Oncoplastic surgery combines the principles of surgical oncology with those of plastic and reconstructive surgery. The intent is to use established techniques from each field in order to provide adequate tumor resection without compromise while optimizing aesthetic outcomes. This patient-centered approach requires a multidisciplinary preoperative evaluation in order to devise a comprehensive surgical plan and coordinate adjuvant treatment as needed. This article provides a historical perspective as well as insight into various creative techniques for breast cancer surgery.
Historical perspective
History has proved that in most cases, the treatment of breast cancer requires surgical intervention. Since Halsted’s original work in the late 1880s, the surgical management of breast cancer has instilled fear in women throughout the world, and breast surgery has been considered unpleasant but a necessary evil. Although the radical mastectomy accomplished local control, the advanced stage of disease often led to poor survivability; thus, surgical change was not possible until the era of screening mammography and the subsequent shift to the detection of earlier, often nonpalpable, tumors. Fortunately, since that time, significant progress has been made in the surgical management of breast cancer.
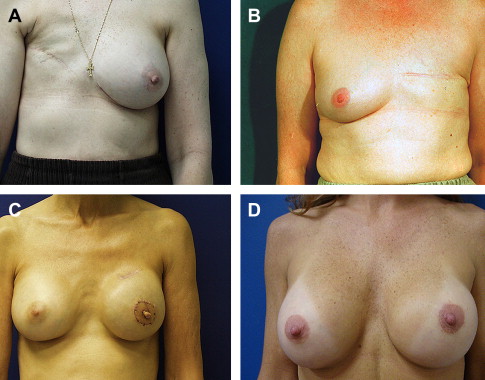
Much of this work began in the mid to late 1970s, and after decades of diligent scientific research, surgeons were able to show that less-extensive tissue resection was possible without endangering a woman’s life. The two most widely recognized clinical trials supporting this hypothesis are the Milan trials and the National Surgical Adjuvant Breast and Bowel Project. After more than 20 years of follow-up for each of these studies, clinicians have learned that various portions of the breast and surrounding structures can be preserved without having an impact on survival in a negative manner. During the course of these studies, however, it also became evident that surgery alone was not sufficient, and adjuvant treatment was necessary in order to achieve success with breast conservation surgery. Fig. 1 illustrates the dramatic differences that result from various surgical approaches for resection of primary breast tumors, ranging from radical mastectomy to lumpectomy. Combining the process of early tumor detection with less-extensive tissue resection and adjuvant therapies allowed for the first major changes in breast cancer surgery to occur. In the years that followed, these same advances contributed to the genesis of the field of oncoplastic, surgery, allowing for more and more creative, yet safe, surgical solutions ( Fig. 2 ).
The idea of combining knowledge from various subspecialties to create a comprehensive, individualized treatment plan was the modest beginning of the multidisciplinary patient-centered model. When considered separately, the advancements over the past several decades in each field, such as radiology, surgery, medical oncology, radiation therapy, and other fields, are impressive. When taken together collectively, however, the progression within each field allowed for clinical changes that are nothing less than extraordinary.
Given the widespread implementation of less-aggressive surgical resections (such as lumpectomy and sentinel lymph node biopsy), the interaction between surgeon, radiation oncologist, radiologist, pathologist, and oncologist has become essential to achieving a good outcome. First and foremost, the objective is to design a surgical plan that does not compromise tumor resection or place patients at undo risk of local recurrence that might result in the need for multiple surgeries. The determination for how much tissue must be removed (from an oncologic perspective) cannot be separated from a thorough and complete preoperative assessment of both breasts, including consideration of breast size and shape and patient desires. In this regard, the basic principles of aesthetic and reconstructive surgery must be understood by the surgeon performing the extirpative procedure because placement of incisions influences later options for reconstruction. Once full consideration is given to the surgical options and possible need for postoperative adjuvant therapy, an extensive discussion with patients helps define the most appropriate surgical plan.
Although studies show that local recurrence may not ultimately have an impact on overall survival rates, mortality is not the ultimate endpoint most women are trying to beat. Most women who have faced the reality of a diagnosis of breast cancer find it challenging to go through the experience, and most of them prefer not to endure the experience again. Thus, although the option of breast conservation brings with it the alluring possibility of avoiding bodily disfigurement (discussed previously), local resection alone is not as effective as mastectomy in reducing the risk of local recurrence. Thus, even in cases of early-stage breast cancer, radiation therapy and often chemotherapy are necessary when breast conservation is chosen instead of mastectomy. Given the widespread and long-standing aversion to mastectomy, however, breast conservation quickly became adopted by surgeons and women alike, and the addition of adjuvant therapies has been accepted when necessary. The reality and fear of local recurrence, however, remains a significant concern for many women, and many of these women opt for mastectomy instead of lumpectomy. Oncoplastic surgery can offer dramatic surgical improvements in this group of women, because often methods of skin sparing, and sometimes even nipple-areolar sparing, can be offered in a safe and effective manner (see Fig. 2 ).
With the adoption of breast conservation, physicians soon found clinical follow-up of these patients challenging because lumpectomy and radiation can result in significant scarring of the breast. This resulted in the unfortunate dilemma of making clinical or mammographic examination of the breast difficult and, in some cases, almost impossible. In addition, the aesthetic outcomes after breast conservation vary widely, and the results are often unpredictable after postoperative radiation therapy. When poor outcomes occur ( Fig. 3 ), surgical intervention with salvage mastectomy is often required to alleviate painful retraction from scarring, and the options for various methods of reconstruction may be limited given the commonly seen damage to the skin and underlying tissues secondary to postlumpectomy radiation.
Definition of oncoplastic surgery
The issues (discussed previously) helped spark the notion for a surgical subspecialty focused on breast surgery. Ultimately, in 2000 this led to the establishment of breast fellowship training programs, and in all likelihood, this subspecialty training will soon include training in oncoplastic surgery. The term, oncoplastic surgery , is fitting and was coined by Dr Werner Audretsch in an attempt to described the blending of surgical techniques from the fields of surgical oncology and plastic and reconstructive surgery. The premise is that whenever surgery is to be performed on the breast, consideration for cancer and aesthetics must be included. A handful of surgeons scattered over many countries began practicing in this manner in the early 1990s; however, only in the past decade has this approach gained widespread acceptance and enthusiasm in the United States. No doubt, this slow process of adoption was necessary in order to ensure that new techniques would not jeopardize patient safety. It is well recognized that oncoplastic surgery can improve surgical outcomes in a safe and effective manner as long as patient selection is appropriate. It is for this reason that multidisciplinary approach to the preoperative work-up is key to the practice of oncoplastic surgery.
Oncoplastic surgery does not refer to any given procedure; rather, it describes a surgical mindset in the approach of a patient facing various types of breast surgery. For example, a woman who presents for breast reduction surgery (commonly considered an aesthetic procedure) should be questioned about her risk for breast cancer and should undergo a preoperative work-up, including appropriate breast examination and imaging. This is done as a preoperative baseline and as a way to detect any potentially occult lesions within the breast. Any abnormalities are worked up prior to surgery, which may include mammography, ultrasound, MRI, and even minimally invasive biopsy if necessary.
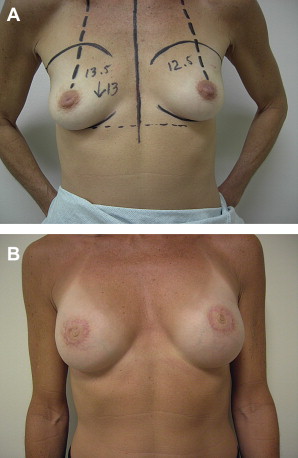
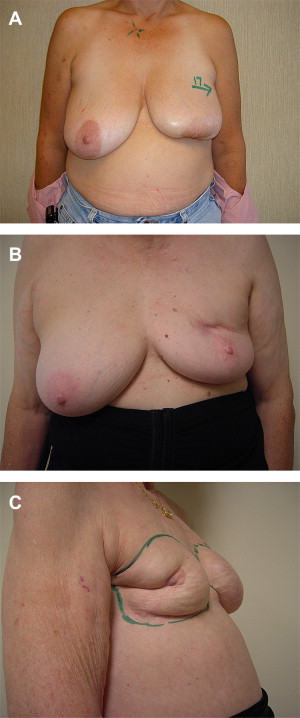
Similarly, a patient presenting with a diagnosis of breast cancer in the setting of large pendulous breasts may be an ideal candidate for a large tumor resection performed using standard techniques for breast reduction. Both of these examples illustrate how the oncoplastic approach can be applied to various clinical situations. Furthermore, the utility of breast reduction as a method for resection of breast cancer offers broad applications in oncoplastic surgery ( Fig. 4 ).
Definition of oncoplastic surgery
The issues (discussed previously) helped spark the notion for a surgical subspecialty focused on breast surgery. Ultimately, in 2000 this led to the establishment of breast fellowship training programs, and in all likelihood, this subspecialty training will soon include training in oncoplastic surgery. The term, oncoplastic surgery , is fitting and was coined by Dr Werner Audretsch in an attempt to described the blending of surgical techniques from the fields of surgical oncology and plastic and reconstructive surgery. The premise is that whenever surgery is to be performed on the breast, consideration for cancer and aesthetics must be included. A handful of surgeons scattered over many countries began practicing in this manner in the early 1990s; however, only in the past decade has this approach gained widespread acceptance and enthusiasm in the United States. No doubt, this slow process of adoption was necessary in order to ensure that new techniques would not jeopardize patient safety. It is well recognized that oncoplastic surgery can improve surgical outcomes in a safe and effective manner as long as patient selection is appropriate. It is for this reason that multidisciplinary approach to the preoperative work-up is key to the practice of oncoplastic surgery.
Oncoplastic surgery does not refer to any given procedure; rather, it describes a surgical mindset in the approach of a patient facing various types of breast surgery. For example, a woman who presents for breast reduction surgery (commonly considered an aesthetic procedure) should be questioned about her risk for breast cancer and should undergo a preoperative work-up, including appropriate breast examination and imaging. This is done as a preoperative baseline and as a way to detect any potentially occult lesions within the breast. Any abnormalities are worked up prior to surgery, which may include mammography, ultrasound, MRI, and even minimally invasive biopsy if necessary.
Similarly, a patient presenting with a diagnosis of breast cancer in the setting of large pendulous breasts may be an ideal candidate for a large tumor resection performed using standard techniques for breast reduction. Both of these examples illustrate how the oncoplastic approach can be applied to various clinical situations. Furthermore, the utility of breast reduction as a method for resection of breast cancer offers broad applications in oncoplastic surgery ( Fig. 4 ).