Surgical treatment for breast cancer has evolved from the original Halsted radical mastectomy to the segmental mastectomy, which was shown to be effective breast cancer therapy through trials as early as 1985. Since that time, breast-conservation therapy (BCT) via segmental mastectomy or lumpectomy and postoperative radiation therapy have become the treatment of choice in early-stage breast cancer, including stage I, IIA, or IIB.1 By current standards, almost three-quarters of breast cancers now qualify for BCT.2,3
Along with advancements in BCT, the melding of oncologic and reconstructive procedures has produced what is known as oncoplastic surgery and tumor-specific immediate reconstruction (TSIR) of the breast.4 TSIR, defined as reconstruction to restore symmetry after partial mastectomy or lumpectomy, has been carried out in various forms for over two decades. Reduction mammoplasty also provides opportunity for quadrantectomy, which may serve to improve local resection and decrease local recurrence rates.5 The specific combination of breast reduction with lumpectomy or partial mastectomy in the macromastic patient has been shown in several studies to be both aesthetically beneficial and oncologically sound.6 Breast reduction as an oncoplastic approach may provide a better alternative surgical option for women with macromastia with optimal cancer treatment and reconstructive outcomes.
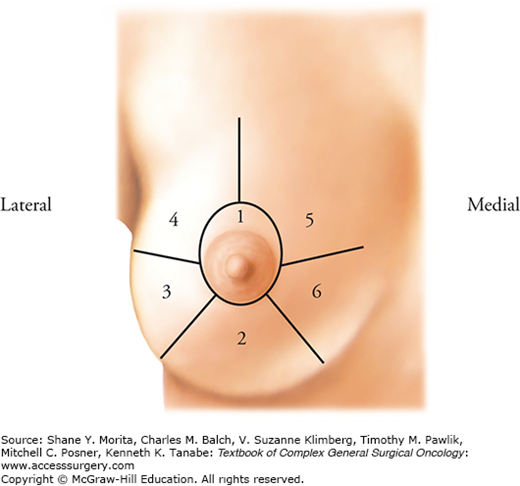
Reduction mammoplasty techniques rely on resection of breast tissue surrounding a vascularized pedicle. This pedicle can be based in various locations depending on the regions of breast tissue undergoing resection. Oncoplastic immediate reconstruction using mammoplasty techniques begins by preoperative quadrant localization of the tumor and estimation of the resection size required to obtain complete tumor excision compared to the total breast volume. Figure 152-1 provides a classification system for different tumor locations. Once the location and size of the resection have been estimated, the surgeon can then proceed to identify an appropriate pedicle location and pattern of skin incision.
Knowledge of breast blood supply is perhaps the most relevant anatomy with respect to the reduction mammoplasty technique. Blood supply to the breast is primarily via perforators from the internal mammary and anterolateral intercostal and anteromedial intercostal arteries. The breast skin maintains viability through the subdermal plexus and the above noted perforators. Interruption of either the subdermal plexus or the primary perforators can lead to breast skin necrosis, namely in the setting of lengthy skin flaps. Conversely, the nipple-areolar complex (NAC) is supplied by a robust subdermal plexus allowing for NAC viability based solely on an underlying vascularized pedicle of breast tissue. Sensation to the NAC is via branches of the third through fifth anterolateral and anteromedial intercostal nerves with the greatest contribution from the fourth intercostal nerve. The reduction mammoplasty techniques often sacrifice one of the above noted sources of innervation. Robust collateral innervation allows for preservation of sensation to the NAC.
Prior to oncoplastic reconstruction by the reduction mammoplasty technique, patients must be diagnosed with early stage I, IIA, or IIB breast cancer to qualify for BCT. Planned excision of greater than 20% of the breast volume during partial mastectomy is likely to result in poor aesthetic outcomes that may be improved with reconstruction via mammoplasty.7 It is the authors’ recommendation to select patients who would be satisfied with a reduction in volume of 250 grams or more from each breast to allow for adequate resection while providing the best final aesthetic outcome following reduction mammoplasty (Fig. 152-2).
Breast-conservation therapy does present several postoperative challenges including contour irregularities and breast asymmetry, which can be amplified in the macromastic patient. These challenges are often managed via TSIR most notably through reduction mammoplasty in large breasts.4 Dose heterogeneity can also be seen during postoperative radiation therapy in the macromastic patient and can be improved following immediate reduction mammoplasty.8,9
Adequate oncologic resection is paramount to the success of immediate reconstruction using reduction mammoplasty techniques as these techniques result in rearrangement of the breast architecture eliminating the possibility for re-resection of tumor margins. Inadequate or questionable margins are considered an absolute contraindication to immediate reconstruction by reduction mammoplasty. A history of previous breast radiation, pregnancy, collagen vascular disease (scleroderma and lupus), indeterminate calcifications, and multifocal disease are also considered contraindications to BCT with reconstruction.9
Assessment of the patient includes appropriate staging to ensure the viability of BCT prior to discussion of reconstructive options. Once candidacy for BCT has been confirmed, the risks and benefits of reconstruction must be addressed with the patient. Previous mammoplasty, BMI >30, current smoker, and large resection volumes (>1 kg) are all known to increase the risk of postoperative complications in reduction mammoplasty and should be considered preoperatively due to the potential for delays in wound healing and subsequent delays in delivery of postoperative radiation therapy.4,9–11 Finally, patients planning to undergo reconstruction via reduction mammoplasty must be psychologically prepared to accept the scar burden associated with these procedures as well as the inherent risk of subsequent mastectomy in the setting of positive or inadequate margins when8 immediate reconstruction is utilized.12
Once preoperative assessments have been completed, the surgical oncologist and reconstructive surgeon should develop a joint operative plan. Tumor location can be identified using the classification system shown in Figure 152-1. Anticipated defect size can then be discussed and an appropriate pedicle location selected using Table 152-1. Although intraoperative findings may dictate changes to the initial operative plan, preoperative identification of the vascular pedicle can minimize the risk of inadvertent pedicle compromise.
Most Commonly Selected Reduction Mammoplasty Pedicle and Skin Incision Patterns for Breast Reconstruction Categorized by Tumor Location
| Tumor Location | Pedicle Options | Skin Incision Options |
|---|---|---|
| 1 | Inferior | Wise |
| 2 | Superior-medial | Wise/Vertical |
| 3 | Superior-medial | Wise/Vertical |
| 4 | Inferior/Superior-medial | Wise |
| 5 | Inferior | Wise |
| 6 | Inferior | Wise |
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree