Bilateral and contralateral lymphatic spread is common; retrograde spread to retropharyngeal lymph nodes has been reported (21, 34, 56).
The deeply infiltrating nature of most cancers correlates with the high frequency of lymphatic metastases at presentation (80% of patients overall, with bilateral spread in 30%).
The American Joint Committee on Cancer staging system (1) for carcinoma of the oropharynx is shown in Table 18-1.
Base of tongue cancers have a worse prognosis than those in the oral tongue because of greater size at diagnosis, more frequent spread to adjacent structures, and higher rate of lymphatic spread. However, stage for stage, they may have a prognosis similar to that of oral tongue cancers (27).
Exophytic or surface tumors respond well to irradiation alone; ulcerative, endophytic cancers that are partly or completely fixed require surgery (11, 12, 13 and 14, 21, 45).
Overall, treatment results for base of tongue cancer, when all stages are considered, appear to be best for combinations of surgery and irradiation, intermediate for surgery alone, and worst for irradiation alone.
Surgical resection consisting of mandibulotomy and neck dissection is recommended for T1 and T2 cancers.
Radical neck dissection yields data for determining the need for postoperative irradiation, which is recommended for patients with disease more extensive than stage N1 or extracapsular extension.
Tumors of the lower base of the tongue that involve the valleculae and extend inferiorly to the supraglottic larynx and pyriform sinus may be controlled by partial glossectomy and subtotal supraglottic laryngectomy, or partial laryngopharyngectomy with preservation of voice (53, 59).
Conditions required for a subtotal supraglottic laryngectomy include no gross involvement of pharyngoepiglottic fold, preservation of one lingual artery, resection of less than 80% of the
base of the tongue, pulmonary function suitable for supraglottic laryngectomy, and medical condition suitable for a major operation.
Locoregional control (LRC) is approximately 48% with surgery alone (22).
TABLE 18-1 AJCC Classification for Carcinoma of the Oropharynx and Hypopharynx | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
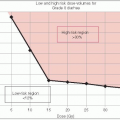
Small T1 and T2 base of tongue tumors without significant infiltration on surface, or exophytic T2 and T3 lesions of the glossopharyngeal sulcus (glossopalatine sulcus), are controlled by high-dose radiation, with LRC of 70% (12).
Large, unresectable base of tongue cancers that cross the midline and infiltrate and fix the tongue are often irradiated palliatively to achieve as much tumor regression as possible.
Surgery combined with irradiation is best suited for larger tumors that extend beyond the base of the tongue or infiltrate and partially fix the tongue.
Adjuvant irradiation should be used routinely for resectable T3 and T4 base of tongue cancers to reduce the likelihood of recurrence (52, 59).
Doses of 60 Gy and bilateral fields covering the primary site and upper necks are necessary because of the significant primary tumor burden and high rate of contralateral and bilateral lymphatic spread.
LRC ranges from 60% to 78% with the combined approach.
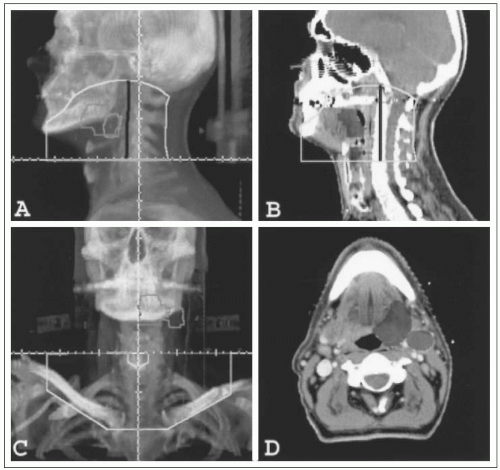
Irradiation portals for base of tongue cancer should encompass the primary tumor and locoregional extensions.
Portals should extend superiorly to the base of the skull and floor of the sphenoid sinus to include the retropharyngeal lymphatics, anteriorly to include the faucial arch and a portion
of the oral tongue, inferiorly to include the supraglottic larynx, and posteriorly to include the posterior cervical triangle.
The primary tumor and both sides of the upper neck are irradiated through opposing lateral fields.
Both sides of the lower neck are irradiated through a single anteroposterior field, with a midline block at the junction between the upper lateral and low-neck fields to prevent spinal cord injury (Fig. 18-2).
Supine patients with bite block or thermoplastic immobilization receive daily treatment of all fields.
The spinal cord is shielded after 40 to 45 Gy, and the posterior cervical triangles are boosted with 9- to 12-MeV electrons to spare the underlying spinal cord.
Tissue compensators ensure dose homogeneity and prevent excessive dose to the supraglottic larynx.
After 40 to 45 Gy with low-energy megavoltage beams, the remaining dose may be delivered with high-energy x-rays to concentrate the dose centrally and reduce the dose to the parotids, mandible, and temporomandibular joints.
After 60 Gy, the fields are reduced to encompass only the primary tumor and may be weighted to the side involved by tumor.
The boost dose after 60 Gy may be delivered by a submental electron beam or a low-energy photon beam field.
Doses to the primary tumor and palpable lymph nodes are 65 to 75 Gy delivered in 6.5 to 7.5 weeks; doses for elective irradiation of subclinical microscopic lymphatic metastases should be at least 50 Gy.
The role of interstitial implants remains undefined.
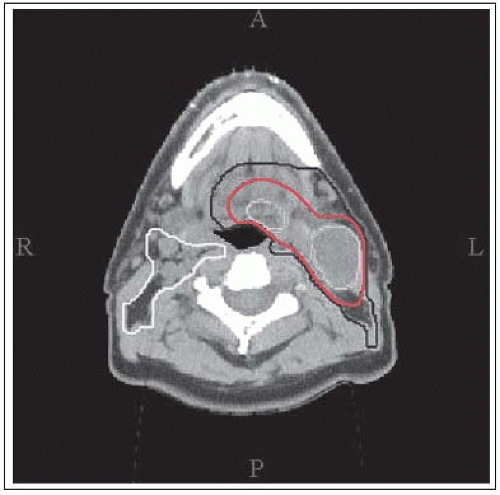
CTV1 (high-risk volume):
Includes all primary and nodal gross tumor volume (GTV) with 10-mm margin.
For T1/T2 disease truncate clinical target volumes (CTVs) inside the hyoid bone.
For T3/T4 truncate CTVs just outside hyoid bone.
Exclude soft palate when not involved.
May truncate air, skin, and bone if not invaded by tumor.
CTV2 (intermediate-risk volume):
Includes 5-mm margin on CTV1 and ipsilateral nodal levels IB, II to V (excludes VI).
Includes medial retropharyngeal inferiorly nodes to the superior edge of the hyoid bone.
Nodal CTV2 of the involved neck extends up to the base of the skull.
CTV2 on ipsilateral involved neck can optionally be defined as CTV3 between the transverse process of C1 and the jugular foreman.
Nodal CTV2 extends inferiorly to sternoclavicular joint when the whole ipsilateral neck is treated with intensity-modulated radiation therapy (IMRT).
May truncate air, skin, and bone if not invaded by tumor.
CTV3 (low-risk volume):
Includes contralateral uninvolved nodal disease.
Excludes contralateral nodal levels V and IB if primary tumor is confined ipsilaterally.
Includes medial retropharyngeal nodes inferiorly to the superior edge of the hyoid bone.
Inferior margin extends to 2 cm above sternoclavicular joint.
Superior margin extends to the transverse process of C1.
May truncate air, skin, and bone if not invaded by tumor.
Figure 18-3 is an example of IMRT target delineation in a patient with T2N2a left-sided base of tongue cancer.
Xerostomia (moderate to severe) occurs in approximately 75% of patients treated with conventional beam arrangement. IMRT can significantly reduce this complication exponentially, at 4% per Gy of parotid mean dose (9).
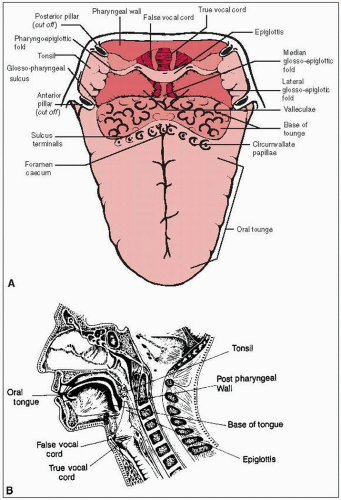
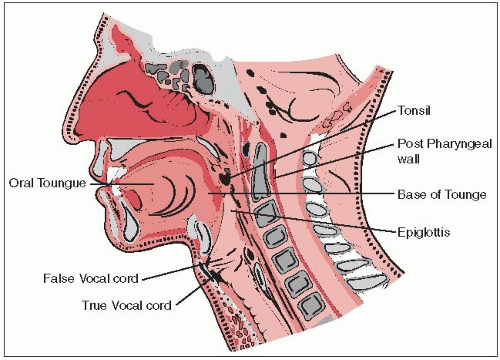
The oropharynx is the posterior continuation of the oral cavity; it communicates with the nasopharynx above and the laryngopharynx below. It can be subdivided into the palatine (faucial) arch and the oropharynx proper (Fig. 18-4).
The palatine arch, a junctional area between the oral cavity and the laryngopharynx, is formed by the soft palate and the uvula above, the anterior tonsillar pillar and glossopalatine sulcus laterally, and the glossopharyngeal sulcus and the base of the tongue inferiorly.
The retromolar trigone has been included in the structures of the faucial arch, although it is actually located within the oral cavity. Its apex is in line with the tuberosity of the maxilla (behind the last upper molar). The lateral border extends upward into the buccal mucosa; medially it blends with the anterior tonsillar pillar, its base formed by the distal surface of the last lower molar and the adjacent gingivolingual sulcus (36).
The lateral walls of the oropharynx are limited posteriorly by the tonsillar fossa and the posterior tonsillar pillar (pharyngopalatine folds). These pillars are folds of mucous membrane that cover the underlying glossopalatine and the pharyngopalatine muscles (36). Deep to the lateral wall of the tonsillar fossa are the superior constrictor muscle of the pharynx, the upper fibers of the middle constrictor, the pharyngeus and stylopharyngeus muscles, and the glossopalatine and pharyngopalatine muscles. The tonsillar fossa continues into the lateral and posterior pharyngeal walls.
The tonsillar fossa and the faucial arch have a rich, submucosal lymphatic network that is laterally grouped in four to six lymphatic ducts; these ducts drain into the subdigastric, upper cervical, and parapharyngeal lymph nodes. Submaxillary lymph nodes may be involved in lesions of the retromolar trigone, buccal mucosa, or even base of the tongue.
Tonsillar fossa lesions tend to be infiltrative, often involving the adjacent retromolar trigone, soft palate, and base of the tongue. At Washington University, St. Louis, Missouri, primary
tumor was confined to the tonsillar fossa in only 5.4% of 384 patients; 65% had involvement of the soft palate, and 41% had extension into the base of the tongue (47).
Tumors of the faucial arch can be superficially spreading, exophytic, ulcerative, or infiltrative; the last two types are frequently combined. They become extensive, involving the adjacent hard palate or buccal mucosa, in less than 20% of patients.
Mandibular involvement was noted in 14% of 110 patients with primary retromolar trigone carcinomas (7).
Tumors of the tonsillar fossa have a high incidence of lymph node metastases (60% to 70%). Although most are found in the subdigastric lymph nodes, midjugular chain, and submaxillary lymph nodes (in lesions extending anteriorly), 5% to 10% involve the posterior cervical lymph nodes (46).
Metastases in the low cervical chain occur in approximately 5% to 15% of patients with upper cervical lymph node involvement.
The incidence of metastatic lymph nodes in the neck increases with tumor stage. Lymphatic progression is systematic, proceeding from upper jugular to lower cervical (33).
Contralateral lymphadenopathy in tonsillar tumors is noted in 10% to 15% of patients with positive ipsilateral lymph nodes. This is seen more frequently when the primary tumor extends to or beyond the midline.
Retromolar trigone, tonsillar pillar, and soft palate lesions have an overall metastatic rate of approximately 45%. Initially, the most common site of nodal involvement is the jugodigastric lymph nodes. Approximately 10% of patients have submaxillary lymph node involvement. Tumors of the retromolar trigone, anterior faucial pillar, and soft palate rarely metastasize to the posterior cervical lymph nodes. Contralateral spread is infrequent (10%).
Sore throat is the most common symptom.
Difficulty in swallowing or pain in the ear is related to the anastomotic-tympanic nerve of Jacobson.
Trismus may be a late manifestation if the masseter or the pterygoid muscle is involved.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree