Procedural safety recommendations
Surgical field
Use of disposable drapes (not textile cloth)
Operating room
Closed door, access restriction, prevent of possible spills
Caregivers
Disposable impervious gown and shoe covers; double gloves, the outer to be changed every 30 min; eye goggles; high-power filtration mask
Environment
Ventilation, smoke evacuator over surgical field
Residue
Rigid dedicated containers during and 48-h after HIPEC
15.5 Costs
The International Classification of Diseases, 9th revision, Clinical Modification (ICD-9-CM) does not include the many surgical procedures distinctive of peritonectomy, except visceral resections. Neither does it include coding for abdominal- cavity hyperthermic perfusion with antiblastic drugs. Therefore, the Hospital Discharge Form, a data-collection tool for patients discharged from public and private health-care structures in Italy, does not adequately evaluate the economic commitment of CRS plus HIPEC. Furthermore, the form reports no more than six procedures, and in many cases, it is difficult to prioritize procedures, which most of the time exceed six. In specialized literature, interest in HIPEC costs is significantly lower than interest in its medical outcome, although issues concerning this matter have been raised in recent years. Baratti et al. [24] assessed the cost of > 380 CRS plus HIPEC procedures performed at the Milan National Cancer Institution from 1995 to 2008, comparing it to reimbursement obtained in the last 2 years. The authors calculated that the average cost for each individual hospitalization was €36,015.89 (range €28,435.24–82,189.08), with a total cost in 2007–2008, of €2,665,185.29. Total reimbursement in those 2 years was €804,483.30, resulting in a loss of €1,861,301.99. It is therefore clear that in Italy, a project for treating PC does not receive adequate financial and institutional support.
In fact, the Italian Classification of Diagnosis-Related Groups (DRGs) does not include CRS or HIPEC. Therefore, hospitals that treat patients with PC must bear this economic deficit. We analyzed the costs in our hospital and determined the cost of the material needed for CRS was €2,792.51 per procedure (without considering staplers), for a diagnostic laparoscopy was €553.14, and for the kit for a single HIPEC procedure was €1,098. Considering mean operative times, the cost of OR personnel (surgeons, anesthesiologist, nurses) was €3,434.12. Moreover, the cost of the OR itself, excluding personnel, and the sterilization procedure was €2,048.86. Evaluating mean ICU and hospital stay, the cost was €13,247.45 per patient. Finally, the cost of preoperative examination of each patient was €1,229.45. The hospital must assume this economic deficit. In France, where the health system is similar to Italy, a similar test was conducted [25]. The authors calculated that the average cost for a single hospitalization was €39,358 (costs for HIPEC administration were excluded). Reimbursement from the health system was €20,485 on average, with a loss of €18,873 per patient. Over a period of 2 years, the deficit was €1,400,000, which is significantly lower than the deficit calculated for Italy. Costs are closely connected to surgery but also to the duration of the hospital stay and therefore to any postoperative complication [25].
The CRS plus HIPEC technique is sometimes criticized, despite expanding scientific evidence of its value, because of its high costs. An Australian analysis [26] compared the cost of CRS plus HIPEC with the cost of lifetime palliative care for PC patients. The analysis of the cost per life-year saved allowed the authors to consider HIPEC as a cost-effective treatment for patients with PC from appendiceal tumor, CC, pseudomyxoma peritonei (PMP), and malignant peritoneal mesothelioma (MPM), and possibly also from other etiologies. Cost analyses also emphasize the need to centralize treatments in tertiary referral centers. In analyzing the per CRS plus HIPEC procedure costs for PC from advanced OC origin in centers with more or less experience, Bristow et al. indicated that there is an incremental cost-effectiveness ratio of US $17,149 per quality-adjusted life year gained with referral to an experienced center [27].
15.6 Data Collection and Study Protocols
HIPEC is now the standard of care in treating PMP, MPM, and CRC with limited peritoneal involvement [28]. With regard to colorectal carcinomatosis, there are different attitudes in international guidelines: the US National Cancer Institute (NCI) does not even mention HIPEC among treatment options, whereas French guidelines recommend it. An ongoing randomized trial, protocol IOVCAR- CRC-1-2012, in Italy evaluates the role of CRS plus HIPEC compared with systemic chemotherapy in resectable CRC PC. HIPEC is in the evaluation phase for PC from OC and GRC, but it is probably useful in particular settings [28]. Two ongoing trials in Italy are evaluating the effectiveness of CRS plus HIPEC in PC from OC: The CHORINE study (Cytoreduction and HIPEC in the treatment of OvaRIaN cancer) is a prospective randomized trial that evaluates stage III unresectable epithelial ovarian/tubal cancer with partial or complete response after first-line neoadjuvant chemotherapy with three cycles of carboplatin (CBDCA) and paclitaxel. The trial compares CRS versus CRS plus HIPEC, both treatment modalities being followed by three cycles of CBDCA and paclitaxel. The Italian Hyperthermic Intra-peritoneal Chemotherapy in Ovarian Cancer Recurrence (HORSE) trial is a prospective randomized study that compares CRS with or without HIPEC in the first recurrence of OC, if platinum sensitive. Further trials are necessary to improve evidence.
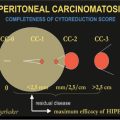
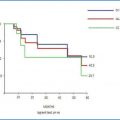
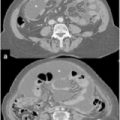
Most trials supporting the importance of CRS plus HIPEC are multi-institutionally based [29–35]. This indicates the importance of study protocols for data collection. A protocol must be adequately organized, structured, and shared by the various participating centers. The objective is to evaluate what impact this treatment has on patient survival in terms of disease-free (DFS) and overall (OS) survival. A fundamental and specific element of the HIPEC research protocol is timing the investigation of the procedure. For example, in order to assess the effectiveness of CRS plus HIPEC in patients with OC, this therapy may be studied in the various stages of the cancer’s natural history. Patient inclusion and exclusion criteria for the study must be shared among the various centers. Sampling size required to achieve the specified objectives must be established. Therefore, the minimum number of cases each center has to present for data collection should be established. Data to be reported and made available in the patient’s medical history file must be established and shared. Presurgery data (past treatment, histological diagnosis, any relapse), intrasurgery data (PCI, CC score, procedures performed, chemotherapy drug used for HIPEC), and postsurgery data (morbidity and mortality, follow-up) must be assessed.
The informed consent issue is of critical importance. Patients must be provided with a thorough oral explanation and with written documentation. The patient must be fully aware of the study objectives and the reason he/she was selected to be enrolled. Enrollment shall take place only after the informed consent is signed, and all patient agreement must be on a voluntary basis. It must be specified that if the patient does not want to be enrolled in the study, he/she will still receive the best possible medical treatment based on available scientific evidence. Data confidentiality must be guaranteed, and it must be made clear to the patient that the study protocol was assessed and approved by an ethics committee.
References
1.
2.
Deraco M, Kusamura S, Laterza B et al (2006) Cytoreductive surgery and hyperthermic intra-peritoneal chemotherapy (HIPEC) for the treatment of pseudomixoma peritonei: ten years experience in a single center. In Vivo 20:773–776PubMed
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree