67.1
Engaging the orthopedic specialist
While orthopedic surgeons are recognized as technicians in the care of patients with fragility fractures, their potential influence on the treatment of millions of patients with low bone mass and osteoporosis has not been fully utilized in our health-care systems. In the United States, almost every person will see an orthopedic provider at some point in their lives, either for a fracture or for an elective procedure. Musculoskeletal complaints, particularly for the older adult and geriatric patient, are among the most common reasons for a person to seek medical care. Treatment of hip fractures and joint replacement remain in the top five expenditures for Medicare and are rapidly escalating in frequency and in overall healthcare spending dollars as the geriatric population grows . Orthopedic surgeons see and operate on patients every day with osteoporosis and low bone mass. Older joint replacement and spinal fusion patients are first mentioned when osteoporosis and orthopedic surgery is considered. However, even hand surgeons, sports surgeons, and pediatric surgeons see patients who are at risk for low bone mass, osteoporosis, and compromised bone quality. Young patients with stress fractures from sports, vitamin D deficient patients, amenorrheic young women, men with low testosterone, patients with eating disorders, patients on steroids, patients with autoimmune inflammatory disorders, patients with paralysis, patients with developmental or genetic disorders, cancer survivors who have had chemotherapy, transplant patients, lifelong active smokers, and patients with history of parathyroid or thyroid disorders are among those who present to elective practices without fractures. Recognition of osteoporosis and poor bone quality is important as it can affect surgical planning, hardware choices, and patient outcomes. Orthopedic surgeons can play an important role on the health-care team identifying patients with osteoporosis or low bone mass and helping to direct them to medical care to prevent future fractures .
67.2
Geriatric fracture care and care treatment pathways
Fragility fractures occur when a patient falls from standing height or less and suffers a fracture. Both patients and providers underappreciate that these falls actually represent low-energy injuries and demonstrate the biomechanical weakness of the patient’s bone and the disease of osteoporosis. A fall from standing height or less that results in a fracture, while painful and debilitating for the patient, is very different than an injury that results from a higher energy event such as a car accident or a fall from a height . Recognizing this difference is extremely important in helping to diagnose and treat patients with osteoporosis to prevent future fractures for these patients . Many hospitals and health systems have developed treatment algorithms and pathways. These pathways coordinate the care of the patient between orthopedic providers, medical providers, anesthesiologists, physical therapists, discharge management teams, and osteoporosis care providers in order to provide comprehensive care to the patient both during the acute treatment phases and in the recovery period. Every member of these treatment teams plays an important role in the efficient and cost-effective care of geriatric fragility fracture patients . Pathway care has demonstrated decreased complications in this medically fragile population, and in some instances, significant cost savings and shorter hospital stays. This is particularly important with hip fracture care and care of fractures that require an inpatient stay and surgery. Care of hip fracture patients represents one of the top expenditures in the United States for Medicare annually and with the aging population, costs are expected to grow as fracture numbers grow .
Surgical management of fragility fractures is urgent in order to minimize the sequelae of complications, such as pneumonia, skin breakdown, and venous thromboembolism, that often follow as a consequence of the fracture. It is well documented that hip fractures have optimal outcomes when managed within 48 hours of the event . However, a large proportion of patients suffering from these osteoporotic fractures are elderly and have multiple comorbidities that must be assessed and optimized before the patient is brought to the operating room. A 75% of hip fracture patients are older than 70, and 95% of these patients have at least one major comorbidity . Rushing an unstable patient to surgery does not lead to improved outcomes, and failure to identify and manage risk factors exposes the patient to increased chance of intraoperative and postoperative complications. Perioperative assessment and optimization must be streamlined to balance urgency versus risk reduction, remembering that prompt surgery is, in and of itself, risk reduction. A team-based approach, working with geriatricians or hospitalists, and anesthesiologists, best facilitates preoperative preparation. After initial stabilization in the emergency department, a 12-lead EKG and basic laboratory tests, including complete blood count, basic metabolic panel, prothrombin time/international normalized ratio, and type and screen, should be obtained. These initial results will help one to identify anemia, renal function and electrolyte disturbances, coagulation status, and possible issues with donor blood products in the presence of antibodies. Anemia, hypoxia, electrolyte disturbances, hypovolemia, and arrhythmias should be corrected as much as possible preoperatively .
Beyond these routine tests, a detailed history and physical exam is often the only thing necessary before proceeding to the operating room. A patient with good functional status and absent or stable comorbidities may proceed to surgery without any delay for further evaluation . Functional capacity can be assessed using metabolic equivalents (METs). Perioperative risk of adverse events is increased in patients unable to perform four METs of work. Activities requiring at least four METs of work include climbing one to two flights of stairs, walking at a pace of 4 mi/h for 15 minutes, or doing heavy house or yard work. Some comorbidities require further evaluation and treatment. Active ischemia or myocardial infarction, decompensated congested heart failure, unstable arrhythmias, transient ischemic attack or stroke, pulmonary compromise, and renal failure should be addressed preoperatively. Mechanism of injury is another consideration. Unwitnessed falls in patients with cognitive impairment should not be presumed to be mechanical; further investigation to rule out cardiac or neurological causes is warranted. Anticoagulated patients may require reversal. For patients on vitamin K antagonists, vitamin K, fresh frozen plasma (FFP), and prothrombin complex concentrates are all options. Vitamin K is not recommended as its effects are too delayed to be of benefit in urgent surgery, and those effects are of longer duration than is necessary . FFP can contribute to volume overload for chronic heart failure (CHF) and renal failure patients. Factor Xa agents rivaroxaban may be reversed with andexanet alfa in the event of uncontrolled or life-threatening bleeding .
Echocardiography (Echo) is rarely needed prior to proceeding to the operating room. However, preoperative echo is indicated for patients with dyspnea of unknown origin, and for patients with current or prior heart failure (especially with worsening dyspnea) who have not had an evaluation within the past 12 months, as per the American College of Cardiology/American Heart Association 2014 task force guidelines for preoperative evaluation . In addition, a current echo study is helpful for evaluating pulmonary hypertension and valvular heart disease such as aortic stenosis; this information is valuable for selection of anesthetic technique. Information about pacemakers and implantable cardioverter defibrillators is necessary for intraoperative risk reduction, especially if the patient is known to be pacemaker dependent. Device interrogation is not routinely needed as major manufacturers have 24-hour telephone support that can supply device type, date of implantation, magnet behavior, and indication for placement. If patients, their surrogates, or medical records do not provide even a manufacturer’s name, preoperative interrogation should be obtained if at all possible . However, delays beyond 48 hours solely to obtain this information are unlikely to be in the patient’s best interest. Transcutaneous pacing, defibrillation, and a magnet should all be readily available in the operating room, with or without this device information. If the decision is made to proceed with surgery without device information, telemetry admission may be necessary postoperatively until the device can be evaluated.
Effective analgesia is part of preoperative optimization and should be administered as quickly as possible. Pain leads to sympathetic stimulation, increasing myocardial work and oxygen demand. For patients with coronary artery disease, cardiomyopathy or ventricular hypertrophy from aortic stenosis, a supply/demand mismatch can trigger myocardial ischemia. Intravenous hydromorphone or morphine titration is straightforward and efficient. Opioid administration is not related to delirium . If regional anesthesia is available, nerve blocks are an extremely effective form of pain control. For hip fracture, Rashiq et al. found that a combination of obturator and lateral femoral cutaneous nerve block is likely to be most effective against postoperative pain, while fascia iliaca blockade is likely to be most effective against delirium . All risk is relative. Osteoporotic fracture patients (or their surrogates) may decide to proceed with high-risk surgery as palliative care even in the face of advanced comorbid disease. Targeted preoperative evaluation and treatment, focused on factors that can be optimized, allows for truly informed consent.
Postoperative care also requires close team interactions. Some engagement with family and caregivers, particularly regarding discharge planning, can occur immediately upon patient presentation to the emergency room prior to surgery. Early mobilization with physical therapy, fall prevention evaluations and training, engagement with the family and caregivers to minimize falls, and careful discharge and disposition planning should begin as soon as possible during the hospital stay. Fracture liaison services have been used in multiple institutions and countries to help identify and provide postfracture medical evaluation and treatment for osteoporosis. These services use a variety of doctors, nurses, and nonnurse care coordinators to ensure that patients get a bone density (DXA) scan, appropriate medical labs, fall prevention education, and appropriate prescribing of osteoporosis treatment medications. The general consensus regarding the establishment of fracture liaison services is that each health system, practice, or institution needs to establish an algorithm that works best with the providers and resources available in that community . Electronic medical records can aid in the identification of patients, but a direct connection with a provider for treatment of the osteoporosis (physician, nurse practitioner, or physician assistant) must also be a part of the plan. While these coordinated systems have demonstrated a significant improvement upon the historical rate of osteoporosis diagnosis and treatment of only 20% of post fragility fracture patients, none are able to capture and treat all of the patients .
67.3
Orthopedic hardware and fragile bone
Osteoporotic bone creates some significant challenges in the management of fractures and other orthopedic elective procedures because the strength of the bone has changed making it more difficult to anchor hardware to the bone . When a bone is loaded mechanically, a complex cooperation between the cortical bone around the outside of the bone and the trabecular bone within the intramedullary canal allows the bone to absorb that loading energy. Significant trabecular bone is lost with aging and with the disease of osteoporosis, creating gaps in this mechanical support system that can make it easier to fracture the bone. What is often forgotten is that the cortical bone is also affected by osteoporosis as it thins and there is an increased porosity within this compact bone. Screws depend upon these cortices to stabilize plate/screw fixation devices to the bone. This fixation allows for some of the mechanical energy that travels across the bone during weight bearing and activity to transfer to the plate (load-bearing construct) until the fracture has healed. If the fracture never heals, the orthopedic hardware will eventually break. The increased porosity and decreased thickness of the bone cortices decrease the contact area between the screw threads and the bone making it more difficult to transfer energy to the hardware. In addition, the bone surrounding the hardware is often weaker than the hardware itself decreasing the strength and energy that is necessary to pull the screws completely out of the bone cortex and disengaging the hardware. Several techniques and special modifications to hardware have been developed in order to manage these challenges presented by osteoporotic bone .
Larger screws with a larger distance between the central core of the screw and the threads, and screws with and increased number of threads (more threads per cm) can increase the grip of screws to the bone. The tip of each screw is tapered and does not have a full set of these wider threads along the first few millimeters of the screw. For that reason, when treating osteoporotic bone, screws must be advanced further through the far cortex of the screw pathway in order to move past this tapered tip and allow for the shaft of the screw and its threads to fully engage that far cortex. This decreases the chance that the screws will pull out of the bone while under mechanical stress. If screws do not fully engage the far cortex, screw pullout strength is only one-eighth of that if it does fully engage. Constructs also depend upon having multiple screws engage the bone both proximal and distal to the fracture sites in order to share the mechanical stresses across as many contact points as possible in the weak bone of osteoporosis . Hydroxyapatite-coated screws are commonly used in spine to engage the cortices of the pedicles as they pass through and to allow bone to grow directly onto the coating on the surface of the screws to improve stability of these pedicle screws. Similar hydroxyapatite-coated screws are available for standard fixation plating and in animal testing have demonstrated increased pullout strength. Augmentation of screw pathways with polymethylmethacrylate (PMMA), calcium phosphate, and calcium sulfate injectable cements also offer a way to increase the surface connections of the surrounding bone with the hardware. This technique of cement augmentation can be particularly helpful in the femoral head and humeral head where there are often large voids of trabecular bone in the osteoporotic patients and screws extending into these regions cannot pass through the far cortex because they would violate the joint space. Techniques with the placement of cement and the insertion of premeasured screws through the cement before it hardens, or the injection of one of these cements through already seated screws that have fenestrations in their distal ends to allow outflow of these cements can be used .
Locking plates have been a major advancement in the treatment of fractures for patients with osteoporotic bone. With standard plates the construct is dependent upon the interaction between the screws and the bone in which they are anchored. With locking plates the heads of the screws thread into the plate and lock into a position along the plate that allows for the transfer of energy from the screws directly to the plate. This decreases the risk of screw pullout and increases the stability of these constructs in osteoporotic bone. Intramedullary, rods are also commonly used in osteoporotic bone because they allow sharing of the biomechanical force placed on the bone between the rods (load sharing) while the rods are anchored to undamaged bone far above and below the fracture site. This allows the transfer of some of the energy encountered by the bone to these uninjured proximal and distal locations until the fracture has healed. Again, making sure that these locking screws fully engage both cortices of the bone is important in order to maximize the stability of these screws in osteoporotic bone .
67.4
Lower extremity fractures
Lower extremity fragility fractures can be devastating to function and independence and can further compromise balance in the elderly, making them even more prone to falls and additional fractures. Upward of 40% of patients with a hip fragility fracture take a step down in mobility function once they have fully healed from their fracture, meaning that if they walked independently, they now need a cane, or if they previously used a cane, they now need a walker. In addition, partly due to these changes in balance and mobility, a substantial portion of patients who were living independently prior to their lower extremity fracture require assisted living or even a long-term skilled facility after healing from their injury. Early surgery to prevent complications with limited mobility such as skin breakdown, respiratory compromise, and pneumonia is important as is early mobilization after surgery if that is possible in order to minimize sarcopenia and muscle loss which may further compromise patient strength, balance, and function .
One of the goals of lower extremity surgery in fragility fracture patients is to allow immediate weight bearing, if at all possible . Biomechanical and animal studies demonstrate that early weight bearing is beneficial to healing as the osteocytes in the bone respond to mechanical signals created by weight bearing and can modulate bone formation through a RANK ligand stimulatory pathway . Certainly, in the treatment of hip fractures, fractures of the femoral shaft, and fractures of the tibial shaft, immediate weight bearing as tolerated should be standard protocol or a different surgical approach or hardware should be used to allow this to occur. Fractures of the metaphyseal and periarticular portions of bone, including the distal femur, the tibial plateau, the distal tibia, and the ankle, do not allow for immediate weight bearing. Fractures of the diaphyseal/shaft portion of the bones that extend into these regions may also result in limitations on weight bearing. Bone in these areas is predominantly trabecular and fracture stability depends upon some healing of this trabecular bone prior to allowing weight bearing. Bearing weight too soon in these unstable fractures can lead to the loss of the fracture reduction and hardware breakage and failures. Unfortunately, it is not uncommon for these fractures to limit weight bearing for 8–12 weeks after treatment, either operative or nonoperative, and for some comminuted unstable fracture patterns in the super elderly where healing can be slow, those limits on weight bearing may extend to 6 months or more. It is also very difficult to make a patient with poor balance partial weight bearing. In general, with the elderly they can either function weight bear as tolerated or bed to chair transfers but are not capable of restricted partial weight bearing because of the significant increase in energy expenditure required to maintain those restrictions . In addition, accumulating evidence demonstrates poor compliance with weight-bearing restrictions in most adult patients, both young and elderly .
With more than 340,000 hip fractures occurring annually in the United States, and similarly high frequency in countries around the world, significant literature exists regarding the treatment of hip fragility fractures. In 2014 the American Academy of Orthopedic Surgeons (AAOS) issued evidence-based guidelines for the management of hip fractures in the elderly . Again, the goal of treatment is to allow immediate weight bearing after surgery, so the type of fixation depends upon the fracture pattern and the stability of the fracture reduction. Subcapital femoral neck fractures that are essentially nondisplaced and impacted into valgus positioning compress at the fracture site with every weight-bearing step and are inherently stable fractures; however, in geriatric patients due to poor bone stock, displace without surgery 79% of the time compared to displacement of this fracture pattern in young adults only 20% of the time . Fixation with cannulated screws that have smooth shafts and threaded portions that extend beyond the fracture and engage the bone in the femoral head and subchondral region of the hip allow for impaction of the fracture zone while maintaining rotational stability of the fracture during early healing and preventing the head from displacing into varus which is an unstable position. Recommendations regarding the number of screws and the orientation pattern of the screws vary, but generally three screws are used . A recent randomized clinical trial investigated the use of a dynamic hip screw versus these cannulated screws for the treatment of these fractures and no difference was seen in outcomes for patients treated by either device, making this fixation technique a viable option for treatment as well .
Displaced femoral neck fractures disrupt the blood supply to the femoral head and in the geriatric population, strong evidence exists to recommend arthroplasty for the treatment of these fractures as open reduction and treatment with screws as described nondisplaced fractures carry a 40% reoperation rate with it. In these patients, either a hemiarthroplasty or a total hip arthroplasty can be performed. In the early 2000s, literature developed recommending the treatment of younger, active, independent patients with a total hip arthroplasty because it decreased the rate of reoperation for the development of later arthritis. In less active patients over the age of 75, no difference was seen with the type of arthroplasty (hemi vs total) . More recent literature demonstrates that this benefit may be modulated by both careful selection of patients (active, fully ambulatory, independent) and surgeon experience with total hip arthroplasty. Large databases looking at outcomes showed little difference between hemiarthroplasty and total hip arthroplasty in general practice, leaving the decision to the surgeon . Monopolar head versus bipolar head showed no significant functional or outcome differences. In terms of surgical approach use for the placement of the arthroplasty, while dislocation rates are slightly higher using the posterior approach in contrast to the anterolateral approach, again surgeon experience should determine the approach used. In patients with significant osteoporosis, direct anterior approach to the hip carries with it an increased risk of intraoperative fracture of the femur and again depends highly upon surgeon experience for its success . Cementing of the implant stem in the femur is supported by moderate evidence overall and more recent literature suggests that cementing should be considered in patients over the age of 80 and those with severe osteoporosis. Press-fit stems in the femur depend upon rapid bone ingrowth into the porous-coated portions of the stem, and for patients with significant osteoporosis, compromise of the stability of the implant, subsidence of the implant, and periprosthetic fractures can occur, sometimes necessitating reoperation .
Intertrochanteric fracture fixation again depends upon the fracture pattern and the inherent stability of the fracture. Stable intertrochanteric and basicervical (at the base of the femoral neck) fractures can be fixed by either a dynamic hip screw and side plate or a cephalomedullary nail (short or long). Clinical trial showed no difference in outcomes between two-hole and four-hole side plates for the dynamic hip screws in the setting of stable fracture patterns . If the lateral wall of the intertrochanteric region is involved in the fracture or the fracture is significantly comminuted, plate screw devices cannot maintain stability of the fracture fragments. Moderate evidence suggests that cephalomedullary nails should be used with unstable intertrochanteric hip fractures . In these constructs a large sliding lag screw is placed as close to the anatomic central axis of the femoral head and into the subchondral bone as possible as this is often the area with the strongest bone to grab onto the hardware threads. Clinical evidence shows that if a measurement from this central anatomic point on the head to the tip of the sliding hip screw is >25 mm, the risk of the hardware cutting out of the bone and hardware failure increased . The sliding hip screws in these constructs allow compression to occur at the fracture site with weight bearing, which increases the mechanical stability of the stabilization and can facilitate fracture healing. While these sliding hip screws can protrude through the lateral cortex of proximal femur as the fracture fragments compress, these screws are generally well tolerated and require no additional intervention. Occasionally, a symptomatic protruding screw can contribute to trochanteric bursitis and local steroid injection can sometimes help with the symptoms. Rarely, these screws are exchanged for shorter less prominent screws once the fracture has healed, but this is reserved for the most symptomatic younger and more active patients as it requires an additional surgery. Hardware is not completely removed even if symptomatic because the osteoporotic bone remains at high risk for a secondary fracture through screw tracts, particularly in the femoral neck, with complete hardware removal. Strong evidence supports the treatment of subtrochanteric (those occurring distal to the lesser trochanter) and reverse obliquity fractures (where the most distal portion of the fracture line exits along the lateral aspect of the femoral cortex) with cephalomedullary nails and the fracture patterns and extent require long nails to be used as plating of these fractures, even with locking plates, carries a higher rate of failure . Fractures of the femoral diaphysis are generally fixed with femoral nails [antegrade or retrograde (through the knee) depending upon the location of the fracture] as these load-sharing devices allow for early weight bearing and some mechanical stimulation of the fracture site to facilitate healing. With the placement of locking plates can be used for the treatment of femoral diaphyseal fractures but often require extensive exposure in order to obtain the necessary multiple screw fixation above and below the fracture to provide stability, often recommended as eight cortices of screw contact above and below the fracture. For that reason, intramedullary nails are more commonly used; however, access to implants around the world may dictate treatment options .
Atypical femur fractures that are associated with long-term use of potent antiresorptive agents (bisphosphonates and denosumab) or genetic diseases (hypophosphatasia) carry with them some unique operative and fracture-healing challenges. These fractures represent a unique subset of subtrochanteric fractures, with a short and often transverse fracture pattern extending from the lateral to the medial cortex of the femur and in a region that is dominated by cortical bone, rather than the long oblique fracture patterns seen in subtrochanteric fractures typically associated with osteoporosis. These fractures may be nondisplaced, presenting either in a patient on antiresorptive with hip and thigh pain with weight bearing or incidentally on X-ray in a similar patient population. In a nondisplaced fracture where the fracture line can be seen in the lateral cortex of the femur, often with an accumulation of subperiosteal fracture callus surrounding the fracture line and creating the described lateral cortex prominence. Controversy exists as to treatment of these nondisplaced fractures. Protected weight bearing for 6–8 weeks until pain improves and longer term avoidance of repetitive impact (running) or high impact (jumping) activities is recommended . These fractures can be extremely slow to heal, so in patients with weight-bearing pain, CT scan or MRI can be helpful in defining the extent of the fracture across the proximal femur. Practitioners have used the principles of treatment for stress and pathologic fractures to guide the timing of surgery, where if pain is not improved after 6–8 weeks of protected weight bearing or the fracture line extends ≥50% of the width of the femur, surgical stabilization is pursued. Patient anatomy with either an excessively varus-angled or excessively valgus-angled femoral neck relative to the shaft, and/or possess and atypical bow shape to the femoral diaphysis as well as the presence of sclerotic callus along the endosteal surface of the femur adjacent to the fracture site can make placement of a standard long femoral nail challenging. These fractures may require smaller diameter nails or piriformis entry reconstruction nails (in contrast to the commonly used greater trochanteric entry nails) in order to avoid further damage to the bone and fracture site. With severe bowing or abnormality to the bone, short nails or proximal femoral locking plates contoured to the bone may need to be used for fixation but carries with it a high complication and failure rate. Local treatments at the fracture line site such as curettage of the fracture line, placement of unicortical compression plates at the fracture site adjacent to a femoral nail, and bone grafting at the fracture site remain inconclusive in their efficacy to improve healing rates or time to healing .
Distal femoral fractures that involve the supracondylar and intercondylar regions of the knee are generally fixed with long periarticular locking plates that place several long fixed-angle locking screws in multiple planes at the level of the femoral condyles and then standard bicortical and locking screws more proximal to the fracture in the femoral diaphysis. These fractures are inherently unstable, and weight bearing is generally delayed on the effected limb until some early healing and fracture callus has been demonstrated. In some patients, this delay in weight bearing can last for several months. A meticulous reduction of the articular surface must be attempted in order to preserve limb length and joint function; however, if later arthritis develops, a total knee arthroplasty can be placed through the healed fracture . In older geriatric patients with severely comminuted distal femoral fractures or severe preexisting osteoarthritis, a resection of the involved fractured bone and a distal femoral replacement using the hinged rotating platform total knee commonly used in oncology resection procedures can be used to allow for immediate weight bearing and function. In patients requiring a distal femoral replacement in this setting of clearly compromised bone quality, the implanted stems should be cemented to allow for immediate weight bearing. Tibial plateau fractures and distal tibial (plafond and pilon) fractures are also periarticular fractures that require fixation with locking plate constructs and limited weight bearing until some healing has occurred . Skin compromise can be an increased challenge in the tibia as plates can be subcutaneous, particularly on the medial side of the bone and patients with diabetes and peripheral vascular disease can have difficulty healing both the fracture as well as the skin overlying the hardware. Some severe distal tibial fractures in these compromised patients, particularly if they are open fractures, may be best treated with below the knee amputation. Nondisplaced periarticular fractures of the knee and ankle may be treated nonoperatively with a cast, brace, or boot but again weight bearing is restricted until some healing has been demonstrated.
67.5
Upper extremity fractures
The consequence of upper extremity fractures long term on activities of daily living is often underestimated. Both the shoulder and the elbow are important in allowing the arm to reach the top of the head (for hair care), the mouth (for eating), and the perineum (for bathrooming) and mobility limitations can make it difficult for patients to independently dress, feed, and perform hygiene care for themselves. The goal of care for these fractures is to maintain as much functional motion as possible in order to facilitate these activities of daily living. In addition, data from the Women’s Health Initiative reinforced the need for patients with upper extremity fractures to be evaluated and treated for osteoporosis as long-term follow-up data showed that out of all of the types of fragility fractures, a fracture of the distal radius was most predictive of an additional fracture in the next decade with a fracture of the proximal humerus being the second highest predictor . This is partially because many of the upper extremity fractures happen in independent and younger geriatric patients who continue to live for many years, while half of all patients who suffer from a fragility fracture of the hip have died within 10 years of that fracture.
Proximal humerus fractures are an extremely common fragility fracture and many can be treated nonoperatively. Treatment choice depends upon the anatomic location and pattern of the fracture as well as the activity level of the patient. The majority of the proximal humerus fractures occur at what is referred to as the surgical neck of the humerus, just distal to the rotator cuff insertions, in the highly trabecular metaphyseal portion of the bone. Most of these fractures have just two parts: the humeral head with the attached rotator cuff and the humeral shaft, and many are minimally displaced and impacted in a valgus position which is inherently stable. These patients can be treated with sling immobilization and allowed early motion of the shoulder. Patients need to be encouraged to immediately start moving the wrist, elbow, and hand in the effected arm to prevent stiffness and help with swelling. After approximately 2 weeks in the sling, most patients are comfortable enough to begin gentle motion of the shoulder as well and can initiate gentle gravity-assisted circles and pendulums and begin physical and occupational therapy to prevent shoulder stiffness. Sleeping with the head and torso elevated at least 30 degrees can help one significantly with pain in the early treatment stages of these fractures. When a patient lies flat, gravity pushes the arm into the chest wall and the fracture side often exacerbating pain. With 30 degrees of shoulder and torso elevation, gravity now pulls the weight of the arm gently away from the fracture site which can improve pain. Vascular and nerve injuries can sometimes occur even with simple patterns of proximal humerus fractures so a thorough exam of the entire upper extremity, including the wrist and hand, must be performed at the time of injury .
Fractures that are displaced into a collapsed varus position (more toward a right angle) or that involve additional fragments of the greater tuberosity and lesser tuberosity are unstable fractures that require open reduction and fixation. Fixed-angle locking plates allow restoration of the proximal humeral anatomy and the placement of multiple screws into the humeral head and the subchondral bone helps maintain stability of the fracture, even in rotation . The area of bone between the humeral tuberosities (where the rotator cuff muscles attach) is often devoid of much bone. The subchondral bone of the humeral head, much like that of the femoral head in hip fractures, often contains the strongest and best quality bone that can grab hardware and help to maintain the reduction during healing of the fracture. Screws into the humeral head must be advanced as close to the articular surface as possible in order to take advantage of the strength of this subchondral bone, but penetration of the screw tips through the joint surface remains one of the greatest risks of this technique . Fractures of the anatomic humeral neck which essentially separate the articular surface from the remainder of the humerus, or fractures that extend through the articular surface itself generally require arthroplasty prosthetic replacement of the joint. If both the anatomic neck of the humerus and the humeral tuberosities are involved in a severely comminuted fracture, it can be challenging to maintain the stability of the prosthetic replacement, even with suture or hardware augmentation repair of the tuberosities to return them to their anatomic positions . Newer techniques using the reverse shoulder that stabilizes the bearing surface in the unfractured scapula and glenoid allowing the mobile surface to be transferred to the fractured proximal humerus and make up for deficiencies in bone and rotator cuff function has had some success.
Fractures of the humeral diaphysis also are commonly treated nonoperatively. Patients are initially placed into a coaptation splint which restricts both elbow and shoulder motion until some of the swelling has subsided and then they transferred to a fracture brace for the extent of healing . A careful neurovascular exam of the arm must be performed because injury to the radial nerve, which passes intimately to the bone in the upper arm, can be damaged by these fractures and result in a nerve palsy. If palsy occurs, nerve function generally returns in 6–8 weeks, but splinting of the hand is required during this time to avoid contractures. Occasionally, this nerve palsy develops in the first few weeks after the injury, so repeat neurovascular exam at follow-up visits is also required. If operative fixation is required for this fracture, careful identification and protection of the radial nerve must first be done before treatment with a locking plate or humeral nail . Again, sleeping with the torso elevated 30 degrees for the first few weeks after injury can help with pain from the fracture as can a cuff and collar suspension. Slings can sometimes push up at the elbow, exacerbating pain at the fracture site. Cutting the elbow portion of the sling out and positioning the sling so that the elbow in dependent and the hand portion is closer to overlying the heart can recreate a cuff and collar suspension from a standard sling.
Distal humerus fractures commonly involve severe comminution of the bone with extension of the fracture into the elbow joint. Damage to the ulnar and radial nerves can occur with these fractures and great care must be taken during operative fixation of these fractures to adequately mobilize and protect these nerves. If nerve palsy occurs from this injury, it generally returns after several weeks but in the interim the patient may require bracing of the hand and wrist to prevent stiffness and contracture due to the nerve palsy. Nonoperative care is reserved for minimally displaced fractures in patients with significant medical or cognitive comorbidities with a goal to allow for the beginning of motion as early as possible. Hinged elbow braces, casts, and splints can be used to provide stability until some healing has occurred . In younger, healthier, more active, and more independent patients, surgery is generally indicated. Open reduction and internal fixation with locking plates has become the standard of care but still carries with it a significant complication rate of nearly 30% with elbow stiffness, fracture and incision healing compromise, and infection occurring most commonly. Parallel plating along the medial and lateral columns of the distal humerus with precontoured locking plates or 90–90 locking compression plating has demonstrated success in the treatment of these fractures . Complex fractures with severe comminution into the joint, extremely poor bone quality, or preexisting significant elbow osteoarthritis sometimes necessitate the placement of a total elbow arthroplasty. Total elbow arthroplasty requires compliance with lifelong 10 lb (4 kg) weight-lifting restrictions. Complications, including infection, implant loosening, and periprosthetic fracture, necessitate that this choice should be restricted to carefully selected patients. Total elbow arthroplasty in these selected patients can provide excellent range of motion and function in the setting of otherwise unreconstructable fractures .
Distal radius fractures are the most common fractures in postmenopausal women and the second most common fragility fracture. Almost 200,000 distal radius fractures occur annually in the United States and the Women’s Health Initiative study identified this fracture type as the fragility fracture most likely to predict a future fracture. Distal radius fractures are often the first fragility fractures for patients and it is important to engage all patients over age 50 or younger postmenopausal women who suffer from a distal radius fragility fracture with a workup for osteoporosis, including a DXA scan . Immediately after a distal radius fracture, patients also experience an increased risk for hip fracture, probably reflecting their high fall risk . Many of these fractures can be treated nonoperatively with a closed reduction and casting. Careful neurovascular exam and skin exam must be performed at the time of injury as damage to the median, radial, and ulnar nerves can occur. Open fractures, sometimes only with a small puncture hole visible, are not uncommon with this injury and require additional treatments with antibiotics and sometimes surgical irrigation of the fracture site to prevent infection. In the early phases of fracture immobilization, both the wrist and the elbow need to be immobilized in order to prevent motion through the fracture during supination and pronation of the forearm. This is often accomplished during the first week or two with a sugartong splint prior to the patient being placed in a short-arm cast. Once early healing is demonstrated on X-rays and exam (usually 4–6 weeks after the fracture), the cast can be changed to a distal radius brace that still protects the fracture but allows daily skin care. The most common distal radius fracture occurs after a fall on an extended hand and can result in significant comminution of the osteoporotic dorsal cortex of the radius, making it difficult to maintain a reduction. The decision to proceed with surgery depends upon the degree of angulation and displacement as well as the involvement of the articular joint surface . In addition, the decision for surgery must involve a discussion with the patient about functional recovery and functional expectations. Rates of surgery for geriatric distal radius fractures vary dramatically by geographic region and training expertise of the consulting surgeon, reinforcing the need for a full discussion with the patient regarding functional expectations after healing .
The most common surgical options for geriatric patients with distal radius fractures involves treatment with dorsal or volar locking plates in order to maintain reduction positions while healing occurs. Plating allows for a visualization, reduction, and stabilization of the disrupted articular surface if the fracture enters the joint. Both volar and dorsal plating bridge the fracture and return the bone alignment to a more anatomic position in an attempt to optimize hand and wrist function after healing. Due to the comminution of bone, particularly along the dorsal cortex from the injury, bone graft and bone graft substitutes are often used at the time of surgery to help restore length and structure to the bone. Dorsal plating carries an increased risk of loss of reduction and irritation of the extensor tendons (up to 30% of cases) when compared to volar plating, but volar plating is not without its risks given its proximity to the median nerve and flexor tendons . External fixators with percutaneous pins to align the fracture fragments were commonly used in the past to help maintain bone length and alignment during early healing by using ligamentotaxis of the adjacent soft tissues to help position the bone fragments. This is used less frequently due to the risks of fracture and infection at the pin sites, as well as the dangers to the patient from the large pins and bars extending from the arm surface. These can still be used quite effectively in the correct patient population. Placement of a spanning dorsal locking plate from the third metacarpal to the radial diaphysis can accomplish the same ligamentotaxis and maintenance of bone length and can be removed after 12 weeks to allow motion at the wrist . With all manners of fracture stabilization, early finger motion and elevation of the wrist and hand is encouraged to minimize stiffness and swelling.
67.6
Pelvis and sacral fractures
Fractures of the pelvic ring, which includes pelvic and sacral fractures, can cause significant pain and mobility limitations for patients and are common fragility fractures after a fall. Because the pelvis forms a ring, most fractures resulting from a fall result in at least two fracture locations within this ring. Fractures of the anterior pelvis involving both the superior and inferior pubic rami are sometimes isolated to that region of the pelvis; however, any complaints of buttock or low back pain in the setting of a pelvis fracture warrant an evaluation for sacral involvement . Pelvic and sacral fractures can be difficult to see on standard anterior-posterior (AP) pelvis X-rays that are a part of a fracture workup in a geriatric patient after a fall. What first presents as hip pain with no fracture seen on X-ray may in fact be a nondisplaced pelvic ring fracture, or even a fracture that is visible on the X-ray but goes unrecognized because it does not occur immediately adjacent to the hip joint. CT scan can be very helpful in the diagnosis of pelvic ring fractures if suspicion is high for injury. Although most pelvis and sacral fractures are treated nonoperatively, patients and providers often fail to recognize these as osteoporosis-associated fragility fractures and fractures that carry a 1-year mortality rate almost identical to hip fractures . Nonoperative treatment involves weight bearing as tolerated with a walker, but pain can make walking and transitions from lying to sitting and sitting to standing difficult for several weeks until some significant healing has occurred. Patients can also benefit from a raised commode seat during this time because significant forces travel through the pelvis and hip joint when rising from the toilet causing pain and effecting both balance and strength until the patient has healed.
Acetabular fractures in the geriatric population have been increasing in incidence as the population of older adults continues to grow. While acetabular fractures are traditionally associated with higher energy injuries such as a fall from a height or a traffic accident, older patients with osteoporosis can suffer from an acetabular fracture from a low-energy fall from standing. These falls drive the femoral head into the pelvis and can cause through and around the acetabulum. Again, these fractured regions of the pelvis are often managed nonoperatively because poor bone quality does not allow for stabilization of an anatomic reduction . The surgeries associated with acetabular injuries can be very physiologically stressful with long operative times, blood loss, and significant surgical dissection required in order to place adequate hardware, making this challenging for many geriatric patients who already have low functional demands. As with hip fractures, early mobilization, with protected weight bearing if at all possible, is advised to prevent the complications associated with bed rest. For patients who do proceed with surgery, open reduction and internal fixation with plate/screw constructs, delayed total hip arthroplasty, and acute total hip arthroplasty are all treatment options . Locking plates have not demonstrated a biomechanical or outcomes advantage in the treatment of acetabular fractures in the elderly and can be an impediment to the placement of long screws necessary to obtain stable purchase in osteoporotic bone. As with the open treatment of other fractures in osteoporotic bone, bone graft may be needed to stabilize gaps left by severe comminution of fracture sites and restore normal bone lengths. Allowing the fracture to heal with deformity followed by delayed total hip arthroplasty or an acute total hip arthroplasty requires modified hardware and techniques that are not typically used during standard total hip arthroplasty for arthritis. Press-fit cups with multiple screws reaching into the adjacent bone, megacups with screw fixation and cement augmentation, and cage reconstructions with cemented cups are all techniques that can be used to treat the geriatric patient with an acetabular fracture . Regardless of the surgery chosen, surgeon experience and availability of appropriate hardware and equipment is necessary for these highly complex surgeries.
67.7
Spine fractures and elective spine surgery
Vertebral compression fractures are the most common fragility fractures with over 750,000 occurring annually in the United States. Almost two-thirds of these fractures go unrecognized acutely as the patient recovers following a short period of back pain and does not realize that they have had a fracture. Once a patient has had a vertebral fracture, they are five times more likely to have another vertebral fracture and twice as likely to fracture their hip in the future compared to a peer patient with no fragility fracture. It is very important to look for occult vertebral compression fractures on chest X-rays, CT scans, and lateral vertebral assessment during DXA scan in order to pick up these patients who are at high risk for additional fragility fractures and enter them into osteoporosis treatment pathways . Patients with symptomatic fracture vertebral compression fractures are initially treated nonoperatively with analgesic medications and activity modifications. Bracing can sometimes help patients avoid flexion positions with their backs that place additional stress on the fractured vertebral body, causing increased pain. Vertebral compression fractures are not unstable fractures structurally, so bracing is not required and braces may not be well fitted or tolerated in the geriatric population. Once they are able to tolerate activity and exercise, patients benefit from gentle exercises that strengthen core abdominal and paraspinal muscles and balance exercises. Compression fractures can create a localized kyphosis, placing the patient’s head in front of their central axis over their feet. This leans the patient slightly forward and can be very disruptive to balance without an assistive device or a compensatory flexion of the pelvis in order to balance the patient’s head once again over the axis with their feet. This imbalance can significantly increase fall risk and physical therapy and fall risk reduction instruction can be an important part of fracture recovery .
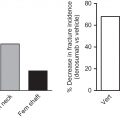
Vertebroplasty and kyphoplasty for osteoporotic compression fractures remain controversial, but may be beneficial in select patients. Both procedures involve image-guided passage of a needle and cannula through the vertebral pedicle and injection of PMMA cement into the vertebral body to connect the fractured portions of the vertebral body together and relieve pain by stopping micromotion at the fracture site. Vertebroplasty utilizes a high-pressure injection of the cement into the bone and fracture site, while kyphoplasty utilizes a fluid-filled balloon to create a cavity within the vertebral body and fracture site to allow for a low-pressure fill of the defect. The goal of these procedures is to provide pain relief and functional improvement by stabilizing the fracture, and potentially more rapid rehabilitation . Randomized studies by both Kallmes and Buchbinder did not show a significant long-term difference between surgically treated and sham-treated patients. Both studies were criticized for their patient inclusion criteria and may not have had a patient population with truly acute and actively mobile fractures. Subsequent studies that prospectively randomized acute fracture patients to vertebroplasty or nonoperative care showed improvements in acute pain and that advantage was maintained at 1 year . Further research to define the optimal patient is needed.
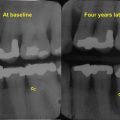
Fixation in elective spine surgery for the treatment of spinal stenosis, spinal instability, and deformity is more prone to failure at the bone–implant interface in patients with osteoporosis. In addition, poor bone quality can result in compression fractures in vertebrae adjacent to fused segments of the spine. The use of larger diameter pedicle screws, hydroxyapatite-coated pedicle screws, and cement augmentation through fenestrated pedicle screws with PMMA or calcium-based cements can help with this issue . Longer fusion constructs involving more levels of hardware placement both above and below the involved area of the spine may be needed to improve hardware stability while the fusion mass is healing . There is an increased interest in preoperative treatment of high-risk spine patients with anabolic agents such as teriparatide, abaloparatide, or romosozumab in order to build bone and strengthen bone prior to elective spine surgery in the osteoporotic patients, but more research is needed to guide the length of treatment needed to provide demonstrative benefit to the patient that is directly related to the spinal surgery and surgical risks such as hardware pullout and adjacent compression fractures.
67.8
Periprosthetic fractures
Bone immediately adjacent to joint replacement prostheses can become increasingly weak due to a shift in mechanical loading forces to other areas of the bone and prosthetic replacement. This change in mechanical force patterns, called stress shielding, can exacerbate a localized osteoporosis immediately adjacent to the implants. Fractures around the implants can occur with falls and commonly involve these areas of stress shielding. Periprosthetic fractures are rapidly growing in incidence as the population with joint arthroplasty devices is both increasing in number and aging. These fractures are underrecognized as osteoporosis-associated fragility fractures and patients are not commonly referred on for the treatment of their osteoporosis with appropriate medication . Treatment of these fractures varies by anatomic location, fracture pattern, remaining stability of the implant, and overall patient bone quality. Intramedullary rods passed through the notch gap in a knee implant, locking fixed angle plates and screws with cerclage wires that surround the area of bone that contains the arthroplasty stem, and revision implants are used as needed to stabilize these fractures, preserve the implant if possible, and restore mobility . Periprosthetic fractures in the geriatric population may require several months of limited mobility until healing has occurred and can be devastating to the independence and self-care capacity of a patient.
References
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree