Chapter 29 Orbital, Ocular, and Optic Nerve Tumors
Based on the incidence rates from the Surveillance, Epidemiology, and End Results Program of the National Cancer Institute, the American Cancer Society estimated that approximately 2390 new cases of all types of primary ocular and orbital malignant tumors were diagnosed in the United States in 2008.1 This demonstrates the rarity of ocular malignant tumors. Uveal melanoma is the single most common malignant tumor of the eye and orbit and makes up nearly 70% of all cancers of these tissues.1 Irradiation is used in the management of many ocular and orbital cancers, as well as in the management of several benign ocular processes. Understanding the pathophysiologic processes of ocular cancers and the results of radiation treatment can guide treatment recommendations.
Etiology and Epidemiology
Choroid Melanoma
Uveal melanoma is the most common primary malignant intraocular neoplasm.1 It is thought to arise from melanocytes of the uveal tract and in the United States occurs in approximately 1500 patients per year.1,2 Uveal melanomas are more common in lightly pigmented persons and are infrequent in nonwhite races. The average age at the time of diagnosis is 60 years in most large series,2–4 and the disease occurs with equal frequency in men and women. The tumors are rarely bilateral. Factors proposed as increasing the risk for the development of uveal melanoma are prolonged sustained sunlight exposure5,6 and lighter-colored irises.5,6 Certain diseases may predispose to melanoma, including xeroderma pigmentosum, which is an inherited disorder of DNA repair; oculodermal melanocytosis,7 in which the ocular surface and the uveal tract are hyperpigmented; and dysplastic nevus syndrome. There are some reports implying a possible rare genetic predisposition, although most melanomas occur as sporadic tumors.
Optic Nerve Tumors
Meningioma
Optic nerve sheath meningiomas arise from the meningothelial cap cells of arachnoid villi and can develop anywhere along the course of the optic nerve from the globe to the prechiasmal intracisternal optic nerve. They may be unilateral, bilateral, or multifocal. Patients with type 2 neurofibromatosis are predisposed to bilateral or multifocal lesions.8 Meningiomas from other locations can also extend to involve the optic nerve.
Optic nerve sheath meningiomas are more common in women. Dutton’s meta-analysis estimates a female preponderance of 61%.9 The typical age at presentation is 40 years. Bilateral cases appear to have an earlier age of onset.
Glioma
Optic nerve gliomas account for 1% to 5% of intracranial gliomas and 4% of orbital tumors. They occur most frequently in children, with 75% in the first decade and 90% in the first two decades of life.10 Approximately 25% of patients with optic gliomas also have type 1 neurofibromatosis. These tumors are increasingly being seen as markers of enhanced risk in patients and their families for the subsequent development of central nervous system tumors.11
Orbital Tumors
In a recent report of 1264 consecutive patients with orbital masses, 33% of patients had malignant lesions. Rhabdomyosarcoma was the most common malignant tumor in children, representing 3% of all orbital masses, and lymphoma was the most common malignant tumor in older patients, representing 10% of cases.12 In one large series, metastatic breast cancer comprised 4% of these lesions.
Lacrimal Gland Tumors
Lacrimal gland tumors are rare. The gender distributions are equal and patient age ranges from 10 to 73 years (mean of 46 years).13 Most of these lesions are malignant, with adenoid cystic carcinoma and mucoepidermoid cancer being the two most frequent ones. Benign pleomorphic adenomas also occur.
Lymphoma
Primary orbital lymphomas are rare and account for less than 1% of all lymphomas diagnosed.14 Lymphomas in the orbit can occur anteriorly in the conjunctival tissues or in the retrobulbar region. Patients with lymphoma at other sites can also present with eye involvement in the course of their disease.
Primary intraocular lymphoma may have malignant lymphoid cells involving the retina, vitreous, or optic nerve head, with or without concomitant central nervous system involvement. The incidence of primary intraocular lymphoma has been increasing over the past 15 years, in both immunocompetent and immunocompromised patients.15 The cause of this increased incidence is unknown. This is a disease of persons in their fifties and sixties, occurring more often in men than women.
Metastatic Tumors
The most common primary tumor to metastasize to the orbit is breast cancer.12 Other orbital metastases have been reported to occur from neuroblastoma, lung cancer, renal cell cancer, and prostate cancer.
Similarly, choroidal metastases are most frequently of breast cancer origin, followed by lung cancer. In one report of 420 patients, the uveal metastasis arose from a primary cancer of the breast in 196 patients (47%), the lung in 90 patients (21%), the gastrointestinal tract in 18 patients (4%), the kidney in 9 patients (2%), the skin in 9 patients (2%), the prostate in 9 patients (2%), and other cancers in 16 patients (4%).16
Benign Ocular Conditions
Pterygium
Most pterygia are located nasally and occur in patients aged 20 to 50 years.17 They are more commonly encountered in warm, dry climates or in patients who are chronically exposed to outdoor elements or smoky and dusty environments. Ultraviolet light exposure appears to be the most significant factor in the development of pterygia. Heredity may also be a factor.
Pterygia represent a degeneration of the conjunctival stroma with replacement by thickened, tortuous elastotic fibers.18 Activated fibroblasts in the leading edge of the pterygium invade and fragment Bowman’s layer. Pterygium development resembles actinic degeneration of the skin.
Pseudotumor
Orbital pseudotumor, or idiopathic orbital inflammatory syndrome, is a nonspecific inflammatory process of unknown etiology that may mimic orbital lymphoma.19 Because the disease mimics infectious or neoplastic processes, these must be ruled out. Autoimmune disease, endocrinopathies, and granulomatous processes must be excluded, as well as local infection with secondary involvement of the orbit, such as sinusitis and subperiosteal abscess. The diagnosis of pseudotumor is vague and remains one of exclusion.
Graves’ Ophthalmopathy
The pathogenesis of Graves’ ophthalmopathy is thought to be an autoimmune one in which activated T lymphocytes invade the orbit and stimulate glycosaminoglycan production in fibroblasts, resulting in tissue edema, lymphocyte infiltration, and marked enlargement of the extraocular muscles.20 Because lymphocytes and fibroblasts are sensitive to radiation, retrobulbar irradiation has been advocated as a treatment. The ophthalmopathy typically goes through three phases: progression, followed by stabilization, and perhaps some improvement. Residual signs of ophthalmopathy after the disease has reached a plateau are thought likely to be the result of fibrosis and other tissue changes rather than persistent inflammation.
Macular Degeneration
Age-related macular degeneration (AMD) is the leading cause of blindness in patients older than 65 years.21 The progressive loss of central vision is usually consequential to an atrophic process involving the retinal epithelium and choriocapillaries in the macula, which is classified as dry AMD. The wet form of AMD is an exudative process with subretinal neovascularization. Wet AMD generally progresses to destructive disciform scarring of the macula, with fibrovascular scars involving the choroid and sensory retina. Patients develop poor visual acuity.
Prevention and Early Detection
Because of the rarity of all ocular tumors, no prevention or early detection methods have been developed for most tumor types. However, in children born into a family with known retinoblastoma, early and careful ophthalmologic evaluation is warranted. Genetic counseling and evaluation of the siblings of patients with retinoblastoma is important, given the high hereditary likelihood.22 After the diagnosis of unilateral retinoblastoma, routine evaluation of the uninvolved eye is indicated because of the increased risk of contralateral disease (see Chapter 69).
Biologic Characteristics and Molecular Biology
Ocular Melanoma
Biologic characteristics that predict outcomes in patients with ocular melanoma include tumor cell type, tumor size, tumor location, and extension of the tumor outside the sclera.23 Cell type is discussed in the pathology section of this chapter, with patients with spindle cell tumors having a better survival rate than those with epithelioid cell tumors. Recent data suggest that specific chromosomal aberrations within the tumor may be associated with the length of survival. Many tumors are treated by means other than enucleation, and because biopsy is rarely performed, the cell type is often unknown.
Survival rates are adversely affected by increased size of the uveal melanoma. Although the earlier literature had various size classifications, the Collaborative Ocular Melanoma Study (COMS) has established a standard size classification.24–26 Small melanomas are 1 to 3 mm thick and less than 16 mm in largest dimension. Medium-sized melanomas are 3 to 8 mm thick and less than 16 mm in largest dimension, and large melanomas are more than 8 mm thick or more than 16 mm in largest dimension (Table 29-1).
TABLE 29-1 Various Other Definitions of Choroidal Melanoma Size
| Size | Measurement |
|---|---|
| Small | 1.5-2.4 mm height and 5-16 mm diameter |
| Medium | 2.5-10 mm height and <16 mm diameter |
| Large | >10 mm height and >16 mm diameter |
Prognosis is also affected by the location of the anterior tumor margin. Tumors located anterior to the equator of the eye in the anterior choroid or ciliary body have a worse prognosis than those located more posteriorly.23 Extraocular extension of a uveal melanoma has poor prognostic implications.24
Orbital Lymphoma
The biology of these tumors varies with the histologic classification within the Revised European-American Lymphoma system or the Working Formulation.27,28 Stage and histologic type play the most significant roles in outcome for orbital lesions.
Primary intraocular lymphoma is believed to be a subset of primary central nervous system lymphoma. It is usually a diffuse large B-cell non-Hodgkin’s lymphoma, and, less commonly, it may be T-cell lymphoma. Because pathologic diagnosis can be difficult, flow cytometry is often done to demonstrate monoclonal populations of B lymphocytes. Immunohistochemical assessments have also been used to demonstrate expression of BCL-6 and MUM1.29 These two markers have been revealed in systemic diffuse large B-cell lymphoma. Molecular analysis detecting immunoglobulin gene rearrangements and ocular cytokine levels showing elevated interleukin-10 (IL-10), with a ratio of IL-10 to IL-6 greater than 1, are helpful adjuncts for the diagnosis of intraocular lymphoma.14,30
Orbital Pseudotumor
The histopathologic type varies, and attempts to refine and subdivide patients have been advocated. The histopathologic spectrum of idiopathic orbital inflammation is typically nondiagnostic and diverse, ranging from the typical diffuse polymorphous infiltrate to the atypical granulomatous inflammation, tissue eosinophilia, and infiltrative sclerosis. One report suggested dividing this condition into three principal types: lymphoid, granulomatous, and sclerosing types.31 Several authors have endorsed the exclusion of reactive lymphoid hyperplasia and defined pseudotumor as a mixed inflammatory infiltrate with fibrosis of varying degrees.19
Pathology and Pathways of Spread
Skin Cancers
Basal cell cancers are seen in 90% of patients, followed by squamous cell cancers in 10%. For patients with squamous cell cancer, involved regional lymph nodes have been reported in as many as 24% of patients.32 Lymph node involvement is more common for larger tumors, recurrent tumors, and those with perineural invasion. Patients with recurrent lesions or perineural invasion may have tumor cells spread more peripherally than is clinically apparent. This may require wider radiation fields. Tumors located in the embryologic fusion planes of the face have been found to be more deeply infiltrating. This area around the medial canthus may affect the depth of treatment necessary for a successful outcome.
Ocular Melanoma
Uveal melanomas arise from melanocytes that are of neuroectodermal origin. Melanoma cells have a large nuclear to cytoplasmic ratio, prominent or multiple nucleoli, and frequent mitotic figures. Tumors are generally classified as composed of either spindle cells or epithelioid cells.33 Spindle cells have a fusiform shape and less pronounced atypia, whereas epithelioid cells are larger and more ovoid in shape and have more anaplastic characteristics. Uveal melanomas are classified as spindle cell melanomas if they are composed of only spindle cells, mixed cell melanomas if they contain both spindle cells and epithelioid cells, and epithelioid cell melanomas if they contain predominantly or exclusively epithelioid cells. Occasionally, the cells within the melanoma undergo necrosis, and these tumors are classified as necrotic melanomas.
The prognosis is more favorable in spindle cell melanoma, intermediate in mixed cell tumors, and poorest in epithelioid or necrotic melanoma. Other negative prognostic indicators include tumor dimension, thickness, and location of the anterior tumor margin.33 Melanomas tend to be slow-growing tumors, but the rate of growth can be quite variable. More rapidly growing tumors, which have a worse prognosis, tend to be anaplastic and composed of epithelioid cells.
At the time of diagnosis, most posterior uveal melanomas are confined inside the sclera of the eye. Extraocular extension of the melanoma can occur through emissary canals, through which normal ocular structures such as vessels and nerves enter and exit the sclera, and generally not by atrophy or thinning of the sclera. Extraocular extension is classified as microscopic or gross (visible on gross inspection), occurs in 8% to 14% of eyes harboring a melanoma, and is associated with a worse prognosis.34
Metastatic disease occurs in less than 3% of patients at the time of initial diagnosis. The most common sites of involvement include hematogenous spread to the liver and the lung. More unusual sites of spread include bone, skin and subcutaneous tissue, and brain and spinal cord tissue. Lymph node involvement was noted in 10% of patients dying from metastatic disease within the COMS.35
Choroidal Metastasis
The most common pathologic type is adenocarcinoma from the breast or non–small cell lung cancer. Most patients have other sites of metastatic disease. Disease extent can be localized to the choroid. The average number of lesions seen in the choroid in one large series was two.16 In this situation, involvement of the opposite choroid can occur in as many as 50% of patients. Orbital metastases can occur and are typically unilateral.
Orbital and Ocular Lymphoma
A wide range of non-Hodgkin’s lymphomas have been described involving the orbit and globe. In patients with orbital lymphomas, most of the lesions are of B-cell origin and classified as low or intermediate grade by the Working Formulation.36 The most common subtype of ocular adnexal lymphoma is a mucosa-associated lymphoid tissue (MALT) lymphoma. Intraocular lymphomas are usually of the aggressive, diffuse, large B-cell type.15
Orbital Meningioma
Meningiomas spread along paths of least resistance, remaining confined to the subarachnoid or intradural space of the intraorbital optic nerve. The tumor may invade the dura, adjacent orbital tissue, muscle, bone, and globe. These tumors may traverse the optic canal and affect the intracranial segment of the optic nerve or adjacent structures. Orbital meningiomas have histologic features similar to those of intracranial meningiomas. Most lesions demonstrate concentric formations of spindle cells or ovoid meningothelial cells with sheets of polygonal cells separated by vascular trabeculae.37
Lacrimal Gland Tumors
Pathologic findings are typically those of adenoid cystic cancer, followed by mucoepidermoid cancer and adenocarcinoma. Outcome seems to be related to the presence of necrosis, hemorrhage, perineural invasion, and high mitotic count.38
Optic Nerve Glioma
In the pediatric form of the disease, the cell of origin for optic nerve gliomas is unknown. Optic nerve gliomas are classified as grade I astrocytomas (pilocytic astrocytomas) in the World Health Organization (WHO) classification of gliomas, are slow growing, and do not tend to metastasize.39 Optic nerve gliomas develop in stages, from generalized hyperplasia of glial cells in the nerve to complete disorganization with loss of neural landmarks within the nerve and nerve sheath. A reactive meningeal hyperplasia may be incited, making it difficult to distinguish a glioma from a perioptic meningioma.
In pediatric patients with optic nerve glioma, 10% to 38% have type 1 neurofibromatosis, and 15% to 40% of children with neurofibromatosis 1 have an optic glioma.40 When bilateral, the lesions are pathognomonic for neurofibromatosis 1.
In the adult form of the disease, the optic nerve gliomas are more likely to be diffusely infiltrative, including astrocytoma (WHO grade II), anaplastic astrocytoma (WHO grade III), or glioblastoma multiforme (WHO grade IV).41 Nuclear atypia, mitoses, endothelial proliferation, and necrosis are potential histologic features.
Clinical Manifestations, Patient Evaluation, and Staging
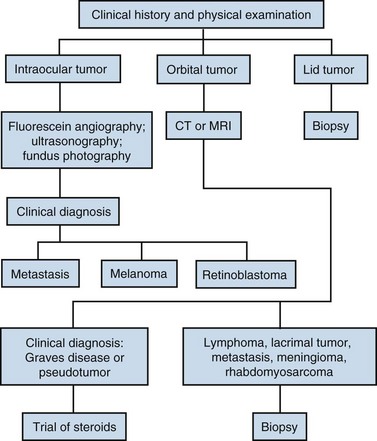
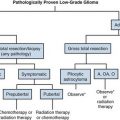
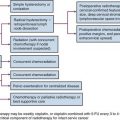
The diagnostic algorithm for ocular, orbital, and lid tumors is given in Figure 29-1.
Ocular Melanoma
The diagnosis of melanoma is based primarily on ophthalmoscopic appearance and ancillary testing. The tumor typically appears as a unilateral, solitary, elevated, dark brown or gray, variably pigmented, dome-shaped mass (Fig. 29-2). Orange pigment (lipofuscin) is often found on the surface of the tumor and is thought to represent increased metabolic activity.42 Retinal detachment may be present and is more likely in larger tumors.
The initial ophthalmologic workup includes fundus photography, fluorescein angiography, and ultrasonography of the globe (Fig. 29-3). These tests facilitate making a correct diagnosis and are also useful in following the lesions for growth or regression after treatment. In a large prospective trial, 645 of 647 patients who underwent enucleation for melanoma were confirmed to be such at pathologic evaluation. Two of the patients had adenocarcinoma.24 In eyes with opaque media secondary to cataract or vitreous hemorrhage, ultrasonography of the globe and MRI of the orbits can allow an accurate diagnosis. Biopsy of a lesion suspicious for an ocular melanoma is used only in cases of diagnostic uncertainty. In patients requiring biopsy, histopathologic and immunohistochemical assessments can be useful in confirming the diagnosis.
To assess disease extent, obtain a general history and perform a physical examination with attention directed to skin lesions, weight loss, the lungs, and the liver. History of a prior cancer would indicate the possibility of a metastatic lesion in the eye rather than a primary melanoma. The most frequent site of metastasis is the liver, so the workup generally includes liver enzyme levels. Elevated levels will prompt evaluation with radiographic imaging. This approach was recently reported to have low sensitivity but high specificity and predictive value.43 Other sites of metastatic disease include the lung, and imaging with chest computed tomography (CT) scanning is most accurate for early detection of disease. The COMS report of sites of metastasis from melanoma demonstrated that sites included liver (91%), lung (28%), and bone (18%).43 Melanomas of the iris rarely metastasize. The brain is an infrequent site of metastasis; brain metastases were discovered in only 4% of patients at the time of death.44
Ocular Metastasis
Patients with uveal metastasis from breast cancer presented to ophthalmologists with visual symptoms in 93% of cases. Of 264 patients with uveal metastasis, 225 (85%) had choroidal metastasis, 8 (3%) had iris metastasis, 2 (<1%) had ciliary body metastasis, and 29 (11%) had metastasis in multiple uveal sites. Asymptomatic metastases were detected in 56% of patients in the opposite eye.45
Patients with orbital tumors more often present with diplopia, ocular motility disorder, and proptosis. Lesions are usually unilateral.46 Metastatic disease may be detected in a high proportion of the patients who present with this entity.
Orbital Lymphoma
Primary intraocular lymphoma is one of the most challenging intraocular tumors to diagnose. Cytologic examination of vitreal aspirates remains the gold standard for exclusion of neoplastic disease in patients with idiopathic uveitis.14 Patients with primary vitreous involvement should also have cerebrospinal fluid (CSF) examination and MRI of the brain and meninges. Eighty percent of patients with primary vitreous involvement have bilateral involvement.
Staging is done using the Ann Arbor staging system.47 A localized orbital lymphoma would be stage IeA.
Optic Nerve Meningioma
Patients typically present with visual loss, afferent papillary defect, color vision disturbance, visual field defect, proptosis, and optic disc edema. Ophthalmoscopic examination may reveal optic nerve head swelling, macular edema, nerve pallor, or choroidal folds. Optic disc swelling may also be observed. MRI is the procedure of choice for diagnosis of these lesions. Lesions appear slightly hypointense to brain and optic nerve tissue on T1-weighted images with fat suppression and gadolinium contrast. Thin CT scans may reveal regular or irregular thickening of the nerve sheath meninges. The nerve may appear normal in size or smaller as the result of circumferential compression or atrophy. Calcification has been described in 30% of patients and is associated with slower growth.48 Differential diagnosis includes sarcoid, demyelinating optic neuritis, orbital inflammatory disease, schwannoma, lymphoma, hemangiopericytoma, and optic nerve metastasis.
Usually these lesions are described as slow growing. Visual loss will generally occur in untreated eyes over a period of 5 to 10 years.49 Rapid growth has been observed during pregnancy, which may be mediated by hormone receptors.50 Other tumors have demonstrated rapid visual loss even in the absence of radiographic enlargement.
Optic Nerve Gliomas
Of optic pathway gliomas, 10% to 20% are confined to the orbit, with the remainder involving the intracranial compartment.10 MRI is the preferred method for evaluation of optic pathway glioma. Both the intraorbital lesion and its intracranial extent can be effectively characterized on MRI. When evaluating the orbit, gadolinium-enhanced T1-weighted images with fat saturation are effective at defining the extent of adult optic glioma. In the intracranial region, MRI provides superior evaluation of the optic nerve, chiasm, tracts, and geniculate body and of optic irradiation compared with CT scanning.
Orbital Pseudotumors
Patients present with proptosis, decreased ocular motility, soft tissue edema, and pain. Decreased visual acuity is not unusual. The condition may be unilateral or bilateral.51 CT scanning may reveal a unilateral focal or more diffuse mass. One review documented infiltration of the retrobulbar fat in 76% of patients, enlargement of the extraocular muscles in 57%, thickening of the optic nerve/sheath complex in 38%, contrast enhancement in 95%, and proptosis in 71%.52 Intracranial extension is unusual but has been documented in up to 8.8% of patients.53
Graves’ Ophthalmopathy
Signs and symptoms of Graves’ ophthalmopathy include bilateral exophthalmia, extraocular muscle dysfunction, diplopia, blurred vision, eyelid and periorbital edema, chemosis, lid lag and retraction, and compressive optic neuropathy. Imaging with CT scanning of the orbit will demonstrate changes consistent with enlargement of extraocular muscles, which are usually symmetric.54