Summary of Key Points
- •
Treatment of lung cancer is rapidly evolving. Large cell carcinomas as a group have therapeutically relevant driver mutations in nearly 40% of cases.
- •
Despite the recent failures of some agents, in 2015 the US Food and Drug Administration issued seven approvals of agents for the treatment of lung cancer.
- •
Many additional promising agents that target several aberrant signaling pathways are under development.
- •
A large proportion of genomic alterations are not considered directly druggable targets, such as mutant p53 or amplified SOX2; this obstacle may be surmounted by identifying synthetically lethal changes amenable to drug therapy.
- •
Targeted therapy requires simultaneous development of the targeted agent along with biomarker assay platforms for patient selection to optimize therapeutic benefit.
- •
To avoid misinterpretation of clinical trial data, thorough understanding of drug activity and characterization of pharmacologic activity, particularly of small-molecule inhibitors, is necessary, particularly when an anticipated clinical benefit is not found.
Major advances in the therapy of cancer have occurred since the beginning of the new millennium. These advances were spurred by increased knowledge of the biologic hallmarks of cancer coupled with breakthroughs in genomic and pharmaceutical technologies. In the field of lung cancer, researchers discovered the oncogenic role of so-called druggable proteins arising from somatic mutations in the epidermal growth factor receptor ( EGFR ) gene and chromosomal rearrangements in the anaplastic lymphoma kinase ( ALK ) gene. These findings led to therapies resulting in substantially higher response rates and survival in patients with lung cancer being treated with EGFR and ALK inhibitors, respectively, compared with conventional chemotherapy. Recognizing the integral role played by the tumor microenvironment in the initiation and maintenance of the malignant phenotype has also resulted in the development of antiangiogenesis agents with clinical relevance in various malignancies, such as the use of the monoclonal antibody bevacizumab in the nonsquamous subtype of nonsmall cell lung cancer (NSCLC). Modulation of immune checkpoints is another highly promising approach. In this chapter, we review promising therapeutic drug targets for the treatment of NSCLC as of 2016.
Although the relevance of each target and its role in each signaling pathway is presented in a linear fashion to facilitate discussion, individual targets do not function in isolation because cells possess a complex architecture of signaling networks that are highly interconnected. Moreover, negative feedback loops and concurrent activation of multiple substrates involved in a number of important pathways can lead to paradoxical effects depending on the cellular context. Thus, the presence of a drug inhibitor can result in pathway activation that leads to cell survival or proliferation rather than cell death, resulting in ineffective therapies. This is a challenge in the therapy of malignancies such as lung cancer, which tend to harbor multiple molecular aberrations. Additionally, targeted therapies may also affect signaling networks within nonmalignant cells and modulate antitumor immunity or the tumor microenvironment.
Key Signal Transduction Pathways
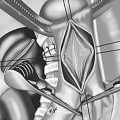
The two major signaling cascades that are triggered upon activation of growth factor receptors are the RAS/RAF/MAPK and the PI3K/AKT/mTOR pathways. Multiple relevant targets for drug therapy in NSCLC can be illustrated as they transduce signals through these two interconnected pathways ( Fig. 48.1 ).

The RAS/RAF/MAPK pathway plays a major role in the signaling cascades of various growth factor receptors, such as EGFR, human epidermal growth factor receptor type 2 (HER2), fibroblast growth factor receptor (FGFR), and others. Upon activation of receptor kinase signaling, recruitment of adaptor proteins (e.g., Grb2, Shc, and others) triggers key downstream steps involving RAS activation. After this event, the serine/threonine kinase RAF (a member of the MAPK kinase or MAPKKK group of protein kinases), represented by the members ARAF, BRAF, and CRAF, phosphorylates two distinct serine residues on the MAPKs (also known as MEK) MEK1 and MEK2. MEK1/2 subsequently phosphorylates both serine/threonine and tyrosine residues in the final p44 and p42 MAPK (also known as ERK1/2) in the cascade, which then phosphorylates downstream substrates, resulting in proliferation and survival.
Similarly, lipid phosphorylation via phosphoinositide 3-kinase (PI3K) signaling regulates various cellular functions such as proliferation, survival, metabolism, and metastasis. This pathway is normally regulated by receptor tyrosine kinases (RTKs), particularly signals generated by insulin and insulin-like growth factor 1 (IGF-1) receptors (IGF-1Rs). The PI3K pathway is also frequently involved in the development and maintenance of the malignant phenotype arising from oncogenically driven RTK activation of the pathway. The class I PI3Ks are primarily involved in the generation of phospholipid messengers in response to RTK activation. Termination of PI3K signaling in turn is mediated by phosphatases such as the tumor suppressor phosphatase and tensin homolog (PTEN) on chromosome 10.
Phospholipid messengers generated upon PI3K activation bind to phosphoinositide-dependent kinase 1 (PDK1) and, downstream to it, protein kinase B (AKT) and other effector proteins through specific pleckstrin homology or other lipid-binding domains. PDK1 is the principal kinase responsible for phosphorylation and activation of the serine/threonine kinase AKT. AKT itself is also phosphorylated by downstream substrates, an example of nonlinear interactions that exist in signaling pathways. Activated AKT phosphorylates various substrates that mediate diverse functions, such as degradation of the Forkhead (FOXO) transcription factors and inhibition of BAD and BAX, resulting in reduced apoptosis and cell survival. AKT also activates mammalian target of rapamycin (mTOR) by direct phosphorylation as well as by phosphorylating the tumor suppressor tuberin (also known as TSC2), thus inhibiting the repressor function of the tuberin–hamartin (also known as TSC1) complex on mTOR. mTOR kinase, a highly conserved serine/threonine kinase, subsequently regulates cellular metabolism and protein synthesis through downstream effectors such as p70S6K and 4EBP1. MEK/ERK signaling also activates mTOR by inactivating TSC2 upon phosphorylation by ERK1/2, one of the several links between the RAS/RAF/MAPK and PI3K/AKT/mTOR pathways.
Therapeutic Targets
This chapter provides a review of the frequency of genomic alterations found in relevant selected targets for two major histologic subtypes of NSCLC, squamous cell carcinoma and adenocarcinoma ( Table 48.1 ). Large cell carcinomas as a group have therapeutically relevant driver mutations in nearly 40% of cases. The distribution of these mutations has been described and mirrors the classification of squamous and nonsquamous subtypes of NSCLC as defined by immunohistochemistry (IHC), and thus is not categorized separately. Many drugs are in clinical use or in development for each corresponding drug target.
| Frequency (%) | |||
|---|---|---|---|
| Genetic Abnormality | Gene Location | Squamous Cell Carcinoma | Adenocarcinoma |
| HER2 overexpression | 17q11.2–q12, 17q21 | 3–5 | 5–9 |
| ∗ HER2 amplification | 17q11.2–q12, 17q21 | ||
| EGFR-TKI naïve | <1 | 1–4 | |
| Acquired EGFR-TKI resistance | — b | 12–13 | |
| ∗ FGFR1 amplification | 8p12 | 22 | 1–3 |
| PIK3CA amplification | 3q26.3 | 33 | 6 |
| c-MET amplification | 7q31.1 | 3–21 | 3–21 |
| HER2 mutation | 17q11.2–q12, 17q21 | 1 | 2 |
| ∗ HER3 mutation | 12q13 | 1 | 1 |
| c-MET mutation | 7q31.1 | 1 | 2 |
| ∗ FGFR2 mutation | 10q26.13 | 3 | 1–2 |
| ∗ FGFR3 mutation | 4p16.3 | 3 | <1 |
| DDR2 mutation | 1q23.3 | 4 | 1 |
| KRAS mutation | 12p12.1 | 6 | 21 |
| ∗ NRAS mutation | 1p13.2 | — | <1 |
| ∗ BRAF mutation | 7q34 | <1–2 | 3–5 |
| ∗ MAP2K1 mutation | 15q21 | — | <1 |
| ∗ PIK3CA mutation | 3q26.3 | 3–9 | 2–3 |
| PTEN mutation | 10q23.3 | 10 | 2 |
| PTEN loss | 10q23.3 | 8–20 | 8–20 |
| AKT1 mutation | 14q32.32 | 1 | Very rare |
| LKB1 mutation | 19p13.3 | 5 | 23 |
| ∗ LKB1/KRAS dual mutations | 19p13.3/12p12.1 | — | 5–10 |
| ∗ PIK3CA/KRAS dual mutations | 3q26.3/12p12.1 | — | <1 |
| ∗ NRG1 fusion | 8p12 | — | <4c |
| ∗ ROS1 fusion | 6q22 | 0–1 | 1–3 |
| ∗ RET fusion | 10q11.2 | <1 | 1–2 |
| ∗ FGFR fusion | (FGFR1) 8p12 (FGFR2) 10q26.13 (FGFR3) 4p16.3 | <1–2 | <1 |
| ∗ BRAF fusion | 7q34 | — | 3 c |
a Table adapted with permission from the American Association for Cancer: Perez-Moreno P, et al. Squamous cell carcinoma of the lung: molecular subtypes and therapeutic opportunities. Clin Cancer Res . 2012;18(9):2443–2451. Genetic abnormalities with an asterisk (∗) pertain to data updated or not found in the original table.
b Denotes that no data have been published to date.
Receptor Tyrosine Kinases
Human Epidermal Growth Factor Receptor Type 2
HER2 (also known as ERBB2) belongs to the same family of HER RTKs as EGFR. In contrast to EGFR, HER2 does not interact with any ligand directly but serves as the preferred dimerization partner of EGFR and other ErbB family members, such as HER3 and HER4, to trigger autophosphorylation and downstream signaling through both the MAPK and PI3K pathways described earlier. HER2 gene amplification (defined as HER2/CEP17 ratio per cell of 2 or greater, and absolute HER2 signals in more than 4; or more than 15 copies in more than 10% of cells using fluorescence in situ hybridization [FISH] assay) is found in approximately 1% to 3% of lung cancers. HER2 exon 20 insertions are found in approximately 3% of adenocarcinomas. HER2 amplification is correlated with histologic subtype and tumor grade, such that high-level amplification appears to be concentrated in the subgroup of high-grade adenocarcinomas. Intratumor heterogeneity in the level of HER2 amplification also appears frequently. This latter feature may partly account for the negative results of clinical trials conducted a decade ago using trastuzumab in combination with chemotherapy for patients with NSCLC. In addition to patients with tumor heterogeneity, these studies included patients with potentially low-to-absent HER2 amplification (e.g., inclusion of patients with 2+ HER2 protein expression as determined by IHC).
Afatinib, an oral pan-HER inhibitor, has been used as monotherapy in genotypically selected solid tumors (lung cancers excluded) with either EGFR or HER2 amplification but showed limited activity, with an objective response rate of 5%. Lapatinib, an oral dual EGFR/HER2 inhibitor, demonstrated limited activity as monotherapy in a molecularly unselected population of NSCLC tumors. Of interest is that one of two patients with HER2 amplification (determined retrospectively) had a partial response, although this result was not confirmed. Dacomitinib is another oral pan-HER inhibitor with demonstrated in vitro activity in selected HER2 -amplified cell lines resistant to trastuzumab and lapatinib, which resulted in a 12% response rate in patients with HER2 exon 20 insertions, but no responses in patients with HER2 amplification.
HER2 amplification is also implicated in acquired resistance to therapy with EGFR tyrosine kinase inhibitors (TKIs) in laboratory models and in the clinical setting. HER2 amplification is found in 12% to 13% of cases of acquired resistance to EGFR-TKIs wherein it is mutually exclusive with the EGFR T790M mutation among tumors with acquired EGFR-TKI resistance. In contrast, no HER2 exon 20 mutations were identified in patients who developed resistance to the irreversible EGFR-TKI afatinib. HER2 amplification is also a putative mechanism of acquired resistance to ALK inhibitors in EML4–ALK-translocated lung cancer cells in vitro, although clinical studies have not confirmed this possibility to date.
In comparison, mutations in HER2 occur in 2% to 4% of NSCLC tumors, largely in high-grade and moderately to poorly differentiated adenocarcinomas. More than 95% of the mutations described to date are small insertions in exon 20, mostly represented by an in-frame insertion of 12 base pairs that causes duplication of the amino acids YVMA. Functional studies of this insertion mutation show that it confers greater transforming and antiapoptotic potential, in addition to its stronger catalytic activity, compared with wild-type HER2 . It can also trigger EGFR activation in the absence of cognate ligands and EGFR kinase activity. HER2 mutations appear to occur in greater proportions among women and never-smokers and are generally mutually exclusive with EGFR and Kirsten rat sarcoma ( KRAS ) mutations as well as HER2 amplification, with rare exceptions. An activating HER2 V659E mutation sensitive to lapatinib was described in a specimen of lung adenocarcinoma from a patient with Li-Fraumeni syndrome. It is anticipated that secondary HER2 mutations, such as L755S, T862A, and the gatekeeper T798M mutation, can arise as a mechanism of acquired drug resistance similar to what is seen in HER2 -amplified breast cancers after chronic therapy with lapatinib.
Afatinib has been reported to induce tumor response or disease stabilization when used as monotherapy in HER2 -mutant lung adenocarcinomas. Similarly, trastuzumab-based combinations have induced partial responses. Although lapatinib demonstrated preclinical activity against cells expressing the HER2 insertion mutation, tumor response has not been documented with monotherapy in the very limited number of patients reported on thus far. Clinical activity has been documented, however, when lapatinib is used in combination with either chemotherapy or trastuzumab-based regimens in patients with NSCLC who have either a HER2 exon 20 insertion or the HER2 V659E mutation. As per above, dacomitinib resulted in a 12% response rate in patients with HER2 exon 20 insertions. HER2 exon 20 mutations, especially HER2YVMA, appear to be a promising target in lung cancer but needs to be validated.
Human Epidermal Growth Factor Receptor Type 3
HER3 (also known as ERBB3) is another representative of the four-member group in the HER RTK family. HER3 is generally considered to have functionally weaker kinase activity compared with EGFR. Heterodimerization with other HER members, such as with HER2 upon binding of the ligand neuregulin, triggers autophosphorylation and recruitment of downstream signaling molecules. HER3 mutations have been reported in approximately 1% of lung adenocarcinomas and 1% of squamous cell lung cancers. Most of the HER3 mutations identified to date are clustered in the extracellular domain (ECD), although some are mapped to the kinase domain. The functional characteristics of most specific mutants described in NSCLC are yet to be verified; however, several HER3 mutations in either the ECD or kinase domain have been shown to promote oncogenesis in a ligand-independent manner, although this effect required the presence of kinase-active HER2. Recently, an activating HER3 V855A mutation that is homologous to EGFR L858R was identified in a patient with chemotherapy resistant NSCLC. This mutation was transforming in murine and human cell line studies in the presence of wild-type HER2 . Various small-molecule inhibitors and monoclonal antibodies against HER2 and HER3, as well as PI3K inhibitors, have demonstrated variable effectiveness depending on the specific HER3 mutation.
The recurrent fusion gene CD74-NRG1 found in mucinous lung adenocarcinomas of never-smokers appears to correlate with increased HER3 phosphorylation in tumor tissue. This chimeric transcript results in the expression of the EGF-like domain in tumor tissue that is otherwise negative for neuregulin. Functional characterization of this fusion protein in vitro showed activation of the PI3K-AKT pathway. Indeed, HER3 plays an integral role in activation of the PI3K survival pathway upon its heterodimerization with EGFR or HER2 in malignant cell lines. EGFR-TKI-sensitive NSCLC cancer cell lines rely on HER3 signaling to activate the PI3K/AKT pathway.
HER3 signaling is also implicated in acquired resistance to EGFR-TKIs. Persistent HER3-activated PI3K signaling is uncoupled from EGFR and is mediated instead through its interaction with MET, which is amplified in this setting. Another mechanism that can sustain HER3-activated PI3K signaling is disruption of negative feedback networks. ERK signaling leads to feedback phosphorylation of the conserved T669 residue within the juxtamembrane domain of EGFR, HER2, and HER4, and this prevents transphosphorylation of HER3 ( Fig. 48.1 ). The loss of this dominant negative feedback suppression of HER3 by intact MEK/ERK signaling is thought to account for the increased AKT phosphorylation found with MEK inhibitors in EGFR- and HER2-driven malignant tumors.
Blockade of HER3 signaling, through monoclonal antibody therapies or antisense oligonucleotides, improves the antitumor activity of EGFR and HER2 TKIs in preclinical models, including cell lines with acquired resistance to EGFR-TKIs. Another proposed approach for reducing HER3-mediated activation to enhance EGFR-TKI activity involves modulation of circulating neuregulin ligands via inhibition of ADAM17, a membrane-associated metalloprotease that cleaves and releases HER ligands from cells to enable receptor binding. Afatinib and dacomitinib are both oral irreversible pan-HER TKIs that have produced marked tumor regression in xenograft models that contained EGFR mutations, including the T790M mutation, which is associated with acquired resistance to EGFR-TKIs. However, subsequent modeling showed that cytotoxicity against T790M can be accomplished only at clinically unachievable concentrations, thus accounting for the limited efficacy seen for this patient subset in the clinic. Nonetheless, these agents can block HER2 heterodimerization with EGFR or HER3, thus explaining the potential to overcome acquired resistance mediated by HER3. In a randomized phase II study comparing dacomitinib and erlotinib, dacomitinib demonstrated significantly improved progression-free survival in KRAS wild-type NSCLC with or without EGFR mutation. A phase III study comparing first-line dacomitinib with gefitinib for patients who have NSCLC with EGFR-activating mutations was ongoing at the time of publication. Another phase III study comparing second- or third-line dacomitinib and erlotinib in patients with KRAS wild-type NSCLC has completed enrollment at the time of the publication of this chapter ( ClinicalTrials.gov identifier: NCT01360554 ). A phase III clinical trial recently demonstrated statistically significant but modest improvements in progression-free and overall survival with afatinib compared with erlotinib in patients receiving second-line therapy for squamous cell NSCLC; however, enthusiasm for these results has been muted by the advances seen with immunotherapy for this patient population. Various monoclonal antibodies against HER3 are being investigated in clinical trials, combining them with other inhibitors of the EGFR or HER2 pathway.
Hepatocyte Growth Factor Receptor
Binding of the ligand hepatocyte growth factor (HGF, also known as scatter factor), a paracrine factor secreted by stromal cells, to its cognate receptor MET facilitates receptor phosphorylation, leading to the activation of downstream signaling through the MAPK and PI3K pathways, which promote epithelial-to-mesenchymal transition (EMT), invasion, and metastasis. Ubiquitin-mediated receptor degradation is regulated at the Cbl E3-ligase RTK binding domain, similar to what has been described for EGFR and HER2. Mechanisms of aberrant activation of MET described in NSCLC include receptor overexpression (with or without HGF), c-MET gene amplification, or exon 14 skipping abnormalities. Levels of MET expression as high as 60% have been reported in various studies of NSCLC. Both the EGFR and c-MET genes are located on chromosome 7, and an increased copy number of the c-MET gene as determined by FISH is associated with an increased copy number of the EGFR gene and confers a worse prognosis. Coamplification of c-MET and EGFR is also described in up to 8.5% of NSCLCs not previously treated with EGFR-TKIs. Amplification of c-MET also occurs infrequently with an incidence of 3% to 7% among patients not treated with EGFR-TKIs, but this incidence increases to 10% to 22% among patients with acquired resistance to EGFR-TKIs. Exon 14 skipping mutations occur in about 3% of patients with NSCLC. Patients with sarcomatoid pulmonary carcinomas are enriched for MET exon 14 skipping mutations, and one study identified that 22% of patients with this relatively rare form of lung cancer have this mutation. MET can be transactivated through a variety of protein interactions and can heterodimerize with other RTKs, such as EGFR, HER2, HER3, and ret proto-oncogene (RET), in cells with c-MET amplification, representing an escape or bypass mechanism mediating resistance to inhibitors of these RTK-activated signaling pathways. In a preclinical model, MET activation through paracrine secretion of HGF also served as a mechanism for resistance to second-generation selective ALK inhibitors such as ceritinib (LDK378), but not to the MET/ALK inhibitor crizotinib.
Somatic intronic mutations of c-MET that lead to an alternatively spliced transcript, encoding a deletion of the exon-14 juxtamembrane domain spanning the amino acids 964 through 1010, result in loss of the Cbl binding site at Y1003. This skipping mutation in exon 14 yields a functional MET protein with decreased ubiquitination and consequently sustained activation of the MAPK pathway through altered receptor downregulation. This mutation variant appears to be mutually exclusive with mutations of other genes involved in the MAPK pathway (e.g., EGFR , RAS , and RAF ). Additional mutations have been described in both the ECD and juxtamembrane domains, some of which have transforming potential. No reports have indicated nonsynonymous mutations in the kinase domain to date. Of note is that most of these other mutations reported are in fact germline. The germline mutation N375S, which occurred at the highest frequency, appears to be associated with smoking and squamous histology. The MET -N375S mutation seems to confer resistance to the small-molecule MET kinase inhibitor SU11274.
Various approaches for inhibiting the MET pathway have been tested or are in clinical development. These strategies include anti-HGF and anti-MET monoclonal antibodies, or small-molecule MET kinase inhibitors. The MET/ALK/ROS1 inhibitor crizotinib was reported anecdotally to induce a rapid and durable response in a patient with de novo c-MET amplification without ALK rearrangement. Models of resistance to MET inhibitors predict the emergence of either secondary mutations or activation of EGFR signaling through increased expression of transforming growth factor-α. A randomized phase III study in previously treated patients with NSCLC of erlotinib with or without tivantinib, initially thought to be a selective nonadenosine triphosphate (non-ATP) competitive MET inhibitor, was halted because of an increased incidence of interstitial lung disease; regardless, there was no improvement in overall survival. Similarly, a separate phase III clinical trial conducted throughout Europe and the United States failed to show an overall survival benefit of erlotinib and tivantinib compared with erlotinib and placebo. Nonetheless, preclinical data generated from two different groups suggest that although tivantinib can mitigate HGF-dependent MET activation, this is not its major mechanism of action. Tivantinib (in contrast to crizotinib) did not inhibit MET autophosphorylation at doses that induced apoptosis. Instead, it exhibited cytotoxicity regardless of activation status of the MET pathway or the presence or absence of a functional MET kinase. In fact, growth inhibition and cytotoxicity reported with tivantinib may be mainly due to its effect on microtubule dynamics, which is not found with other MET inhibitors.
Onartuzumab (MetMAb), a monoclonal antibody that binds to the ECD of MET to prevent ligand binding, was evaluated in a randomized phase III study in combination with erlotinib as compared with placebo plus erlotinib in patients with NSCLC and MET-positive status as determined by IHC. The rationale for the study was based on promising results for progression-free survival (2.9 vs. 1.5 months; hazard ratio [HR], 0.53; p = 0.04) and overall survival (12.6 vs. 3.8 months; HR, 0.37; p = 0.002) noted in patients with MET-positive NSCLC who received the onartuzumab plus erlotinib combination compared with the placebo plus erlotinib treatment in the preceding randomized phase II study. In contrast, patients with MET-negative NSCLC who received the combination had worse progression-free survival (1.4 vs. 2.7 months; HR, 1.82; p = 0.05) and overall survival (8.1 vs. 15.3 months; HR, 1.78; p = 0.16) compared with patients who received placebo plus erlotinib. Unfortunately, the phase III clinical trial was stopped early due to futility as the experimental arm did not improve overall survival (OS), progression free survival (PFS), or overall response rate (ORR) compared with erlotinib alone.
Whereas targeting MET based on protein expression has had challenges, MET amplification and MET exon 14 skipping mutations are emerging as promising targets. The interim analysis of a small study demonstrated that 4 of 12 patients with intermediate (2.2–5) or high (>5) ratios of MET to CEP7 responded to crizotinib. An even more impressive response rate was observed in an interim analysis of a trial of the safety and efficacy of crizotinib for patients with MET exon 14 skipping mutations where 10 of 15 patients had confirmed or unconfirmed partial responses. One case report showed that a patient with a MET exon 14 skipping mutation who demonstrated a response to crizotonib acquired a mutation in the MET kinase domain, D1228N, at the time of progression. Responses have also been observed in patients with MET exon 14 skipping mutations treated with cabozantinib. Other MET inhibitors in development include AMG337 and capmatinib (INC280). These ongoing trials will help clarify which MET abnormalities are potentially targetable in NSCLC, but MET exon 14 skipping mutations and amplification seem to be better predictors of response than MET expression by IHC at this time.
Fibroblast Growth Factor Receptor
The fibroblast growth factor receptor (FGFR) signaling module plays an important role in various cellular processes, such as vascular and skeletal development during embryogenesis, as well as regulation of angiogenesis and wound healing in adults. The FGF family of ligands, with more than 20 members, is sequestered to the extracellular matrix by heparin sulfate proteoglycans. Five FGFRs exist, of which FGFR s 1–4 are highly conserved and contain the classic tyrosine kinase motifs in their split kinase domain. Moreover, FGFR s 1–3 are subject to alternate splicing, which results in variants with tissue-specific expression and varying ligand affinity. Dimerization of the ternary complex consisting of FGF, FGFR, and heparin sulfate proteoglycan activates downstream signaling, which ultimately leads to pathway activation of the RAS/MAPK and PI3K/AKT signaling cascades.
Various mechanisms of oncogenic FGFR signaling have been described in NSCLC. Focal amplification of FGFR1 is reportedly found in 22% of squamous-type NSCLCs. FGFR1 amplification appears to result in ligand-independent signaling and confers sensitivity to treatment using small molecule FGFR-TKIs. Somatic gain-of-function mutations in FGFR2 and FGFR3 , a subset of which have transforming ability, have also been described in up to 6% of squamous NSCLCs. These mutations are commonly coincident with mutations in TP53 and PIK3CA and are mostly sensitive to inhibition by FGFR-TKIs. Mutations in FGFR2 or FGFR3 can occur in either the kinase domain, causing constitutive activation, or in the ECD, which results in constitutive dimerization. Cell models (i.e., fibroblasts) expressing the ECD mutations and exposed to a low concentration of multikinase inhibitors with anti-FGFR activity exhibited enhanced growth. This growth-promoting phenomenon was not seen with higher drug concentrations or with the use of selective FGFR inhibitors.
Various chromosomal rearrangements involving FGFR1 – 3 result in fusion products that also exhibit ligand-independent oligomerization capability, activation of the MAPK pathway, and sensitivity to FGFR-TKIs. Several of these reported in NSCLC include BAG4–FGFR1, FGFR2–CIT, FGFR2–KIAA1967, and FGFR3–TACC3. The FGFR3–TACC3 fusion, found in approximately 2% of squamous cell NSCLCs and rarely in adenocarcinoma, is the most frequently reported to date. Other potential fusion partners that mediate oligomerization in other tumor types include BICC1, CCDC6, BAIAP2L1, CASP7, and OFD1.
Similar to other TKIs, an anticipated mechanism of acquired resistance to FGFR inhibitors is the emergence of secondary mutations, such as the V555M alteration in FGFR3 . Oncogenic switch or constitutive activation of other pathways leading to activation of the MAPK or PI3K pathway, such as through MET, may also underlie acquired or intrinsic resistance to FGFR inhibition, thus providing a rationale for investigations on combination therapy. Likewise, oncogenic switch to FGFR signaling has been suggested to mediate resistance to EGFR-TKIs, as well as to HER2, MET, and angiogenesis inhibitors.
Because of the high degree of homology between the vascular endothelial growth factor receptor 2 (VEGFR2) and FGFR tyrosine kinase domains, various oral multikinase inhibitors that are approved by the US Food and Drug Administration (FDA) or in clinical development (e.g., sorafenib, pazopanib, axitinib, regorafenib, ponatinib, cediranib, nintedanib) are able to inhibit FGFR1 in nanomolar concentrations. Several of these agents, such as dovitinib and brivanib, were in fact developed to have relatively greater selectivity for FGFR kinase than for VEGFR2. Nonetheless, hypertension is a common toxic effect of these agents, which suggests that inhibition of the VEGF pathway remains a major effect of these agents. More selective FGFR inhibitors in early phase clinical testing include AZD4547 and BGJ398. On-target adverse effects, such as hyperphosphatemia and retinal detachment, have been reported.
The results of the Lung Cancer Master Protocol, which includes the FGFR inhibitor AZD4547 in patients with squamous cell carcinoma of the lung, are eagerly awaited (NCT02154490).
c-Ros Oncogene 1
c-Ros oncogene 1 (ROS1) is a proto-oncogene that encodes an RTK closely related to ALK. Notably, ROS1 is expressed only transiently in the lung during murine development and is not found in healthy adult human lung tissue. Its ligand has yet to be identified. A phosphoproteomic analysis of TK signaling demonstrated that ROS1 ranked among the top 10 RTKs activated in NSCLC. Further analysis demonstrated that constitutive activation of ROS1 arose from the presence of SLC34A2–ROS1 fusion in an NSCLC cell line. Multiple other fusion partners have since been reported in NSCLC, such as CD74–, TPM3–, SDC4–, EZR–, LRIG3–, KDELR2–, CCDC6–, and FIG–ROS1. The transforming potential of many of these fusions has been well established. Although localization to the Golgi apparatus of the FIG–ROS1 fusion appears to be crucial for its transforming ability, no discernible pattern of distribution has been found for the other variants. ALK inhibitors have demonstrated preclinical and clinical activity against ROS1-rearranged NSCLCs. This is not surprising given the close homology between ALK and ROS1. However, unlike FGFR, ALK, and RET fusions, in which the mechanism of constitutive kinase activation is attributed to the dimerization domain of the partner protein, the mechanism of activation of most ROS1 fusion proteins remains unclear because most partner proteins lack the dimerization domains.
In an unselected population of patients with NSCLC, the frequency of ROS1 rearrangement is 0.9% to 1.7%, with most cases found in adenocarcinomas. This prevalence can increase to approximately 6% of EGFR/KRAS/ALK wild-type lung adenocarcinomas in East Asian never-smokers. For patients who have lung cancer with ROS1 rearrangement, the objective response rate to pemetrexed appears to be higher and the median progression-free survival longer than in lung cancer patients without the ROS1 or ALK rearrangement. One mechanism of acquired resistance to crizotinib is the acquisition of a secondary mutation in the ROS1 kinase domain that interfered with drug binding in a patient with CD74–ROS1 rearrangement. Cabozantinib is one agent that may overcome resistance mutations in this setting. Aside from crizotinib, other oral agents with anticipated or demonstrated activity against oncogenic ROS1 fusions as well as crizotinib-resistant ALK translocations in NSCLC include the selective ALK inhibitors ceritinib (LDK398), lorlatinib, the dual ALK/EGFR inhibitor brigatinib, and the ROS1/ALK/NTRK inhibitor entrectinib. Crizotinib is a more potent inhibitor than ceritinib. The expansion cohort of a phase I clinical trial with 50 patients with ROS1 mutations treated with crizotinib demonstrated a response rate of 72% with a median duration of 17.6 months. A separate retrospective study of off-label use crizotinib for ROS1-rearranged NSCLC similarly reported an overall response rate of 80% with a median PFS of 9.1 months. Crizotinib has since been approved by the US FDA for the treatment of ROS-1 rearranged NSCLC.
Rearranged During Transfection–RET
The primary mechanism of RET activation in NSCLC occurs through chromosomal rearrangements. Various oncogenic RET fusions have been described by separate investigators since the first publication in late 2011. Fusion partners reported include KIF5B, CCDC6, TRIM33, and NCOA4, all of which contain coiled–coil domains that have oligomerization potential to induce constitutive TK activation. Functional studies indicate that these RET fusions have oncogenic potential.
RET rearrangements, similar to ROS1 and ALK, are observed primarily in lung adenocarcinomas from never-smokers and are also associated with poorly differentiated tumors. Although the overall prevalence is only 1% to 2% in adenocarcinomas, the prevalence can be as high as 16% among never-smokers with nonsquamous histology negative for driver mutations in other oncogenes ( EGFR, KRAS, NRAS, BRAF, HER2, PIK3CA, MEK1, AKT, ALK, and ROS1 ). Vandetanib and cabozantinib are small-molecule inhibitors of multiple kinases, including VEGFR2 and RET, that are currently approved for treatment of metastatic medullary thyroid cancer. Other FDA-approved agents that demonstrate in vitro inhibition of RET include axitinib, sunitinib, regorafenib, sorafenib, and ponatinib (which exhibits the highest potency). Preliminary findings from a phase II study of cabozantinib in patients with NSCLC and RET rearrangements demonstrated objective tumor responses in two of three patients treated. Clinical activity has also been reported with vandetanib. Alectinib also has potent antitumor activity against RET rearrangements, including those with gatekeeper mutations (V804L and V804M). In fact, in one report two of four patients responded to alectinib after failure of other RET inhibitors. Mechanisms of acquired resistance are yet to be established in the clinical setting. Preclinical modeling predicted the emergence of the gatekeeper V804L/M mutation, which is resistant to vandetanib but remained sensitive to ponatinib.
Discoidin Domain Receptors
The members of the discoidin domain family of receptors, DDR1 and DDR2, are unusual RTKs that have as their ligand different types of collagen rather than a typical growth factor. Both DDRs are activated by fibrillar collagens, but only DDR1 can be activated by nonfibrillar collagen. DDR1 is mainly expressed in epithelial cells, whereas DDR2 is found in mesenchymal cells. Novel somatic mutations in lung cancer of both DDR1 and DDR2 were first described in 2005. Mutations are found in both the kinase domain and other regions. Functional characterization of DDR2 mutations, identified in approximately 3% to 4% of squamous cell lung cancers, later established their oncogenic potential.
DDR2-transformed cells appear to require the coordinated activity of both DDR2 and the Src family of kinases for maximal proliferation, which explains their exquisite sensitivity to dasatinib, a dual Src and DDR2 inhibitor, compared with either a DDR2- or Src kinase-specific inhibitor as a single agent. Of the commercially available kinase inhibitors, dasatinib has the most potent activity against DDR2 (Kd value 5.4 nM) compared with other kinase inhibitors such as ponatinib (9 nM), imatinib (71 nM), nilotinib (35–55 nM), sorafenib (55 nM), and pazopanib (474 nM). Clinical responses to dasatinib among patients with DDR2 mutation have been reported. However, its therapeutic index is narrow because of its multiple off-target effects, particularly pleural effusion, and thus DDR2-selective agents are needed.
Tyrosine-Protein Kinase Receptor UFO (AXL) and Proto-Oncogene Tyrosine-Protein Kinase (MER)
The primary ligand for AXL and MER, both members of the TAM (representing the three members: Tyro-3, Axl, and Mer) receptor family of RTKs, is the vitamin K–dependent ligand growth arrest-specific protein 6 (Gas6). Ligand binding induces dimerization that results in stimulation of proliferative and antiapoptotic signaling through the MAPK/ERK and PI3K/AKT pathways. AXL is ubiquitously expressed, whereas MER is expressed in hematopoietic-derived cells, epithelium, and reproductive tissues. Both are involved in regulation of the actin cytoskeleton and tumor cell migration and invasion. They exhibit transforming potential and have complementary roles in promoting tumor cell survival and resistance to chemotherapy in NSCLC. Conversely, either knockdown or pharmacologic inhibition of AXL or MER using sulfasalazine reduces growth, suppresses invasiveness, and restores sensitivity to various cytotoxic agents.
Overexpression of AXL and MER is reported in 93% and 50% to 69% of NSCLCs, respectively. The Gas6 ligand is also frequently expressed in NSCLC, thus providing continuous signaling through autocrine and/or paracrine mechanisms. Overexpression of AXL, which can be upregulated during activation of EMT, appears to mediate resistance to targeted therapies as well as to EGFR and HER2 TKIs. Inhibition of AXL restores sensitivity to EGFR-TKI therapy. A potentially oncogenic AXL fusion product that carries the tyrosine kinase domain and dimerization units (AXL–MBIP) was identified by transcriptome analysis of lung adenocarcinomas. Taken together, these findings highlight the therapeutic potential of targeting AXL and MER. A caveat in drug development against these targets is that both proteins have an essential function in limiting inflammation. Increased inflammation seen in knockout mice lacking both receptors paradoxically fosters a tumor-promoting microenvironment in colitis-associated colon cancer.
Tropomysin Receptor Kinase
The genes NTRK1–3 encode the tropomysin receptor kinase (Trk) proteins Trk A, B, and C, respectively. The Trk receptors are transmembrane proteins critical for the development of both the central and peripheral nervous systems. Rearrangements of NTRK genes are the most common oncogenic mutations of these genes that result in constitutive activation of fusion proteins. NTRK gene rearrangements have been discovered in NSCLC and other malignancies such as colorectal cancer, papillary thyroid carcinoma, glioblastoma, and human secretory breast cancer. One patient with a soft-tissue sarcoma that harbored a LMNA–NTRK1 rearrangement had a dramatic response to the TRK inhibitor LOXO-101. Similarly, a patient with metastatic colorectal cancer with a LMNA–NTRK1 rearrangement experienced a partial response to the pan-TRK inhibitor entrectinib. In NSCLC, MPRIP–NTRK1 and CD74–NTRK1 rearrangments were the first to be reported and were found to be oncogenic. This same study suggested that NTRK1 gene rearrangements are present in 3% to 4% of patients without other known oncogenic alterations, but this may represent fewer than 1% of all patients with NSCLC. Regardless, the responses observed in other malignancies to the TRK inhibitors in development are similarly encouraging for NSCLC.
Nonreceptor Targets
RAS
The RAS superfamily of guanosine triphosphatases (GTPases) consists of three highly related proteins: KRAS, HRAS, and NRAS. These proteins interface with a large number of effectors, including RAF and PI3K. Although they share similar properties, each isoform may have preferential signaling. For example, KRAS is more potent than HRAS in RAF activation, and the opposite is true for PI3K activation. Mutations in NSCLC resulting in constitutive activation of RAS proteins occur predominantly at codons 12, 13, and 61 of KRAS, particularly in smoking-related adenocarcinomas, of which approximately 30% harbor these mutations. Mutant KRAS alleles are also often amplified at higher levels in NSCLC compared with the wild-type allele, similar to observations seen with EGFR and suggesting that the preferential amplification of the mutant copy of the gene has functional significance.
RAC1b, an isoform of the RAC1 GTPase that includes one additional exon, is found to be preferentially upregulated in lung cancer via splice–site mutations. RAC1b appears to promote KRAS-induced lung tumorigenesis, and its expression appears to be associated with sensitivity to MEK inhibition. Inactivating mutations in the tumor suppressor gene NF1 are found in approximately 7% of lung adenocarcinomas. Because NF1 suppresses the activity of GTPase-activating proteins that stimulate the catalytic activity of RAS, its inactivation mimics a hyperactivated RAS phenotype even in the absence of RAS mutations.
Intact signaling through the PI3K pathway, specifically the binding of RAS to PI3K, is also required for tumorigenesis in mouse models of KRAS -driven lung tumors. Other mouse models indicate that nuclear factor-ĸB and cell-cycle targets such as PLK1 and cyclin-dependent kinase (CDK) signaling, particularly CDK4 are essential for proliferation of KRAS -mutant lung adenocarcinoma, with lethal effects seen upon pharmacologic inhibition of these implicated pathways. Additional observations also indicated that inhibition of proteasome function and of transcription factor pathways impaired the growth and increased the apoptosis of KRAS-mutant NSCLC. Of interest is that GATA2 dependency is also found in other similar oncogenically driven NSCLC tumors, such as those mediated by EGFR , NRAS , NF1 , and EML4–ALK.
Data based on KRAS -knockdown experiments showed variable effects on cell viability among KRAS -mutant cell lines, with some KRAS -mutant cell lines appearing not to be dependent on this pathway. The same KRAS -knockdown experiments showed dependency on RAS signaling in various KRAS wild-type cell lines. Based on this finding, a KRAS -dependency gene expression signature was developed that was more predictive of sensitivity or resistance to targeted therapies, such as MEK inhibitors, than was KRAS mutation status itself. Presence of the KRAS -dependency gene expression signature in KRAS -mutant cell lines is associated with a well-differentiated tumor phenotype, whereas induction of EMT results in KRAS independence. A potentially druggable target protein identified from integrated global transcriptome, proteome, and phosphoproteome analysis of a panel of NSCLC cell lines using this KRAS -dependency stratification is lymphocyte-specific tyrosine kinase (LCK). Indeed, KRAS -dependent cell lines were sensitive to LCK inhibition, whereas KRAS -independent cell lines were not. MET inhibition also selectively impaired the growth of KRAS -dependent cell lines, as predicted based on this stratification.
NRAS mutations are present in less than 1% of lung cancers and have been described predominantly in adenocarcinomas. These mutations appear to be more common in current or former smokers. The nucleotide transversion mutations typically associated with smoking appear to be found less frequently in NRAS -mutant NSCLC (13%) than in KRAS -mutant NSCLC (66%). In vitro studies showed that, similar to KRAS mutants, many of the NRAS-mutant cell lines were sensitive to MEK inhibition alone. In one MEK-resistant cell line that displayed high levels of IGF-1R, combination treatment with an IGF-1R and MEK inhibitor showed a greater antiproliferative effect compared with either drug used alone. These results parallel those seen with this combination in KRAS -mutant NSCLC, which exhibits increased dependence on IGF-1R signaling compared with KRAS wild-type cells.
No direct RAS inhibitors have been successfully developed in the clinic as yet. Strategies explored have mainly sought to prevent plasma membrane localization of RAS, such as with the use of farnesyl transferase inhibitors, with disappointing results. More recently, disruption of the interaction with phosphodiesterase δ, which facilitates plasma membrane localization, has been proposed as a novel approach. Biochemical screening identified the derivative deltarasin, which inhibited RAS signaling and suppressed proliferation of KRAS -mutant pancreatic cancer cell lines in vitro and in vivo. Inhibition of the mTOR pathway as monotherapy demonstrates only modest activity in KRAS -mutant NSCLC. MEK inhibitors represented a promising approach for KRAS -mutant NSCLC. In a randomized second-line study of KRAS -mutant NSCLC, the combination of docetaxel with selumetinib (a MEK inhibitor) improved progression-free survival compared with placebo plus docetaxel (5.3 months vs. 2.1 months; HR, 0.58), with objective responses seen only in the selumetinib group (37% vs. 0%). Adverse events were increased in the selumetinib group, such as febrile neutropenia (18% vs. 0%) and asthenia (9% vs. 0%). Recently it was reported in a press release that the SELECT-1 phase III clinical trial that randomized 510 patients to selumetinib or placebo in combination with docetaxel failed to improve progression-free survival.
v-Raf Murine Sarcoma Viral Oncogene Homolog B–BRAF
Mutations in the RAF family most commonly occur in BRAF , whereas mutations in CRAF and ARAF are rare, found in less than 1% of human cancers. Among patients with NSCLC, BRAF mutations are found in both squamous and nonsquamous histologies and tend to occur in smokers. These mutations appear to promote constitutive BRAF–CRAF dimerization, resulting in RAS-independent activation of the MEK/ERK cascade. Dimerization appears to be needed for downstream signaling for either wild-type or mutant BRAF , except for those characterized by high catalytic activity, such as the V600E and G469A mutations, wherein dimerization is not required for biologic function. Oncogenic alterations in BRAF may also arise from chimeric fusion proteins. The SND1–BRAF fusion transcript has been described in 3% of lung adenocarcinomas among never-smokers. A few of these fusion transcripts are present concurrently in specimens with either EGFR or HER2 mutations.
The constitutively activated V600E mutation represents nearly 50% to 60% of the BRAF mutations found in NSCLC. It is associated with micropapillary features, female gender, and poor prognosis. In contrast to RTK-activated cells, which show feedback downregulation of RAF/MEK signaling upon ERK activation ( Fig. 48.1 ), this physiologic feedback inhibition is missing in V600E BRAF -mutant tumors and is accompanied by high levels of MEK kinase activity. The efficacy of MEK inhibitors in BRAF V600E mutants is attributed to this dependency on MEK activity for proliferation and survival. Non-V600E mutations, such as G469A, T599_V600insT, and V600_K601delinsE, demonstrate increased kinase activity relative to wild-type BRAF . However, other non-V600E mutations are known to be kinase-impaired or inactivating (e.g., D594, G466, G496del, and Y472). Nonetheless, ERK activation can still be achieved through heterodimerization with CRAF, thus predicting resistance to selective BRAF inhibitors (BRAFi). These kinase-impaired BRAF mutations, which have weak oncogenic potential, appear to be sensitive to dasatinib.
Tumor responses have been reported among patients with BRAF V600E-mutant NSCLC treated with vemurafenib and dabrafenib. A recently published phase II clinical trial demonstrated a 63.2% overall response rate in patients with BRAF V600E mutations receiving dabrafenib and trametinib in the second line. Despite the clinical success of BRAFi, resistance may develop due to the emergence of KRAS mutations. Other anticipated mechanisms of acquired resistance to BRAFi, based on models of melanoma, include emergence of activating somatic mutations in NRAS or MAP2K1 / MAP2K2 , bypass signaling (e.g., other RTK-mediated pathways such as FGFR), BRAF amplification, or alternative BRAF splice isoforms. MAPK-independent mechanisms also occur, with the PI3K pathway frequently implicated. In contrast to the experience with various TKIs, secondary mutations in the target oncoprotein itself (i.e., BRAF or CRAF ) are yet to be described in clinical samples, although several CRAF mutations generated from random mutagenesis experiments have been identified that can promote CRAF dimerization and confer resistance to RAF inhibitors. The selective advantage from the relief of RAF autoinhibition due to the presence of RAF inhibitors (RAFi) may also paradoxically foster drug dependence for growth.
Mitogen Activated Protein Kinase Kinase–MEK
A somatic activating mutation in the nonkinase region of the kinase in exon 2 of MEK1/2 ( MAP2K1/MAP2K2 ), a dual-specificity serine/threonine and tyrosine kinase, has been reported in approximately 1% of lung adenocarcinomas and renders the cells sensitive to MEK inhibitors. This G to T transversion mutation is known to be related to smoking and is found in specimens from former smokers. Because MEK1/2 activation represents the penultimate step of signaling in the canonical MAPK pathway, its inhibition has potential activity against tumors dependent on MAPK signaling, regardless of MEK mutation status. However, despite high basal ERK phosphorylation in EGFR mutant cells, these cells are uniformly resistant to MEK inhibition because of the feedback mechanism discussed earlier. In addition, MEK inhibition induces positive feedback of PI3K/AKT signaling as well in EGFR- and HER2-driven cancers through an increase in HER3 activation.
MEKi demonstrate heterogeneous effects in KRAS -mutant tumors, which are in part attributed to the presence of activated parallel pathways such as PI3K/AKT/mTOR in KRAS -driven tumors. Thus, synergistic effects have been documented with the combination of MEKi and PI3K inhibitors (PI3Ki), although clinical development is challenging because of the serious toxicities encountered with combination therapy. Results of a preclinical study suggest that an intermittent dosing regimen is effective and may be successful in mitigating toxicity with PI3Ki and MEKi combinations. The effects of MEK inhibition in KRAS -mutant cancer cell lines also tend to be cytostatic, and xenograft models typically show reduction in tumor growth but not tumor regression with MEK inhibition alone. These preclinical features predict the clinical experience thus far with MEK inhibitors used as monotherapy; that is, objective tumor responses are rarely seen. In one pooled shRNA drug-screening approach to identify synthetically lethal combinations with MEKi in KRAS -mutant cancer cells independent of sensitivity to MEK/PI3K inhibition, the antiapoptotic member of the BH3 family of proteins BCL-XL was identified as a promising target. MEK inhibition increases levels of the proapoptotic protein BIM, which, however, is bound and inhibited by antiapoptotic proteins such as BCL-XL. Indeed, the combination of MEKi and inhibitors of BCL-XL (BCL-XLi) caused marked tumor regression in vivo in KRAS -mutant xenografts and in a genetically engineered mouse model of KRAS -driven lung cancer. Nonetheless, this strategy was not universally effective. KRAS -mutant cells exhibiting EMT demonstrated less sensitivity to this combination. Moreover, acquired resistance ultimately emerges.
Phosphoinositide 3-Kinase
Class I PI3Ks are heterodimeric proteins composed of a regulatory and a catalytic p110 subunit that has four isoforms: α, β, δ, and γ. Tissue distribution and function vary according to the isoform, with cell proliferation and growth principally regulated by p110α. Amplification or activating mutations in PIK3CA , which encodes the p110α catalytic subunit, have both been described in NSCLC. Amplification of PIK3CA and mutation of PIK3CA appear to be mutually exclusive. Somatic gain-of-function mutations in PIK3CA can be found in up to 9% of squamous NSCLCs. These mutations most commonly occur either in the helical domain encoded by exon 9 (E542K, E545K), and therefore interfere with binding of the p85α regulatory subunit, or in the kinase domain encoded by exon 20 (H1047R, H1047L). Somatic mutations in the gene encoding p85α, PIK3R1 , occur in approximately 40% of endometrial carcinomas and in approximately 1% of NSCLCs. Although several mutants described in endometrial cancer have increased AKT signaling, others show no appreciable biologic effect. The functional consequences of PIK3R1 mutations in NSCLC are still unknown.
