##
Any adrenal mass needs evaluation for adrenal hormonal excess and malignancy. , Imaging characteristics can be helpful to exclude malignancy. Workup for adrenal hormone excess includes assessment for cortisol, aldosterone, and catecholamine excess. Here, we present a case of an incidentally discovered adrenal mass, which was determined to be benign and nonfunctioning and where further imaging and biochemical monitoring were not required.
Case Report
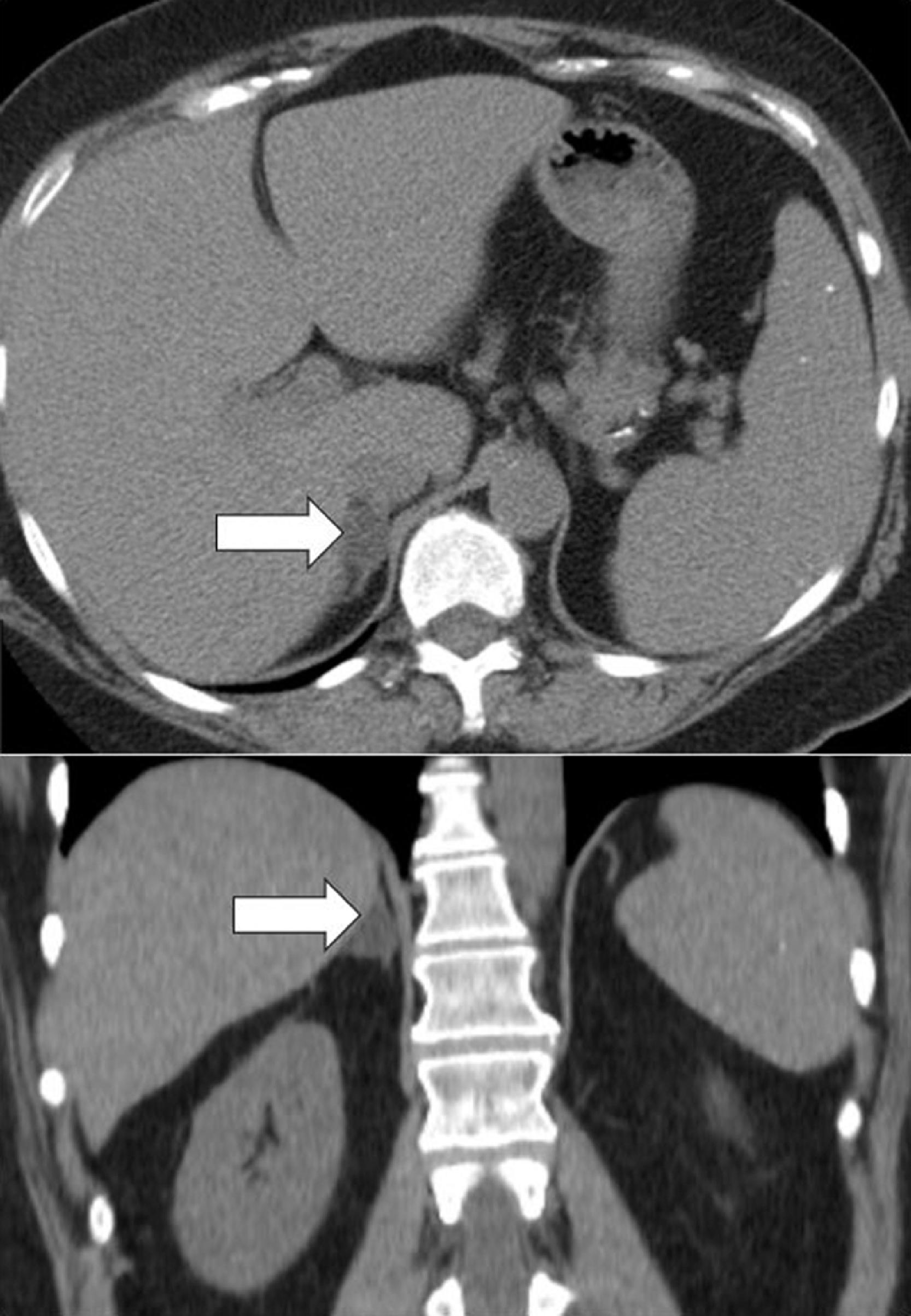
The patient was a 59-year-old woman who presented for evaluation of an incidentally discovered right adrenal mass on an abdominal computed tomography (CT) scan performed for investigation of left-sided abdominal pain. The right adrenal mass measured 1.6 × 2.0 × 1.2 cm with an unenhanced CT attenuation of 5.5 Hounsfield units (HU) (see Fig. 4.1 ). She had partial workup at home and was advised that she did not have a pheochromocytoma. She was referred to our institution for further evaluation.
She had a 6-year history of hypertension and type 2 diabetes mellitus. She was also diagnosed with dyslipidemia 4 years prior. Her bone mineral density performed several years prior was normal. Her medications included lisinopril, hydrochlorothiazide, glipizide, and insulin. She had no overt signs of adrenal dysfunction or past history of malignancy. She had no change in body weight. On physical examination her body mass index was 33.67 kg/m 2 , blood pressure 132/82 mmHg, and heart rate 94 beats per minute. She had no stigmata of Cushing syndrome.
INVESTIGATIONS
The baseline laboratory test results are shown in Table 4.1 . The laboratory tests were normal.
| Biochemical Test | Result | Reference Range |
| 4 pm serum cortisol, mcg/dL1 mg DST serum cortisol, mcg/dLACTH, pg/mLAldosterone, ng/dLPlasma renin activity, ng/mL/hrDHEA-S, mcg/dLPlasma metanephrine, nmol/LPlasma normetanephrine, nmol/L | 2.5<1408.515.3950.10.56 | 1.4–7<1.810–60≤21≤0.6–316–195<0.5<0.9 |
OUTCOME AND FOLLOW-UP
The patient was counseled that the adrenal mass was a benign nonfunctioning adrenal adenoma. This was concluded based on imaging phenotype of the adrenal mass with low unenhanced CT attenuation. The patient was advised that no further endocrine follow-up was necessary.
Discussion
CT attenuation measurement on unenhanced CT can help clarify the etiology of an adrenal mass. Adrenocortical adenomas can be lipid rich (HU <10) in around 60% of cases, demonstrate indeterminate unenhanced CT attenuation of 10–20 HU in around 20%–25% of cases, and be lipid poor (>20 HU) in 15%–20% of cases. , Adrenocortical carcinomas, other malignant adrenal tumors (e.g., sarcomas, metastases), and pheochromocytomas usually demonstrate unenhanced CT attenuation >20–30 HU and infrequently in the indeterminate zone of 10–20 HU (around 2%–5%). Thus, a homogeneous adrenal mass with an unenhanced CT attenuation of <10 HU excludes malignant adrenal tumors and pheochromocytomas, and imaging follow-up in these cases is not needed. In addition, workup for pheochromocytoma is not needed in adrenal tumors demonstrating unenhanced CT attenuation with <10 HU. , , As reported in a systematic review of 2023 patients with adrenal adenomas, 2.5% of adenomas may demonstrate growth >1 cm depending on when in relation to its natural history the tumor is first discovered. However, the risk of malignant transformation was 0%. In patients with either nonfunctioning adrenal adenomas (serum cortisol concentration after the 1-mg dexamethasone suppression test <1.8 mcg/dL) or those with mild autonomous cortisol secretion (MACS) (serum cortisol concentration after the 1-mg dexamethasone suppression test >1.8 mcg/dL), overt hormone excess (primary aldosteronism, catecholamine excess, or Cushing syndrome) developed in approximately 0.2% (6 of 2745 patients). The proportion of patients with nonfunctioning adrenal adenomas who developed new MACS during a mean follow-up of 20.3 months was 4.3% (149 of 2083). Repeating dexamethasone suppression tests in patients with bilateral nodular disease or in those with new symptoms potentially related to MACS could be considered.