The oral cavity consists of the upper and lower lips, gingivobuccal sulcus, buccal mucosa, upper and lower gingiva (including alveolar ridge), hard palate, floor of mouth, and the anterior two thirds of the mobile tongue.
The lips are composed of orbicularis muscle, which is covered by skin and mucous membrane on the inner surface. The transitional area between the two is the vermilion border. Blood is supplied through the labial artery, a branch of the facial artery. The motor nerve branches emerge from the facial nerve. The infraorbital branch of the maxillary nerve serves as the sensory nerve to the upper lip, whereas the lower lip is served by branches of the mental nerve, which originates in the inferior alveolar nerve. The commissure is partially innervated by the buccal branch of the mandibular nerve.
The upper gingiva is formed by the alveolar ridge of the maxilla, which is covered by mucosa and the teeth; it continues medially with the hard palate. The lower gingiva covers the mandible from the gingivobuccal sulcus to the mucosa of the floor of the mouth. It continues posteriorly with the retromolar trigone and above with the maxillary tuberosity. There are no minor salivary glands in the mucous membrane over the alveolar ridges (12).
The buccal mucosa is made up of the mucous membrane that covers the internal surface of the lips and the cheeks (buccinator muscle), extending from the line of attachment of the upper and the lower alveolar ridges to the point of contact of the lips (posteriorly) and the orbicularis (anteriorly). The masseter muscle lies posterior and lateral to the buccinator muscle. The blood supply comes from the facial artery. Sensory fibers are supplied by the buccal nerve, which is a branch of the mandibular nerve. The motor nerve to the buccinator muscle is derived from the facial nerve.
The floor of the mouth is bounded by the lower gingiva anteriorly and laterally, and extends to the insertion of the anterior tonsillar pillar into the tongue posteriorly. It is divided into halves by the lingual frenulum and is covered by a mucous membrane with stratified squamous epithelium. The sublingual glands lie below the mucous membrane and are separated by the midline genioglossus and geniohyoid muscles. The genial tubercles are bony protuberances occurring at the point of insertion of these two muscle groups on the symphysis (12). Muscles include the mylohyoid and the digastric muscles. The submaxillary glands are located on the external surface of the mylohyoid muscle between its insertions to the mandible. The submaxillary duct (Wharton’s duct) is approximately 5-cm long and courses between the sublingual gland and the genioglossus muscle; its orifice is in the anterior floor of the mouth, near the midline. The sensory nerve is the lingual nerve, a branch of the submaxillary nerve. The arterial supply is the lingual artery, a branch of the external carotid artery.
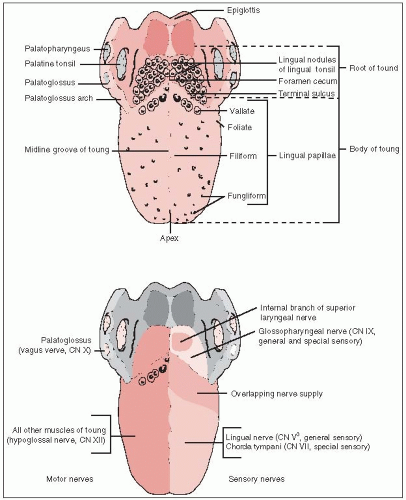
The tongue is a muscular organ composed of the styloglossus, hyoglossus, and hyoid muscles (Fig. 17-1). It is covered by a mucous membrane with stratified squamous epithelium. The circumvallate papillae, situated posteriorly with a V-shaped configuration, separate the base of the tongue from the mobile tongue.The oral tongue consists of the tip, dorsum, lateral
borders, and undersurface. The blood supply is the lingual artery, a branch of the external carotid artery (12). The sensory nerve is the lingual nerve, a branch of the maxillary nerve; the hypoglossal nerve is the motor nerve. The taste buds are innervated by the chorda tympani branch of the sensory root of the facial nerve.
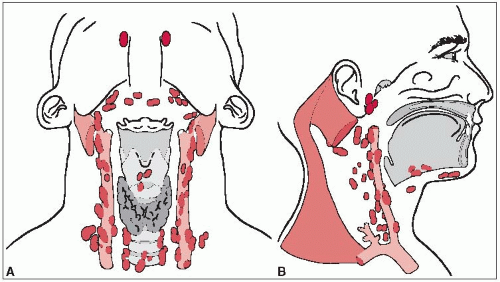
Lymphatics of the upper lip drain mostly to the submandibular lymph nodes; although the periauricular and the parotid lymph nodes also occasionally receive lymphatic channels from the upper lip. Lower lip lymphatics drain to the submandibular and, posteriorly, to the subdigastric lymph nodes. Lymphatics of the lower gingiva drain to the submandibular and subdigastric lymph nodes.
The first echelon of lymph node drainage of the floor of the mouth is to the submandibular and subdigastric lymph nodes.
Primary lymphatic drainage in the oral tongue is to the subdigastric and submandibular lymph nodes. Rouviere (13) described the lymphatic trunks that bypass this primary lymphatic drainage and go directly to the midjugular lymph nodes, which probably accounts for the relative frequency of metastatic lymph nodes in these locations (Fig. 17-2).
Lymphatic drainage of the buccal mucosa is primarily to the submandibular and the subdigastric lymph nodes.
Except for lesions arising from the tip of the tongue or extending across the midline, metastatic disease usually occurs in the ipsilateral cervical lymph nodes (10).
Lymph node involvement in lesions of the lip is relatively rare, although 5% to 10% of patients with clinically negative necks later develop lymph node metastases (11).
The incidence of lymph node metastases of the upper gingiva is 15% to 20% on presentation. There is approximately the same incidence of later development of clinical cervical lymph node metastases in initially clinically negative necks (10).
Approximately 30% to 65% of patients with cancer of the oral tongue and floor of the mouth have positive neck nodes on presentation. Of patients with clinically negative nodes, approximately 40% have pathologically positive nodes. Of all patients with negative nodes at presentation, the incidence of eventual development of a nodal metastasis without treatment is approximately 20% to 35%. Submental lymph nodes are involved in fewer than 5% of patients (10).
The incidence of bilateral lymph node involvement is relatively high for floor of mouth cancers because many lesions are near or cross the midline.
Five to ten percent of oral tongue cancers have bilateral lymph node metastases.
For cancers of the buccal mucosa, the incidence of positive cervical lymph nodes on presentation is 10% to 30%.
A variety of therapeutic measures is available for managing localized carcinomas of the oral cavity, including surgery, radiation therapy, laser excision, and combinations of these methods.
TABLE 17-1 American Joint Committee on Cancer Staging System for Lip and Oral Cavity Carcinomas | |||||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|