Problems
Prevalence (%)
ECOG PS ≥2
~20
ADL dependence
~20
IADL dependence
50–60
Comorbidity
>90
Severe comorbidity
30–40
Depression
20–40
Cognitive impairment
25–35
At risk of malnutrition/malnourished
30–50
Comorbidity is a major influencer of remaining life expectancy (which is different from life expectancy at birth). This can vary by up to 10 years for older patients of the same age [4]. In addition to survival, comorbidity impacts relapse-free survival and risk of cancer [5]. The impact of comorbidity in general on toxicity from chemotherapy is less clear independently from functional status, but the associated polypharmacy does increase toxicities. As in younger patients, specific diseases can interfere with the use of specific chemotherapy drugs [6–8].
Another principle is the age-related decrease in functional reserve. Whereas baseline physical functioning changes little with age, the ability of patient and body systems to handle stress decreases. This plays an important role in treatment planning and management as we will discuss below. Older patients also frequently are vulnerable in their social support. This might vary considerably with culture and location, but with urbanization and the rise of the nuclear family, this can be a critical issue for city dwellers or displaced persons. Given this global picture, optimal treatment of older cancer patients requires a multidisciplinary approach.
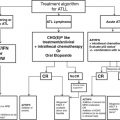
3 Geriatric Screening and Assessment
A complete comprehensive geriatric assessment (CGA) can take hours to days. Furthermore, geriatricians are in short supply, in both developed and emerging countries. Therefore, geriatric oncology researchers have developed a two-step approach to identify patients needing a geriatric work-up. Patients are initially screened with a short instrument for geriatric problems. If they screen positive, they are referred to a multidisciplinary team or geriatrician for further evaluation (Fig. 1). One should note the importance of doing an early geriatric screening. This allows using the 2–4 weeks usually needed for an oncology work-up for a parallel geriatric work-up, if necessary. This two-step approach identifies roughly half of the patients as having geriatric issues. When cancer patients undergo a geriatric evaluation, this modifies the cancer management in ¼ to ½ of cases [9]. Several screening tools are available and were recently reviewed in detail by the International Society of Geriatric Oncology (SIOG) CGA task force [10]. The article also contains a copy of the instruments themselves. From a practical point of view, we suggest reviewing a few of the tested tools and choosing the one best adapted to your individual clinical setting. For example, if you want many clinics to test all older patients for referral to a multidisciplinary clinic, then a short, patient-filled tool, such as the G8, is likely best. On the other hand, if you have a multidisciplinary clinic where team members can assess the patients at first visit, a slightly more extensive tool such as the SAOP2 can help you identify more precisely which team members to involve. Most screenings can be patient answered or included in the initial nursing assessment.
Fig. 1
General approach to treatment planning in an older cancer patient
3.1 Adaptation to a Sparse Resource Setting
A tropical oncologist might find himself/herself without an available consulting geriatrician or multidisciplinary team at hand. Although specific data are lacking, the advantages of running a geriatric screening are multiple. Firstly, this undeniably detects problems that otherwise would have been missed. Secondly, it identifies patients who will need a closer follow-up and coordination of care by at least the oncology team and the primary care physician or even a primary nurse practitioner in remote areas. We will detail some of these management considerations below. There is also an abundant general geriatric literature about nursing interventions that do not need an available physician. Sending a member of the oncology team for a short training in geriatric matters or an online course might prove very helpful.
4 Management Considerations
4.1 Decision Help Tools
An overall approach to treatment selection can use a three-tier model: healthy, vulnerable, and frail patients. Some tools have been developed that may assist in decision making. Several are available online (Table 2) and cover geriatric assessment, chemotherapy risk assessment, or life expectancy estimates. Standard oncology tools, such as Adjuvant! Online, can be suggestive, but should be used with caution, as their data estimates can be skewed in the elderly [11]. In addition, published predictive assessments are available, for example, for the risk of postsurgical complications: PACE/PREOP, Kristjansson [12, 13]. Some links provided in Table 2 are found very useful by the authors but in no way pretend to be an exhaustive list. Such lists evolve rapidly. With advancing age and comorbidity, patients may use increasingly diverse criteria to judge which treatment choice is “worth it,” and subjective estimates by both patient and physician become increasingly imprecise as case complexity increases. Therefore, one of the main goals of these decision helps is to provide accurate estimates of the benefits and risks of cancer and its treatment alternatives for discussion with the patient and other stakeholders.
Table 2
Useful links to online resources (blank lines added for you to insert your own favorites)
Name | Type | Link |
|---|---|---|
CARG score | Chemotoxicity risk prediction | |
CRASH score | Chemotoxicity risk prediction (the page also contains a low neutropenia risk calculator, CIRS-G calculator, and SAOP2 questionnaires in several languages) | |
ePROGNOSIS | General life expectancy | |
NCCN older adult oncology | Consensus guidelines | |
POGOe | Collection of free geriatric resources | |
SIOG | Geriatric assessment and cancer treatment guidelines for older patients |
4.2 Screening for Tropical Conditions
In tropical countries, parasitoses such as helminthiasis, kala azar, malaria, and filariasis are prevalent and should be treated prior to chemotherapy initiation. Vaccinations against viral diseases such hepatitis B and human papillomavirus have become available. Large vaccination campaigns such as those conducted against hepatitis B in Thailand appear to lead to a decrease in hepatocellular carcinoma. Data are sparse about the antitumoral effectiveness of vaccines in the elderly. On the other hand, the prevalence of chronic hepatitis B and C is a real issue. Lamivudine prophylaxis decreases the risk of reactivation of hepatitis B during chemotherapy [14]. At the present time, no prophylaxis is recommended for hepatitis C patients.
4.3 Surgery
Most surgical series highlight the fact that elective surgery in older patients has outcomes similar to those of younger patients with similar ASA scores, with only slightly higher morbidity/mortality [15]. A geriatric evaluation needs to be conducted to identify patients at risk of complications beyond a simple ASA score [12, 13]. Preoperative screening for risk of delirium is important, as it significantly increases the risk of functional dependence and mortality and prolongs hospitalization. Furthermore, it can be prevented or reverted with mostly simple, non-medicamentous means if detected early [16]. On the other hand, because of the age-associated decrease in functional reserve, emergency surgery has a higher risk of morbidity and mortality in older patients than in younger ones [17, 18]. Therefore, every effort should be made to preempt emergency situations: public education, well-prepared elective interventions, and stabilization of an acute patient prior to surgery (e.g., endorectal stent). Discharge planning is also important. Older patients have higher transitional care needs, and home interventions can improve survival [19, 20].
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree