of extensors and work on balance activities are very important components to a postural intervention program. The key to maintaining posture is prevention, prevention, prevention. The key to any exercise program is extension, extension, extension.8–10
After reviewing strength, flexibility, and posture changes with age, it is important to note that there are several musculoskeletal orthopedic pathologies that are extremely prevalent in older adults.
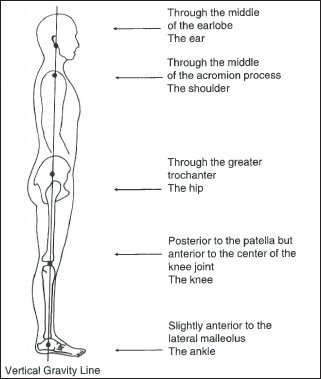
Figure 11-1. Proper posture shown with a vertical gravity line. (Reprinted with permission from Lewis CB, Bottomley JM. Musculoskeletal changes with age. In: Lewis CB, ed. Aging: The Health Care Challenge. Philadelphia, PA: FA Davis; 1990.)
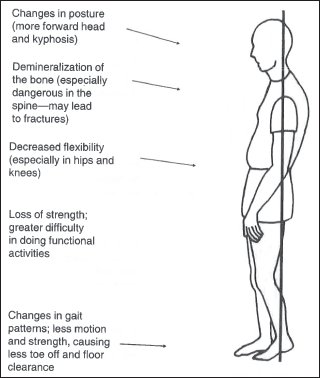
Figure 11-2. Postural changes with age. (Reprinted from Lewis CB. What’s so different about rehabilitating the older person? Clin Manag. 1984;4[3]:12.)
OSTEOPOROSIS
Distinguishing “Normal” Aging of Bone From Osteoporosis
Osteoporosis is no longer considered an inevitable consequence of aging. Many of the sequelae associated with the development of osteoporosis can be prevented by the development of a healthy peak bone mineral density during childhood with a maximum density at the time of physiological maturity and by using sound nutritional and exercise practices throughout the lifetime to maintain mineralization of the bone.10 Understanding the controlling mechanisms of bone cell response to nutritional and biochemical interventions and mechanical loading is important in preventing the development of osteoporosis (see also Chapter 3).
Mechanical Stress
Physical stress on bone stimulates increased bone deposition. Exercise can apply compressive and tensile stress; in addition, simply overcoming the forces of gravity on the musculoskeletal system or resisting impact can stimulate bone deposition. Because of the large number of muscles (more than 600) that originate and insert on the numerous bones of the skeletal system (around 206), muscle contraction, especially against resistance (gravity or external loads), can place large forces on the muscle–tendon– bone joints, and these forces are relayed to the bone matrix. These facts are being revealed in tests with astronauts in the US Space Shuttle program; in addition, efforts are being made to use exercise in zero gravity as a means to retard increased bone resorption during space flights.
There is a clear age-related loss in bone mineral content. This loss occurs first in cancellous bone, which begins to decline before the third decade of life. Compact bone is retained for another decade before resorption increases11–13 (Figure 11-3). The decline in trabecular bone mineral content is greater for women than men and greater again for postmenopausal women.14–18 After menopause, the rate of trabecular bone mineral loss in women can increase to 7% per year, with the greatest loss in the first 5 years. This rate of loss is large compared with the average loss before menopause of less than 1% per year.14
Conditions That Influence Age-Related Decrease in Bone Mineral Content
With aging, there is a loss of bone mineral content as depicted in Figure 11-3. Several conditions can exaggerate this loss, including nutrition, endocrinologic factors, and exercise-related factors. The 2 main determinants in the development and severity of osteoporosis are peak bone mineral content and the rate of bone mineral loss.19 Thus, it is important to understand the factors that increase peak bone mineral content as well as how to retard bone mineral loss.
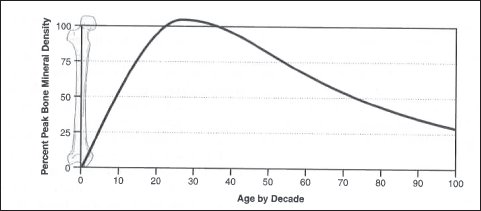
Figure 11-3. Life cycle changes in bone mineral content. Peaking at maturity and showing a gradual decline throughout the remainder of the life cycle. (Reprinted from Bottomley JM. Age-related bone health and pathophysiology of osteoporosis. Orthop Phys Ther Clin North Am. 1998;7[2]:117-132.)
Effects of Exercise on Bone Remodeling
Exercise is reported to influence bone mineral.20 Bone density was higher in athletes compared with sedentary controls, and athletes involved in weightbearing activities had the highest bone mineral content.20 The finding of increased bone mineral density in individuals involved in weightbearing activities has been shown repeatedly in similar cross-sectional studies.15,20,21 Furthermore, it is believed that the amount of muscle mass is proportional to bone mineral content.19,22 In other words, the stronger the muscle, the stronger the bone.
Exercise can affect the retention of bone mineral even in amenorrheic athletes involved in weightbearing activities. Exercise involving weightbearing retains more bone mineral than nonweightbearing. For individuals who have been involved in exercise throughout their lives, there is evidence that they maintain a higher bone mineral density (decreased resorption) compared to sedentary controls.23 The effects of exercise on the bone are discussed more extensively in a subsequent section of this chapter.
Risk Factors for Osteoporosis
Risk factors are not the cause, but they are contributing factors to the development of osteoporosis. The number of risk factors that predispose an individual to osteoporosis is not cumulative. That is to say, if you have 3 risk factors, you are not 3 times more likely to develop osteoporosis. Rather, the more risk factors identified, the greater the predisposition toward the development of osteoporosis. Factors such as age, sex, genetic makeup, race, body type, and complexion may initiate the process. Other factors such as poor nutrition, inactivity, and smoking may serve to accelerate bony loss.
Age is by far the most important empirical determinant of bone mass. From the fourth decade on, less bone is formed than is resorbed at individual remodeling foci, and this imbalance increases with advancing age.24 Although this imbalance in bone remodeling could be caused by osteoblast senescence, the observation that healing of fractures in older adults is not delayed suggests that aging does not impair the response of osteoblasts to appropriate stimuli. Serum levels of both growth hormone and insulin-like growth factor 1 (which mediates the effect of growth hormone on bone and cartilage) have been shown to decrease with aging.25
There may be impaired regulation of osteoblast activity caused by abnormalities in either systemic or local growth factors that are genetically influenced. Therefore, genetic factors may predispose an individual to the development of osteoporosis. At least 12 local regulators of growth produced by bone, cartilage, or marrow cells have been identified.26 Either age-related or genetic defects in the synthesis of one or more of these regulators may explain the uncoupling of bone formation from resorption that allows age-related bone loss. These factors include skeletal growth factor, bone-derived growth factor, macrophage-derived growth factor, a factor r esembling transforming growth factor beta, and prostaglandin E2.
Table 11-1 summarizes the relative risk factors in the development of osteoporosis.
Sex clearly influences the development of osteoporosis. Women have a higher incidence of osteoporosis related to lower levels of estrogen.
Race also appears to have an impact on the development of osteoporosis. White women, particularly of northwestern European background, and Asian women are more at risk than black women, in whom osteoporosis is actually very rare.27 Family history also plays a part in the development of osteoporosis. Slight build, fair complexion with freckles, and blond hair, all of which are genetically regulated, have a higher incidence of osteoporosis. Environmental factors, such as customary dietary habits developed within family structures, could play a role in increasing the risk for osteoporosis.
Mechanisms of the Benefits of Exercise
The effects of gravity and mechanical stress on the bone have been associated with functional adaptation of the bone.28 In other words, there is a continual remodeling of bone in response to functional demands placed on the bone. According to Wolff’s law, the internal architecture of the bone responds to stress by laying down more bone wherever the muscles are exerting their greatest force. Additionally, stress on the bone creates a negative potential within the bone according to the piezoelectric effect, thereby attracting positive ions, such as calcium.28
When force is applied to bone, bone bends, and there is an inherent moment of inertia applied to the bone. These mechanical stresses or loads are crucial in keeping bone healthy. Mechanical loads stimulate bone cells within the loaded region to deform and increase their synthesis of prostacyclin, prostaglandin E2, and other growth hormones and increase their synthesis of RNA. This causes the cascade of events within the osteoblasts and osteoclasts in response to changes in bone strain, reflecting an adaptation to the imposed loading environment.28 A minimum amount of strain is required to be effective for increased bone remodeling.
The major impact of activity on bone mass is localized. Bone mineral density is increased only in the areas that are stressed.29–31 Weightbearing and bone site–specific forces are the key factors in the relationship of bone development and muscle pull.30,31
Muscle mass and strength bear an interesting relationship to bone mass. There is a positive correlation between muscle strength and muscle mass with the bone mineral density.32,33 It appears that overall strength is the key factor as strength in one area typically reflects strength in other regions of the body. To affect change in bone mass, the training stimulus must exceed the normal loading of the muscle.
The type of exercise is very important. Sinaki’s landmark studies34,35 clearly demonstrated that in postmenopausal women who had sustained osteoporotic vertebral fractures, extension exercises significantly reduced the incidence of fracture reoccurrence, whereas flexion exercises increased the risk of fracture.
Based on current research, it is important to consider the following factors when prescribing exercise to enhance bone mass: (1) weightbearing physical activity is essential for the normal development and maintenance of a healthy bone mass; (2) sedentary older individuals may increase bone mass by becoming more active, but the primary benefit of the increased activity may be in avoiding the further loss of bone that occurs with inactivity; and (3) the optimal program for older adults would include activities that improve strength, flexibility, and coordination that may indirectly, but effectively, decrease the incidence of osteoporotic fractures by lessening the likelihood of falling.28–33
Table 11-2. World Health Organization Classification of Osteoporosis
| Normal | Bone mineral density that is not more than 1.0 standard deviation below the young adult mean value |
| Osteopenia or low bone mass | Bone mineral density that lies between 1.0 and 2.5 standard deviations below the young adult mean value |
| Osteoporosis | Bone mineral density that is more than 2.5 standard deviations below the young adult mean value without a history of fracture |
| Severe osteoporosis | Bone mineral density more than 2.5 standard deviations below the young adult mean value with a history of one or more fractures |
Adapted from Kanis et al36 as per the World Health Organization.
Table 11-2 shows the World Health Organization’s recommended classification of osteoporosis based on bone mass measurements. Categories are defined by comparing an individual’s bone mass to that of the average young adult. By World Health Organization’s definitions, osteopenia is described as a state of low bone mass. Individuals in this range are at an increased risk for fracture, and steps need to be taken to address diet modification and weightbearing exercise to prevent further bone loss. Individuals with greater loss in bone mass with no history of fracture are defined as having osteoporosis. These individuals are at an increased risk for fracture with minimal or no trauma. The most severe category are those people with marked loss in bone mass in addition to a history of fracture. These individuals are defined as having severe osteoporosis.36 See Appendix C for evidence-based evaluation and treatment ideas.
OSTEOPENIA
Osteopenia refers to metabolic bone diseases that are characterized by x-ray findings of a subnormal amount of mineralized bone mass. The most common osteopenia is osteoporosis, which is generally defined as a decrease in the quantity of bone with an increased incidence of fractures from minimal trauma. One of the first signs of osteoporosis is alveolar bone loss called dental osteopenia followed by bone loss in vertebrae and long bones. Indeed, there appears to be a strong correlation between skeletal osteopenia and density of alveolar bone.37 Dental osteopenia leads to an inadequate amount of bone mass in the mandible, loss or mobility of teeth, edentulousness, and inability to wear dentures.38
It has been found that calcium deficiencies and calcium-phosphorus imbalances contribute to the development of osteopenia and the subsequent pathogenesis of osteoporosis.39 Prevention and management include not only increased calcium intake but also estrogen therapy, dietary vitamin D, and exercise.
Osteopenia commonly is present in hyperthyroidism, and the development of hyperthyroidism aggravates normal age-related bone loss. Mild hypercalcemia is commonly seen in hyperthyroidism due to the endocrine imbalance of the thyroid hormone. Estrogen acts on the thyroid gland to produce calcitonin. In a condition in which there is too much thyroid hormone and too little estrogen, calcium absorption is decreased, and calcium excretion is increased. In hypothyroidism, there is a mild decrease in the rate of calcium deposition in bone related to the imbalance between the decreased amount of thyroid hormone and a surplus of parathyroid hormone.
OSTEOMALACIA
Osteomalacia is a bone disorder caused by a failure of normal calcification of the bone matrix. The most common causes of osteomalacia are vitamin D deficiency, a calcium deficiency, abnormal metabolism of vitamin D, and low serum calcium-phosphorus levels. In contrast to osteoporosis, in which there is a loss of bone mass and resulting brittleness of the bones, osteomalacia causes the bones to soften due to poor mineralization and an inability to absorb vitamin D, calcium, and phosphate.40
The primary etiology is a vitamin D deficiency, which results in poor absorption of calcium in the intestines and increased excretion of phosphate from the kidneys. Vitamin D is obtained from the diet (D2 and D3) and from biosynthesis following exposure to sunlight (D3). Its metabolite, 1,25-dihydroxyvitamin D (1,25[OH]2D), enhances the gastrointestinal absorption of calcium and phosphate and thus has a direct effect on the bone calcification process. Vitamin D deficiency may result from dietary restriction of food (eg, too little fish, whole-grain flour, and dairy products), malabsorption of vitamin D, or insufficient exposure to ultraviolet radiation.40,41
Vitamin D from the diet is absorbed in the upper small bowel via fat-dependent absorption. Derangement in upper intestinal function or fat malabsorption can result in vitamin D deficiency. Diagnoses such as pancreatic insufficiency, irritable bowel syndrome, biliary obstruction, or sprue can lead to poor absorption of this essential nutrient.
Once absorbed, vitamins D2 and D3 are hydroxylated in the liver to 25-hydroxyvitamin D and subsequently in the kidneys to 1,25(OH)2D. Interference with the metabolism of vitamin D may contribute to the development of osteomalacia. Liver disease, particularly cirrhosis of any etiology, may interfere with hepatic 25-hydroxylation of vitamin D. In renal failure, the deficiency of renal 25-hydroxyvitamin D 1-alpha-hydroxylase activity is the primary cause of osteomalacia because it produces a deficiency of 1,25(OH)2D.
Certain drugs may also impede the absorption of vitamin D by causing an increase in vitamin D excretion or catabolism. Drugs that increase the hepatic degradation of 25-hydroxyvitamin D, such as phenytoin and phenobarbital, are known to predispose individuals to osteomalacia. In nephrotic pathologies, there may be an increase in vitamin D clearance and excretion, which results in a deficiency of vitamin D.40,41
Phosphorus is also essential for the calcification of bone. Hypophosphatemia may result from gastrointestinal or renal loss of phosphate, which is independent of parathyroid or vitamin D metabolism. Malabsorption and subsequent gastric and intestinal tract wasting of phosphates may be compounded by vitamin D deficiency and hyperparathyroidism. This malabsorption also may be exacerbated by phosphate-binding antacids. Renal wasting of phosphorus is a prominent feature of proximal renal tubular disorders. These disorders range from defects that limit phosphate absorption and increase phosphate clearance to renal failure, which results in defects involving absorption of phosphorus, glucose, amino acid, uric acid, and vitamin K. In renal tubular acidosis, the acidotic state will repel positive ions, such as calcium and phosphorus, and contribute to the development of osteomalacia.41
The classic symptom of osteomalacia is generalized or localized bone pain. The pain is often exaggerated by movement, and bony tenderness is common. A complaint of general fatigue and achiness is often heard. Proximal myopathy and sensory polyneuropathy may accompany these complaints. Initially, the progression of osteomalacia is insidious and deformity is unusual, although pathologic fractures ultimately may occur as bone strength declines and result in vertebral wedge fractures, bowing of the femur and tibia, and postural changes similar to those seen in osteoporosis. Gait and functional declines are associated with the overall loss in muscle strength.40
Treatment must address the nutritional-malabsorption component of this metabolic disorder. Dietary supplementation of vitamin D may be required to restore positive calcium balance and normal bone mineralization. The gastrointestinal, hepatic, or renal disorder underlying osteomalacia must be treated. Research indicates that exercise has a positive effect on osteomalacia only when adequate dietary vitamin D is provided and the metabolic disorder corrected. Then, exercise has a positive effect on bone mass, similar to that described in osteoporosis.40,41
AVASCULAR NECROSIS
Death of bone and the cellular components of bone in the absence of infection is referred to as osteonecrosis or avascular necrosis. Avascular necrosis is the result of a disrupted arterial supply and most commonly affects the femoral head following an intracapsular or femoral neck fracture in which the circumflex arteries are injured as a result of the fracture. Avascular necrosis also can be the end result of a thrombosis of an artery supplying bone. The bone tissue becomes ischemic, and permanent loss of bone occurs.42
Osteonecrosis, a process of “creeping substitution” in which there is resorption of “dead” trabeculae and woven bone is laid down on dead trabeculae, results in the collapse of bone. Osteonecrosis can result from a number of etiologies, but most commonly it is associated with fracture, alcoholism, pancreatitis, diabetes mellitus, obesity, or gout. Other conditions that may lead to avascular necrosis include systemic lupus erythematosus, Cushing disease, caisson disease, Gaucher disease, idiopathic Chandler disease, sickle cell anemia, and long-term corticosteroid use.43
Although the talus, scaphoid, and proximal humerus are susceptible to osteonecrosis, the femoral head is the most common site associated with this pathology. The femoral head and neck receive their circulatory supply from the medial and lateral femoral circumflex artery, which travel in a distal to proximal direction in the femoral neck and head. Fracture or displacement secondary to fracture of the neck of the femur can compromise the circulation to the head of the femur and lead to death of the bone. Following trauma or with insidious conditions, pain is reported in the groin, medial thigh, and knee, which is intermittent and associated with weightbearing activities. Internal rotation, flexion, and adduction of the hip exacerbate the pain, and the patient will present with an antalgic gait. Radiographic examination will show the source of arterial disruption if a fracture is present but not for conditions like thrombosis. A more sensitive evaluation of bony status (eg, a bone scan, magnetic resonance imaging, or computed tomographic scan) is required to detect earlier and subclinical stages of bone loss. In older adults, the treatment of choice is total joint replacement.
PAGET DISEASE
Also known as osteitis deformans, Paget disease of bone is an example of an imbalance in which bone formation overtakes bone resorption. Paget disease is a progressive disorder associated with a marked increase in osteoblastic activity. At first, there is a softening and later an overgrowth and hardening of bone. The disease progresses in 3 distinct stages: (1) osteoclastic, (2) osteoblastic, and (3) sclerotic. In the early stages, blood flow increases to the affected bone—primarily the skull, vertebrae, pelvis, and bones of the lower extremities. There is an initial osteoclastic, resorptive stage in which abnormal proliferation of osteoclasts occurs. During this period of softening, characteristic deformities develop. The skull thickens and the forehead becomes prominent, the lower extremities bow, and the individual experiences the development of kyphosis in the thoracic vertebrae and a loss of the lumbar curve in the lumbar area with posterior prominence of the vertebrae. The initial resorption is followed by abnormal regeneration of bone through an overactive osteoblastic phase followed by sclerosis. The serum alkaline phosphatase levels are extremely high (over 100 units), indicating overactivity of the osteoblasts. The normal cancellous architecture is replaced by coarse, thickened layers of trabecular bone, and the cortical bone becomes thickened, irregular, eroded, and uneven. One would think that with the increased calcification of bone that the bone would be stronger; however, the converse is true—the bone is enlarged, eroded, and weakened by irregular alignment of trabeculae.41,44
The postural deformities seen in Paget disease result in a progressively increased thoracic kyphosis and bowing of the femur and tibia. If the femoral neck softens to the point of collapse, a reduced femoral neck angle (coxa vara) results in a waddling gait pattern. These postural changes increase local mechanical stress and are associated with increasing fatigue and bone pain.41
On radiographs, the vertebrae appear to be flattened and broadened. The cortical bone and end plates become exaggerated, and the cancellous bone develops a coarse yet almost transparent appearance. Primarily affecting the axial skeleton, the progressive stages of Paget disease weaken the bony structures, resulting in significant postural deformities. If the femur and tibia are involved, they, in addition to the vertebrae, are common sites of pathological or stress fractures in individuals with Paget disease.41
Symptoms are initially nonexistent, and the disease begins insidiously and progresses slowly. Often the disease is first detected by an abnormal radiograph or an incidentally elevated serum alkaline phosphatase level. Pain that develops is deep, aching bone pain often associated with stress fractures, hypervascularity, and mechanical stress of the excessively weakened bones. If the skull is involved, headaches, tinnitus, vertigo, and hearing loss are frequent complaints. Hearing loss is associated with the involvement of the ossicles of the inner ear or foraminal collapse and encroachment of the eighth cranial nerve. As the disease progresses, individuals usually complain of extreme fatigue, light-headedness, and overall “stiffness.” If pain occurs acutely, it is usually indicative of a pathological fracture.
Cardiovascular involvement is often associated with Paget disease as well. Due to vasodilatation of blood vessels in the bones, skin, and subcutaneous tissues overlying the affected bones, the individual may present with peripheral vascular involvement and an increase in cardiac output severe enough to result in congestive heart failure. In fact, it is the cardiac involvement that is the most common cause of death in the patient with Paget disease.44
Other clinical manifestations of Paget disease include nerve palsy syndromes and dementia. Nerve palsy syndromes occur as a result of entrapment of the nerves due to bony collapse. With bony impingement on the structures at the base of the skull, slurred speech, incontinence, diplopia, and impaired swallowing can occur.
Osteosarcoma is reported in less than 1% of individuals with pagetic bone and may be heralded by a rapid enlargement of bone, increased bone mass, or an elevation in serum alkaline phosphate levels.
Two classes of drugs are approved by the Food and Drug Administration for the treatment of Paget disease. Both classes of drugs suppress the abnormal bone remodeling that is associated with this disease. Bisphosphonates, such as alendronate sodium (Fosamax), etidronate disodium (Didronel), and pamidronate disodium (Aredia), are drugs that inhibit abnormal bone resorption. Calcitonin is a hormone secreted by the thyroid gland that also inhibits abnormal bone resorption (eg, Calcimar, Miacalcin, and osteocalcin). Other forms of treatment may include chemotherapy in the presence of osteosarcoma, limb-sparing resection, total joint replacement, or amputation.44
OSTEOARTHRITIS
The most prevalent orthopedic joint pathology is osteoarthritis. It occurs in 50% of individuals aged 65 to 75 years and 70% of people over the age of 75.44 Osteoarthritis is termed the “wear-and-tear arthritis.” The cause of primary osteoarthritis is unknown. It is defined as a noninflammatory progressive pathology of a movable articulation, especially a weightbearing joint, and is characterized by deterioration of articular cartilage and formation of new bone at joint margins and remodeling of subchondral bone.45 Osteoarthritis most commonly occurs in the carpometacarpal joint, the knees, and the hips. Patients will complain of pain during weightbearing in the joints, and the pain tends to be relieved by rest.
Classic treatment consists of nonsteroidal anti-inflammatory drugs. However, nonsteroidal anti-inflammatory drugs for older persons have received a somewhat negative review in the medical literature due to side effects associated with long-term use.46 In a remarkable study, physical therapy and nursing encouraged physicians to use more local and specific approach modalities, such as exercises that are specific to improve a person’s functioning in the osteoarthritic joints.46 It has been demonstrated that strengthening around an osteoarthritic joint can alleviate some of the pain as well as increase the strength and improve the functional mobility of arthritic patients.47,48 The clinical implication of these studies is that therapists should work with these patients on stretching and strengthening exercises frequently throughout the day. Specific techniques for the various joints of the body are given in subsequent sections of this chapter.
In addition to pharmacologic agents and exercise, typical interventions for osteoarthritis include education, rest, and possibly surgery. Patients should be instructed in joint protection and energy conservation techniques that can help prevent acute flare-ups and help to minimize joint stress and pain.
Table 11-3. Common Joint Deformities of Extremities in Rheumatoid Arthritis
JOINT | TYPICAL DEFORMITY OR CONTRACTURE |
| Hands (MCP/PIP/DIP) | MCP ulnar drift, swan neck deformity, boutonnière deformity, mallet deformity, rheumatoid thumb deformity |
| Wrist (carpal joints) | Volar subluxation, radial deviation |
| Elbow | Nodular enlargement, flexion, and pronation contracture and/or deformity |
| Shoulder | Adduction and internal rotation contracture and/or deformity, may have subluxation |
| Toes (MTP/PIP/DIP) | Hallux valgus, hallux rigidus, hammer toes, claw toes, mallet toes, overlapping toes, lateral subluxation with lateral deviation |
| Subtalar/midtarsal | Pronation, pes planus, instability |
| Ankle | Plantar equinus contracture and/or deformity |
| Knee | Genu valgus or genu varus, flexion contractures and/or deformity, subluxation of patella |
| Hip | Leg length discrepancy, flexion, and adduction contractures and/or deformity |
DIP, distal interphalangeal joint; MCP, metacarpal phalangeal joint; MTP, metatarsal phalangeal joint; PIP, proximal interphalangeal joint.
Rehabilitation should include appropriate weightbearing and nonweightbearing exercises. An individually designed program of strengthening, range of motion, and cardiovascular fitness exercises should be implemented. The design of the strengthening program should include low weight and much repetition to minimize stress on the joints. Exercise that produces pain indicates that the joint is being overstressed through too much resistance or incorrect performance of the exercise. Exercises incorporating low-load, prolonged stretching performed several times a day will help to gain a more appropriate, length-tension relationship for the muscles surrounding the affected joint and may lead to decreased stress in the intra-articular and periarticular joint structures. Heat modalities may assist in decreasing pain and stiffness, and cold modalities may decrease pain and inflammation. Splints, braces, and walking aids may also be warranted to decrease the joint stresses.
Surgical interventions such as arthroscopy, arthroplasty, and osteotomy are often used to provide symptomatic relief, improved joint mobility, and improved joint mechanics. Over 70% of hip and knee joint replacements are performed in older adults with osteoarthritis.49 Rehabilitation following total hip or total knee replacement are discussed in a subsequent section of this chapter. See Appendix D for evidence-based evaluation and treatment ideas.
RHEUMATOID ARTHRITIS
RA, a chronic, systemic inflammatory autoimmune disease, is the second major orthopedic pathology affecting the joints in older adults. Over 10% of people over the age of 65 are affected by RA, and the prevalence of this disease increases with advancing age.50 RA classically affects younger women 3 times more than men, although this predominance is less evident beyond the age of 60.50 The major differences between late-onset and early-onset RA are that the exacerbations tend to be severe and the remissions tend to be much better. Therefore, the therapist must be cautious during the exacerbation phases and limit therapy to active assistive and active exercises. During the remission phases, the therapist can be much more aggressive when designing a strengthening and stretching program for an older patient than one for a younger person.
The characteristic feature of RA is chronic inflammation of the synovium, peripheral articular cartilage, and subchondral marrow spaces. Due to chronic inflammatory states, granulation tissue called pannus is laid down, and the resulting friction erodes the articular cartilage.50 Inflammation of the tendon sheaths also occurs, resulting in the fraying and eventual rupture of the tendons. The resultant deformities of the hands with dislocation and lateral migration of the fingers and the same deformities of the toes are examples of the typical extremity deformities seen in patients with RA. Knee valgus is another example of deformities seen in this pathology.
Although the cause of RA is not specifically known, recent literature suggests that there is evidence of a genetic predisposition for the disease that is triggered by bacteria or viral infection. A definitive diagnosis is based on a combination of clinical manifestations and laboratory results. An individual with RA will often have a decreased red blood cell count, increased erythrocyte sedimentation rates, and a positive rheumatoid factor.
Clinically, RA manifests itself bilaterally, primarily affecting the small joints of the hands and feet, ankles, knees, hips, shoulders, elbows, and wrists. Table 11-3 describes the typical joint deformities seen in RA. The other area commonly involved is the cervical spine. Tenosynovitis of the transverse ligament of the first and second cervical vertebra and erosion of the facet joints may lead to cervical instability with the risk of neurologic damage from compression.50 See Appendix E for evidence-based evaluation and treatment ideas.
THE AGING SPINE
Pain in the neck and back is not uncommon in the older population. Although there is a higher prevalence of this problem in the population aged 35 to 55 years, older persons do have a relatively high incidence of back and neck dysfunction.51,52 Some of the major changes that are considered to be part of the normal aging process affect the cervical spine and back.
Muscles are less flexible, resilient, and strong.51,52 Nevertheless, Rider and Daly53 found that older adults respond well to flexibility and strength training. In their study, a group of older women whose average age was 72 were put on a spinal mobility program consisting of strengthening and stretching activities. The finding of this study was that functional mobility improved significantly.53 The loss of flexibility of all soft tissues will affect mobility of the spine.
The bone tends to become less dense or be affected by osteoporosis, and as a result the older person will tend to lose height. Approximately 20% of height is lost by the thinning of the intervertebral discs, but the majority of the height loss is caused by the collapse of the cartilaginous end plates secondary to a decrease in bone density and ballooning in the disc area.54
Joints are more prone to osteophytes. Twomey and Taylor54 have stated that the layer of fat pads in older joints acts as cushions against osteophytes and that these vascular systems are more highly innervated, which may cause more pain and sensitivity. If joint congruity is not maintained by the tone of the multifidus, there is a chance that torn portions of the cartilage would be displaced, particularly with sudden rotatory movement. Therefore, manipulative techniques would be particularly successful in freeing the torn pieces of cartilage; however, if the techniques are too aggressive, they may gap the joints and conceivably exacerbate the damage due to shearing of articular cartilage in the joint capsules.55 Aging changes in the cervical spine mean that older patients suffer from osteophyte formations and decreased range of motion with age. This was shown in an excellent study by Hayashi and associates.52 In addition, older patients experience a higher incidence of vertebral anterolisthesis and retrolisthesis and a slight decrease in the diameter of the spinal cord, which may or may not cause neurologic symptomology.54
The implication of these changes is that the therapist needs to work on strengthening, flexibility, and the appropriate manual therapy techniques to alleviate the older patient’s symptoms. Alternative exercise forms such as tai chi and qigong have also been shown to be effective in enhancing spinal mobility.56
SPINAL PATHOLOGY OF OLDER ADULTS
Lumbar Stenosis
There are many pathologies that can affect the spine of an older person. The first spinal pathology to be discussed is lumbar stenosis, which is a multilevel impingement on structures in the lumbar spine ligaments, usually by osteophytes.55 Pain may be in the back, hips, or lower extremities and worsens when the person walks or extends the lumbar spine.55 It is usually partially or completely relieved with flexion. Lumbar stenosis rarely affects anyone under the age of 60.57 Treatment for lumbar stenosis consists of the following:
❖ Rest for 1 to 2 hours in the afternoon with knees higher than the hips
❖ Flexion exercises of the trunk
❖ Heat and massage to decrease muscle spasm
❖ Teaching and enforcing posterior pelvic tilting in all positions and activities (see Appendix F for evidence-based evaluation and treatment ideas)
Vertebral Compression Fractures
Vertebral compression fractures usually affect the spinal areas of the thoracic and upper lumbar spine for older persons. Fractures can occur during any kind of routine activity, such as bending, lifting, or rising from a chair. The patient often complains of immediate, severe local back pain. The pain may subside in several months, but in some cases may continue for years. However, other vertebral compression fractures may cause no pain at all. The fracture may be gradual and asymptomatic and diagnosed only by radiographs.58 Multiple vertebral compression fractures will cause shortening of the spine and lead to the classic kyphotic position described earlier in this chapter. Progression of thoracic kyphosis can result in alveolar hyperventilation and retention of bronchial secretions with poor respiratory reserve. Eventually, the person may develop repeated episodes of pneumonia. Because all of the organs are compressed into a smaller space, often there are additional problems with abdominal symptoms, bloating, and constipation.58
Treatment for acute compression fractures is bed rest, but the patient must get out of bed every hour for 10 minutes to work on stabilization of the back.58 Pain relief modalities may be helpful, such as heat, ice, transcutaneous electrical nerve stimulation, or electrical stimulation, to relieve some of the symptoms.59 The authors of this book have found that the use of a 6-inch Ace wrap or the binders used with rib fracture is very helpful in providing support and comfort in the area of the compression fracture. Once the person can tolerate exercise, extension exercises should be used extensively.59 Any type of extension exercises to the thoracolumbar spine is helpful.34,59 See Appendix G for evidence-based evaluation and treatment ideas.
Cervical Spondylosis
One of the pathologies affecting the neck of an older person is cervical spondylosis, which is defined as degenerative changes in the cervical spine. Symptoms of this are pain in the cervical spine with possible radiculitis into the shoulder, arms, or fingers.60 The treatment for cervical spondylosis includes anti-inflammatories, keeping the neck in neutral or a slightly flexed position, manual traction, heat, active range of motion, and progressive resistive exercises that the patient can tolerate.61
Vertebral Artery Syndrome
A second pathology of the cervical spine is vertebral artery syndrome (VAS). An encroachment on the vertebral foramina results in VAS, and this can be caused by a multitude of things. The most likely cause is the combination of a narrowing of the disc, osteophyte formation from osteoarthritis, and a forward head position.62 The symptoms of VAS are dizziness, tinnitus, and blurred vision that occur in conjunction with a combination of neck rotation and extension. The treatment for VAS is wearing a cervical collar to prevent extension, axial extension exercises, and cervical isometric exercises.62
The standard test for VAS is to rotate and fully extend the cervical spine while evaluating for dizziness, nausea, and nystagmus of the eyes. Caution when evaluating an older individual with suspected VAS needs to be applied. Using the standard vertebral artery test is not advisable and could actually be dangerous.63–68 Performing the vertebral artery test may decrease blood flow in the vertebrobasilar circulation enough to result in infarction.67,68 Arterial diagnostic testing would confirm the therapist’s suspicions of the presence of VAS. The Dix-Hallpike maneuver69 is the typical test performed in 45 degrees of cervical rotation and 30 degrees of extension to diagnose benign paroxysmal positional vertigo. This maneuver does not place the older adult in as much risk as the vertebral artery test because the patient is not placed in end-range rotation or extension. Often nystagmus can be seen in older adults by placing them in the supine position with their head turned, although the supine position may not be comfortable for the severely kyphotic individual. An alternative is to perform the Dix-Hallpike test on the person with kyphosis using a tilt table with pillows to support the spine and head. By lowering the person’s entire body, the person’s alignment remains the same; yet, there is stimulation to the semicircular canal. If the patient becomes vertiginous in the Trendelenburg position and complains of vertigo with head rotation and extension, this is indicative of the possibility that the individual has VAS.70,71
Rheumatoid Arthritis
A third pathology causing problems in the neck in older adults is RA. Patients/clients with RA with subsequent neck pain will tend to experience the pain in the middle area and the posterior aspect of the cervical spine. Therapists should check the x-rays for atlanto-occipital subluxation. If present, the therapist should not use any manual techniques that could further exacerbate dislocation (eg, mobilization, traction, or occipital release).62 Proper treatment includes supporting the neck with a cervical collar, heat, ultrasound, gentle massage, and range of motion and progressive resistive exercises.62
Ossification of the Posterior Longitudinal Ligament
The fourth pathology of the neck is ossification of the posterior longitudinal ligament (OPLL). In OPLL, the ligament tends to ossify, usually over several segments of the cervical spine. This causes limitation in neck flexion and radiculopathy.72 The treatment for OPLL consists of heat, cervical traction, and rest from sedentary static activities such as knitting, reading, computer usage, or desk work. In addition, stretching and range of motion or progressive resistive exercises are helpful.
In all of these pathologies, the therapist must first check the person’s environment. Frequently, adding pillows between the knees while the person sleeps in the side-lying position can provide relief for low back pain. Putting a lumbar pillow in the wheelchair or changing the level of the footrests can provide relief for the entire spine. Since older patients spend so much time sitting and some patients are often bound to their chairs, the therapist must check their environments to make sure they are not exacerbating any spinal symptoms. Often a simple modification of the environment can provide tremendous relief from spinal pain. See Appendix H for evidence-based evaluation and treatment ideas.
THE UPPER EXTREMITY
The Shoulder
Range of motion in the shoulder does decline with age. Despite the fact that studies have documented age changes,73,74 clinically there is evidence to show that if a person uses the shoulder more frequently, the range of motion decrease will be less. The aging shoulder is more prone to certain pathologies, such as the ones discussed here—osteoarthritis, bursitis, and rotator cuff tears.
Osteoarthritis
The first pathology, osteoarthritis, is very rare and may be overdiagnosed. Only 2% of shoulder problems in older adults are truly osteoarthritis.75 The symptoms of true osteoarthritis are a constant ache, crepitus, difficulty sleeping, and weakness. When the therapist moves the shoulder, there is a hard end felt with joint movement. In addition, there will be a grinding and a dryness with shoulder movement.76,77
Treatment of osteoarthritis, when the patient has severe joint pain, is rest, gentle pain-free range of motion exercises, and anti-inflammatories.76 However, once the patient can move through range with less pain, heat or ice, functional adaptation, joint mobility, gentle weightbearing isometrics, and range of motion exercises can be helpful. In addition, thermal modalities, such as ultrasound and ice, can be very helpful in alleviating pain.
Bursitis
The second shoulder problem, which is more commonly seen than osteoarthritis in the older population, is bursitis. The symptoms of bursitis are the following:
❖ A palpable tenderness in the area of the inflamed bursa
❖ Pain with movement of the muscle affected by the temporary bursa
❖ Symptom relief with rest77
The patient will usually have a recent history of overuse of the shoulder prior to the initial onset of symptoms.78
Treatment for bursitis is heat or ice, ultrasound, and energy conservation. Painful movements should be avoided, and the patient should begin pain-free isometrics when he or she can tolerate them. No exercise should be done that exacerbates the pain, but having the patient exercise below and above a painful arc will be useful.
Rotator Cuff
The third shoulder pathology, and the one most commonly seen in older adults, is rotator cuff problems. The rotator cuff is composed of the infraspinatus, the supraspinatus, subscapularis, and teres minor. An x-ray of the subacromial space of less than 5 mm is diagnostic of a rotator cuff tear.78
With the rotator cuff, the patient will complain of pain when sleeping on the shoulder. He or she will be positive on the impingement sign when the arm is brought to full passive flexion, and pain will be present for the last 10 to 20 degrees. Crepitus and catching sensations due to fibrosis and scarring may also be present. If the problem progresses, the patient/client may even have atrophy of the rotator cuff muscles and definite weakness in the shoulder abductors and flexors.79
Treatment for impingement, tears, and tendinitis of the rotator cuff is symptomology management. If the person has pain throughout an arc, the therapist should avoid range of motion exercises that use the arc and irritate the rotator cuff. The patient can be instructed to passively move the shoulder through that range and to do some end-range stretching and strengthening exercises. Heat, ultrasound, and electrical stimulation may help decrease the inflammation. Passiv e- and active-assisted stretching exercises can also be helpful as well as isometrics that do not encourage tightness in the shoulder musculature. The person must exercise the arm at least twice a day to see significant improvement.
Adhesive Capsulitis
Rotator cuff dysfunctions can become more irritating problems if the person develops a frozen shoulder. Although frozen shoulders are not always preceded by rotator cuff problems, they are a common occurrence in older adults. With frozen shoulders or adhesive capsulitis, a person may or may not experience pain. A capsular pattern in which external rotation is most limited and abduction, flexion, and internal rotation of the shoulder are also limited is a symptom of adhesive capsulitis. The person may display a protracted scapula and atrophy of the deltoid, rotator cuff,78 biceps, and triceps. Tenderness of the anterior joint may also be present.
Treatment for a frozen shoulder is heat or ice depending on how painful the joint is and how well the person tolerates ice. Extremely painful joints may need the numbing effect of ice. Ultrasound can also be used to relieve some inflammation. Joint mobilization must be done in all limited directions followed by active-assisted or passive range of motion and contract-relax stretching. Posture work and scapular retraction exercises are also helpful.
Humeral Fracture
Humeral fractures are the final pathology to be discussed here. Classically, they will be either displaced or nondisplaced. Slightly more nondisplaced fractures occur, and they usually require pinning or wires. A fractured humerus usually requires that the patient use a sling for 1 week. After that time, the patient can remove the sling to work on general pendulum exercises, shoulder shrugs and circles, protraction and retraction, and any active motion exercises for the hand or wrist. At this point, the person should be doing no passive range of motion. For the first week, the patient should also learn ways of writing, eating, and performing activities of daily living without stressing the shoulder.77
By the third week, the patient can begin gentle isometrics, either against the wall or using a Theraband. Active range of motion in the pain-free ranges can begin at this point as well, and the person should begin doing scapular humeral rhythm motion in front of the mirror (ie, elevating the arms without raising the shoulders). This type of activity can also be used for all the previously noted shoulder pathologies. One of the most prevalent problems is that patients with shoulder pathologies have poor scapular humeral rhythm. Normally, they do not achieve full range of motion because they are never taught how to properly move the shoulder. Simply working with patients in front of a mirror and encouraging them not to lift the shoulders as the arm is lifted is adequate for attaining the desired results.
By the sixth or eighth week, if the patient is healed, joint mobilization can begin. Passive range of motion can also begin, but scapular humeral rhythm should be stressed. See Appendix I for evidence-based evaluation and treatment ideas.
THE LOWER JOINTS OF THE UPPER EXTREMITY
The joints of the upper extremity (the elbows, wrists, and hands) show minimal changes in range of motion with age. However, strength does decline.80,81 The practitioner should be careful when looking at grip strength measures in older adults because studies have shown that the older patient’s grip and pinch strength may be influenced by extraneous variables. These variables range from mental status to gait and balance problems. Therefore, grip strength may not be a true indicator of strength in the older population.82,83
The Elbow
Almost one-quarter of all elbow traumas and one-third of elbow fractures are fractures of the radial head,84 which usually are stabilized with an internal fixation device. For the first 3 weeks, the patient is immobilized in a hinged splint with the forearm held neutral. The patient can do range of motion exercises with the hand and shoulder, and to control swelling, cold packs can be applied for 10 minutes every hour. At day 21, active range of motion exercises can be started and passive range and progressive resistance exercises (PREs) can be increased gently as the patient/client tolerates. This regimen is followed slowly until 12 to 15 weeks.84
It is important to note that since this is such a painful fracture, practice and skill acquisition on a visual level may be beneficial. According to Maring,85 the experimental group who visualized a forearm activity did much better than the control group who did not.
The Wrist
The most common pathology of the wrist is Colles fracture, which is a fracture of the distal radius as a result of a fall on the hand. It can be treated by closed reduction, or it can be reduced by screws.86 The therapist will usually see the patient once while the extremity is in a cast for instruction in edema control and for range of motion exercises for the uncasted upper extremity joints. After 4 weeks, the cast is usually removed, and at that time the therapist can use modalities as needed, such as heat, ice, and electrical stimulation to control swelling and increase circulation. Gentle joint mobilizations to the carpal joints, active range of motion, and gentle passive and resistive exercises can be started at this time. By 6 weeks, when the person is completely healed, the therapist can begin work on more vigorous passive resistive, contract-relax stretching exercises, or both. The therapist should be sure to reinforce the exercises with daily, functional activities at home.
RA or osteoarthritis often affects the wrist. Marked limitation in joint mobility can severely impede functional capabilities. Often splints are advised to protect the wrist during activity. Joint protection techniques should be a part of therapy intervention. Teaching an individual how to manage activities of daily living without stressing the joints of the wrist will decrease the amount of pain and inflammation.
The Hand
The most common pathologies in the aging hand are:
❖ RA
❖ Osteoarthritis
❖ Dupuytren contracture
Rheumatoid Arthritis
In RA, the synovial fluid in the joints of the hand becomes particularly painful, and the person may develop ulnar drifting and significant deformities of the hand. The patient may undergo surgery or arthroplasty for severe deformities; nevertheless, the therapist can work on light exercises and splinting to help alleviate pain symptoms as well as focusing on range of motion deficits.87
Osteoarthritis
Osteoarthritis of the hand is more common than RA. It most commonly involves the interphalangeal joints and the carpometacarpal joint of the thumb. Since the thumb is so important for functioning, this particular problem can be devastating. The patient will present with pain, swelling, and weakness, possibly due to overuse of the hand. The treatment involves joint protection, splinting to stabilize the thumb, joint mobilization, and strengthening exercises. Heat, ice, paraffin, and ultrasound can also give relief from pain and inflammation.87,88
Dupuytren Contracture
The final pathology involving the hand is Dupuytren contracture, which is relatively uncommon in people under 50. It is caused by excessive collagen formation around tendons, nerves, and blood vessels in the palm of the hand, and it can cause minimal or permanent flexion of the fingers, usually of the proximal interphalangeal joints. Figure 11-4 demonstrates a typical Dupuytren contracture. It is usually not painful, and, therefore, people often delay treatment. However, treating the problem early can be extremely effective. Heat and ultrasound to the fascia of the hand followed by unidirectional transverse friction massage, stretching, and splinting in a stretched position can be extremely helpful. Patients are encouraged to continue the friction massage, range of motion exercises, and heating at home to enhance the benefits of the therapeutic regimen.87 See Appendix J for evidence-based evaluation and treatment ideas.

Figure 11-4. Typical Dupuytren contracture in an older man.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








