Malignant epidural spinal cord compression (MESCC) is a common neurologic complication of cancer. MESCC is a medical emergency that needs rapid diagnosis and treatment to prevent undergo emergent evaluation including magnetic resonance imaging of the entire spine. If MESCC is diagnosed, corticosteroids should be administered. Simultaneously, spine surgery and oncology teams should be immediately consulted. If indicated, patients should undergo maximal tumor resection and stabilization, followed by postoperative radiotherapy. Emerging treatment options such as stereotactic radiosurgery and vertebroplasty may be able to provide some symptomatic relief for patients who are not surgical candidates.
Malignant epidural spinal cord compression (MESCC) is a common complication in patients with advanced neoplasm. This disease occurs when cancer metastasizes to the spine or epidural space and compresses the spinal cord. Patients usually present with acute deterioration of neurologic functions such as inability to ambulate due to the mass effect of the metastatic diseases on the spinal cord. It is of paramount importance that the emergency department (ED) physician appreciate that MESCC is considered a treatable medical emergency, and that prompt management requires swift decision making with the collaboration of specialists such as oncologists, imaging and pathology specialists, and spine surgeons to avoid further deterioration of the patient’s neurologic functions. The management strategy for MESCC has evolved over the years, in part due to technological advancements in spinal instrumentation. Herein the authors present a primer for the ED team on the epidemiology, pathophysiology, and clinical presentation of MESCC, describe the role of medical and surgical approaches in managing this disease, and, based on recent data, recommend guidelines for use in clinical practice.
Epidemiology
In the United States, approximately 500,000 deaths are attributable to metastatic disease every year. Of all osseous sites, the spinal column is the most common location for metastatic deposits. Almost all major types of systemic cancer can metastasize to the spinal column. Evidence suggests that 2.5% to 5.0% of patients with terminal cancers have spinal involvement within the last 2 years of illness, and MESCC occurs in up to 40% of patients who have pre-existing nonspinal metastases. The incidence of MESCC varies by primary disease site and patient age. In adults, the most common primary tumor sites leading to MESCC are the prostate, breast, and lung, each accounting for 15% to 20% of all cases. Non-Hodgkin lymphoma, renal cell carcinoma, and multiple myeloma account for 5% to 10%, and the remainder of cases are due to colorectal sarcomas and other unknown primary tumors. In the pediatric population, neuroblastoma, Ewing sarcoma, Wilms tumor, lymphoma, and soft-tissue and bone sarcoma are the most common types that lead to spinal cord compression. The most common level of MESCC involvement is the thoracic spine (60%–78%), followed by the lumbar (16%–33%) and cervical spine (4%–15%); multiple levels are involved in up to 50% of patients.
Pathophysiology
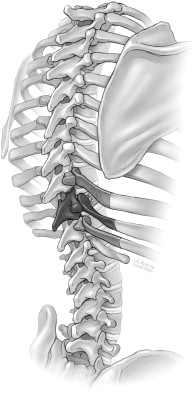
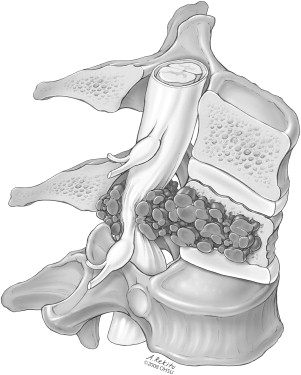
The most common way by which a primary malignancy spreads to the spinal column is through direct arterial embolization of tumor cells. Classically, it is believed that the valveless venous system in the spine (Batson’s plexus) may facilitate the hematogenous spread of the primary tumor to the spinal column. Recent evidence from animals suggests that arterial embolization may be a more important mechanism for metastasis. This seeding of tumor cells results in an expansive mass in the vertebral body. Compression of the epidural space can be caused by the continued growth and expansion of the mass itself or from retropulsion of bony fragments following collapse of a vertebral body weakened by tumor ( Fig. 1 ). Additionally, some tumors, especially lymphoma and neuroblastoma, can reach the epidural space by the direct growth of the paravertebral tumor into the spinal canal through an intervertebral foramen. Intramedullary, subdural or lepomeningeal metastases are rarely encountered causes of MESCC.
Animal studies and intraoperative observations have demonstrated that damage to the functional integrity of the spinal cord caused by MESCC is largely due to vascular compromise. First, the tumor mass or bony fragment impinges on the venous plexus surrounding the cord, which results in cord edema. The increased edema causes increased pressure on small arterioles, which leads to diminished capillary blood flow. Disruption of blood flow to the cord leads to white matter ischemia and, with prolonged compression, may eventually cause cord infarction. Production of vascular endothelial growth factor (VEGF) is also associated with spinal cord hypoxia. It has been proposed that steroid efficacy in the treatment of acute MESCC is at least partly due to down-regulation of VEGF expression.
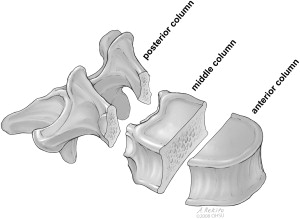
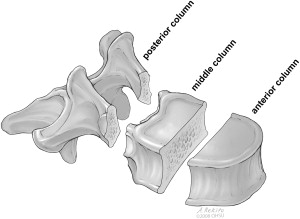
Another important mechanism by which metastatic tumors can harm the spinal cord is destabilization of the spinal column. Tumor invasion of the bony spine can lead to failure of the spinal column in the same way as a traumatic injury. Denis proposed a 3-column model for the evaluation of spine stability. In this model ( Fig. 2 ), the anterior column is composed of the anterior longitudinal ligament, the anterior annulus, and the anterior portion of the vertebral body. The middle column includes the posterior longitudinal ligament, the posterior annulus, and the posterior portion of the vertebral body. The posterior column includes those spinal structures that are posterior to the posterior longitudinal ligament. Disruption of 2 or 3 columns creates an unstable spine. It has been recognized that it is more common for a malignant lesion to involve the vertebral body and cause it to collapse. Findlay reported, in a small series, that more than half of patients with MESCC had a collapsed vertebral body. Collapse often involved the anterior and middle columns, hence spinal instability.
Pathophysiology
The most common way by which a primary malignancy spreads to the spinal column is through direct arterial embolization of tumor cells. Classically, it is believed that the valveless venous system in the spine (Batson’s plexus) may facilitate the hematogenous spread of the primary tumor to the spinal column. Recent evidence from animals suggests that arterial embolization may be a more important mechanism for metastasis. This seeding of tumor cells results in an expansive mass in the vertebral body. Compression of the epidural space can be caused by the continued growth and expansion of the mass itself or from retropulsion of bony fragments following collapse of a vertebral body weakened by tumor ( Fig. 1 ). Additionally, some tumors, especially lymphoma and neuroblastoma, can reach the epidural space by the direct growth of the paravertebral tumor into the spinal canal through an intervertebral foramen. Intramedullary, subdural or lepomeningeal metastases are rarely encountered causes of MESCC.
Animal studies and intraoperative observations have demonstrated that damage to the functional integrity of the spinal cord caused by MESCC is largely due to vascular compromise. First, the tumor mass or bony fragment impinges on the venous plexus surrounding the cord, which results in cord edema. The increased edema causes increased pressure on small arterioles, which leads to diminished capillary blood flow. Disruption of blood flow to the cord leads to white matter ischemia and, with prolonged compression, may eventually cause cord infarction. Production of vascular endothelial growth factor (VEGF) is also associated with spinal cord hypoxia. It has been proposed that steroid efficacy in the treatment of acute MESCC is at least partly due to down-regulation of VEGF expression.
Another important mechanism by which metastatic tumors can harm the spinal cord is destabilization of the spinal column. Tumor invasion of the bony spine can lead to failure of the spinal column in the same way as a traumatic injury. Denis proposed a 3-column model for the evaluation of spine stability. In this model ( Fig. 2 ), the anterior column is composed of the anterior longitudinal ligament, the anterior annulus, and the anterior portion of the vertebral body. The middle column includes the posterior longitudinal ligament, the posterior annulus, and the posterior portion of the vertebral body. The posterior column includes those spinal structures that are posterior to the posterior longitudinal ligament. Disruption of 2 or 3 columns creates an unstable spine. It has been recognized that it is more common for a malignant lesion to involve the vertebral body and cause it to collapse. Findlay reported, in a small series, that more than half of patients with MESCC had a collapsed vertebral body. Collapse often involved the anterior and middle columns, hence spinal instability.
Clinical presentation
Pretreatment neurologic status is by far the most important predictor of function after treatment. Therefore, it is highly desirable to diagnose MESCC before the patient develops any neurologic deficits. Most patients with MESCC have a known cancer diagnosis, emphasizing the importance of providing ED personnel with ready access to the prior medical records.
Pain is by far the most common presenting symptom of MESCC, occurring in approximately 83% to 95% of patients. Back pain caused by MESCC can take several forms and local and quality can vary. Initially, pain can be localized and confined to the region of spinal metastases, as the tumor stretches the periosteum or invades adjacent soft tissues. Radicular pain is also common among patients with MESCC and may occur when the tumor mass compresses or invades the nerve roots. Pain is usually worse at night when the patient is recumbent due to lengthening of the spine, or with Valsalva maneuver. A more ominous type of pain is mechanical back pain, which is made worse by movement and partially relieved with rest, may suggest spinal instability caused by vertebral body collapse. This can be a harbinger of subsequent neurologic deterioration. Hence the ED triage team must maintain equipoise when evaluating patients with the common complaint of back pain.
Motor deficit is the second most common symptom of MESCC (60%–85%), followed by sensory deficits (40%–80%). Patient complaints related to these symptoms are often vague. Weakness is frequently described as clumsiness or heaviness which can progress to paralysis. Motor deficit can involve upper and lower motor neurons. Upper motor neuron weakness is more likely to be symmetric, whereas lower motor neuron weakness is often asymmetric and affects the distal end of limbs first. Loss of ability to ambulate is usually due to weakness. Sensory deficits rarely occur before motor deficits or pain, and they usually begin distally and ascend as the disease advances. Increased susceptibility to falling can indicate the progression of motor and sensory deficits. Autonomic/sphincter dysfunction is typically a later finding (40%–60%). Among elderly patients, urinary retention is a more reliable sign of autonomic sphincter dysfunction than urinary incontinence. Sphincter dysfunction is a poor prognostic indicator for preservation or improvement of ambulatory status.
Diagnosis
A diagnosis of MESCC begins with obtaining a medical history and performing an appropriately focused general physical examination that is coupled with a comprehensive central nervous system (CNS) examination in patients suspected of having MESCC. New onset of back pain or neurologic symptoms such as symmetric weakness or paresthesia in a patient with known cancer should prompt further workup for MESCC. Imaging of the entire spine should be performed on any patient suspected of having MESCC not only to define the diagnosis but also to aid surgical or radiotherapy treatment planning. Magnetic resonance (MR) imaging is currently the gold standard imaging modal for assessing spinal metastatic disease. It is sensitive (93%) and specific (97%) for detection of MESCC and because multiple levels are frequently involved, imaging of the entire spine is highly recommended. Conventional computed tomography myelography techniques, with or without MR imaging are used if a patient cannot have MR imaging due to metallic implants.
Other imaging modalities are less useful than MR imaging. Plain films have insufficient sensitivity and specificity to make a diagnosis and they should not be performed; delaying MR imaging should be avoided. Radionuclide bone scans and positron emission tomography can detect MESCC but they are not as accurate as MR imaging due to lower resolutions.
Management
Patients with MESCC are usually affected by widespread cancer. Large retrospective studies have reported the median survival time for a patient with MESCC as 3 to 6 months. Treatment of spinal metastatic diseases including MESCC is mainly palliative. The goals are to control pain, avoid complications, and preserve neurologic function.
Corticosteroids
Corticosteroids are believed to delay neurologic deterioration by decreasing spinal cord edema and may also have an oncolytic effect on certain tumors, such as lymphoma and multiple myeloma.
As alluded to earlier, the efficacy of corticosteroids in managing patients with MESCC can partially be explained by a role in reduction of hypoxic spinal tissue VEGF expression. In a randomized trial, patients with MESCC were assigned to the treatment arm of a 96-mg intravenous (IV) bolus of dexamethasone followed by 96 mg/d orally for 3 days and a 10-day taper, versus no corticosteroids before radiotherapy. In the group treated with dexamethasone and radiation, ambulatory rates were higher than the group treated with radiation alone at 3 months and 6 months ( P <.05).
Although the efficacy of corticosteroids in delaying neurologic deterioration has been proven through these clinical data, the optimal loading and maintenance doses of corticosteroids have not been determined. Studies in animals have found a positive dose-dependent association of dexamethasone’s effect in reducing cord edema, which reaches a maximum effect at approximately 100 mg/kg. Vecht and colleagues, in the only randomized trial examining corticosteroid loading dose, reported no difference between an intravenous dexamethasone loading dose of 10 mg versus 100 mg with respect to pain reduction, ambulation, or bladder function. In this trial, the maintenance dose for all patients was 16 mg of oral dexamethasone per day.
Currently, due to lack of consensus, there are 2 widely used dosing regimens for steroids: a high dose (100 mg loading dose, followed by 96 mg/d) and a moderate dose (10 mg loading dose, followed by 16 mg/d). Some physicians advocate using motor symptoms to titrate the steroid dosage; that is, patients with rapidly progressive motor symptoms such as loss of ability to ambulate receive a high dose, whereas patients with minimal or nonprogressive weakness are treated with moderate doses.
Radiation
Palliative radiation therapy has been the standard care for patients with MESCC since the 1950s. The efficacy of radiotherapy in the preservation or improvement of neurologic function in patients with MESCC has been reported in numerous retrospective studies. Given a lack of equipoise regarding the efficacy of radiation therapy, a prospective, randomized controlled trial comparing radiation to no radiation would not be ethical. Despite general acceptance of the effectiveness of radiotherapy, the optimal dose and treatment regimen remains controversial. In conventional external-beam fractionated radiotherapy, the proximity of the spinal cord limits the dose that can be delivered. Various dose schedules have been tried for pain relief and reversal of compression. In a systematic review of various dose schedules, Sze and colleagues found no differences in pain relief between single fraction and multifraction radiotherapy. In 1 randomized study, Maranzono and colleagues, reported that a hypofractionation schedule resulted in no difference in back pain relief, maintenance of ambulation, and good bladder function rates among patients with MESCC receiving radiotherapy. In a retrospective study, post-treatment ambulatory rate and motor function improvement were not shown to be affected by the initial dose and number of fractions, but the rate of in-field recurrence was lower with protracted schedules. Because fractionation helps lower the risk of spinal cord injury, the recommendation based on these studies is to give a single fraction of 8 Gy to MESCC patients with limited survival expectations and 3 Gy in 10 fractions to all other patients. Most radiation oncologists adhere to typical schedules of 2.5 to 3.6 Gy delivered in 10 to 15 fractions.
Known predictors of outcome with radiation therapy are: (1) extent of functional limitation at the start of radiation; (2) tumor type; and (3) rapidity of onset of neurologic deficits. For example, 80% to 100% of patients who are still ambulatory when they begin radiation therapy maintain their ability to walk, whereas only one third of patients who are not mobile before treatment regain the ability to walk. Primary tumors most sensitive to radiation are lymphoma and seminomatous germ-cell tumor. Most solid tumors, such as breast, prostate, and lung cancers, are considered intermediately radiosensitive. Melanoma, osteosarcoma, and renal cell carcinoma are usually considered to be radioresistant. Although patients with radioresistant tumors may still experience substantial palliation with radiation, the chance of major functional recovery or long-term response to radiation is much less than that for patients with radiosensitive tumors. Patients who rapidly develop neurologic deficits are less likely to improve than those who develop deficits more gradually. This may reflect the fact that patients with sudden onset of paralysis have actually suffered an infarction of the spinal cord itself, which is not likely to improve even with relief of the compression. A much weaker predictor of outcome is the extent of subarachnoid block observed on MR imaging; an epidural metastasis that causes minor compression should have a better outcome than a large mass that encircles and deforms the spinal cord, and obliterates the subarachnoid space.
Surgical Treatment
The role of surgical decompression in the management of patients with MESCC has evolved over the years. Historically, radiation alone was the standard treatment for MESCC, largely due to an early study comparing the efficacy of laminectomy followed by radiotherapy with that of radiotherapy alone; no difference in outcome or survival was reported. Surgery at that time was a laminectomy that usually did not address the primary site of compression. Laminectomy decompressed the spinal canal and spinal cord but had only been proven to be effective if compression was posterior. As mentioned earlier, MESCC more commonly involves the anterior elements of the spinal column, such as the vertebral body. In the setting of anterior spinal compression, a laminectomy is insufficient to achieve decompression; furthermore, it may lead to loss of spinal stability if the posterior column is disrupted, resulting in neurologic deterioration after surgery. Therefore, this procedure should be reserved for the removal of posterior lesions.
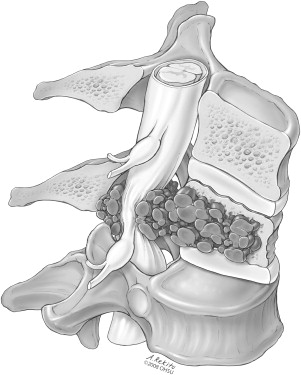
In the 1980s, with the advancement of surgical techniques and spinal instrumentation, it became possible to decompress the spinal cord circumferentially, and reconstruct and immediately stabilize the spine. This procedure can be done by combining an anterior approach, for example, thoracotomy, with a posterior approach, for example, laminectomy and fixation. For the thoracic spine, the most common location of MESCC, a single posterolateral approach can be used. This procedure involves removing anterior compressive lesions, reconstructing the anterior and middle columns of the spine, and restoring the stability of the posterior columns using segmental fixation with pedicle screws and rods ( Figs. 3–6 ). A sagittal MR image showing epidural compression of the thoracic spinal cord in a 50-year-old patient with metastatic melanoma and postoperative radiographs of the same patient showing spinal hardware after decompression and stabilization are presented in Fig. 7 . The advantage of surgical treatment over radiotherapy alone has been suggested in several uncontrolled surgical series. In a meta-analysis, Klimo and colleagues reviewed data from 24 surgical articles (999 patients) and 4 radiation articles (543 patients), and reported that surgery followed by radiation leads to higher overall ambulatory success rates than radiation alone (85% vs 64%, P <.001).