Loss of PTEN, the negative regulator of PI3K, results in a hyperactivated AKT phenotype. Mechanisms implicated in the loss of PTEN include epigenetic silencing (e.g., promoter methylation), posttranslational modification, increased degradation, and mutations or homozygous deletions. Genetic changes in PI3K (amplification or mutation) and mutation of PTEN appear to be more common in squamous cell carcinomas than in adenocarcinoma (9.8% vs. 1.6%, respectively), particularly within the Asian population. Although both activating PIK3CA mutations and inactivating PTEN mutations augment AKT signaling in experimental systems, they do not appear to be functionally redundant in vivo because they can be found concurrently, such as in endometrial cancers. Indeed, in contrast to the PTEN null setting, cell lines with PIK3CA mutations have variable degrees of AKT phosphorylation and often show diminished AKT signaling.
Despite experimental preclinical data suggesting that these mutants can be exquisitely sensitive to PI3K or AKT inhibitors, clinical experience to date suggests that the mutation status alone is not a good predictive marker for tumor response because most patients with tumors harboring either a PIK3CA mutation or PTEN loss appear to have stable disease rather than objective response when treated with these agents. Resistance to PI3K inhibitors is unlikely to arise from mutations at the gatekeeper residue alone, as indicated by modeling experiments showing that the mutated kinase has severely reduced catalytic activity and thus cannot be viable. In a large phase II trial that screened over 1200 patients for PI3K mutations, the 12-week progression-free survival rates in response to buparlisib (BKM120) were 23.3% and 20.0% in squamous ( n = 30) and nonsquamous groups ( n = 33), respectively. Since the prespecified rate of 50% was not met by either group, this trial was halted. Some PI3K inhibitors still in development include the PI3Kα inhibitors BYL719 and taselisib, and the dual PI3K/mTOR inhibitors SF1126 and PQR309.
Concurrent mutations in genes of the MAPK signaling pathway are common in lung adenocarcinomas with PIK3CA mutations. Coexisting mutations that activate MAPK signaling render cells resilient to the effects of inhibiting a single pathway because of built-in redundancy from integration of both pathways to a final common effector, such as 4EBP1 phosphorylation. Combined inhibition of ERK and AKT signaling is thus necessary to suppress tumor growth in such conditions. However, parallel pathway inhibition, although potentially efficacious, may cause greater clinical toxicity as a tradeoff.
Protein Kinase B–AKT
The AKT family of kinases includes three isoforms—AKT1, AKT2, and AKT3—which belong to the protein kinase B family of serine/threonine kinases. Each isoform shows relative specificity, albeit considerable overlap, in its regulation of cellular processes and tissue distribution. These activities include antiapoptosis and cell survival for the ubiquitously expressed AKT1 ; maintenance of glucose homeostasis for AKT2 in insulin-responsive tissues including liver, adipose tissue, and skeletal muscle; and brain development for AKT3 . The oncogenic E17K mutation in exon 4 of the pleckstrin homology domain of AKT1 is uncommon in NSCLC, occurs primarily in the subset with squamous histology, and is generally mutually exclusive with the presence of PIK3CA mutations. This mutation is associated with increased membrane localization, which results in elevated autophosphorylation of AKT1, increased levels of cyclin D1, and reduced sensitivity to an allosteric Akt kinase inhibitor. In contrast, amplification of either AKT1 or AKT2 has been reported collectively in 7% of lung cancers but coamplification of these genes has not been found. Although the reported cases involved small cell and large cell carcinomas as well, most cases appear to involve squamous histology rather than adenocarcinoma.
The PI3K/AKT/mTOR signaling pathway is subject to feedback regulation similar to that of other pathways. Moreover, AKT activates multiple processes besides mTOR. Indeed, inhibition of AKT results in greater than a threefold increase in RTKs, such as HER3, RET, FGFR, and IGF-1R, across several cell lines, supporting the view that activation of AKT causes feedback inhibition of RTK expression. This feedback regulation/inhibition of RTK expression effect appears to be independent of mTOR activity. Induction of HER3 phosphorylation appears to be the most prominent effect of AKT inhibition, particularly in HER2-driven tumors. These findings may provide an explanation for the modest objective responses seen to date with these agents even in patients with an activated PI3K pathway signature.
Mammalian Target of Rapamycin
mTOR interacts with a number of proteins to form two distinct complexes: mTOR complex 1 (mTORC1) and mTOR complex 2 (mTORC2). mTORC2 is characterized by its association with the rapamycin-insensitive Rictor, and the interaction between Rictor and mTOR is mutually exclusive with that of Raptor, the binding partner in mTORC1. Physiologic activation of PI3K/AKT/mTOR signaling results in feedback downregulation of the pathway, with loss of expression of insulin receptor substrate-1 (IRS-1) ( Fig. 48.1 ), which is the major substrate of IGF-1R and insulin receptors. The indolent behavior of several tumor types with an activated mTOR pathway has been ascribed to this negative feedback loop. Inhibition of mTORC1 by rapamycin and its analogs paradoxically increases AKT activity through induction of IGF-1 signaling via inhibition of p70S6K-mediated IRS-1 downregulation.
Unlike mTORC1, which is inhibited by rapamycin and its analogs, mTORC2 is generally insensitive to rapamycin, although prolonged treatment in several models can block mTORC2 assembly to cause its degradation. Because mTORC2 plays an important role in AKT activation, this differential effect of rapamycin on the mTOR complexes also explains the phenomenon of feedback activation that probably underlies the modest responses seen in the clinic with rapalogues. This phenomenon also provided the impetus for the development of small-molecule inhibitors that can inhibit the catalytic activity of both mTORC1 and mTORC2 to avoid or mitigate the feedback AKT activation. In addition, a consequence of mTOR inhibition is feedback activation of RTKs as well as activation of ERK signaling through loss of p70S6K-mediated inhibition of PI3K. These findings provide further evidence supporting the development of dual PI3K/mTOR inhibitors as well as the combination of MAPK and PI3K/AKT/mTOR pathway inhibitors described previously.
LKB1/STK11 is a serine/threonine kinase whose major phosphorylation target, AMP-activated protein kinase (AMPK), upon activation regulates various targets, including the TSC2 gene product tuberin, resulting in mTOR suppression. LKB1/STK11 also phosphorylates related AMPK subfamily members (e.g., BRSK, MARK, NUAK), which have additional functions including regulation of cell polarity and cytoskeletal organization. LKB1/STK11 is the second most commonly mutated tumor suppressor after p53 found in NSCLCs, particularly in adenocarcinomas, accounting for 20% to 30% of cases in the Western hemisphere. Most LKB1 mutations in lung tumors result in the generation of truncated and inactive LKB1 proteins. LKB1 -deficient cells exhibit aberrant upregulation of mTOR signaling with an attenuated AKT activation phenotype (similar to TSC2-deficient models) because of the previously mentioned negative feedback phenomenon in PI3K/AKT/mTOR signaling. However, LKB1 -deficient cells are paradoxically hypersensitive to apoptosis, relative to wild-type cells, during conditions of low-nutrient energy stress (e.g., glucose deprivation) or exposure to AMPK agonists (e.g., AICAR) because of an inability to restore metabolic homeostasis. LKB1 -deficient cells also exhibit alterations in dTTP metabolism and are sensitized to DNA damage and disruption of intracellular dTTP synthesis compared with LKB1 wild-type cells; this finding suggests that deoxythymidylate kinase is a putative synthetic lethal target.
Inactivating mutations of LKB1 appear to be more frequent in patients with a history of smoking, and the higher frequency of these mutations among white compared with Asian populations is thought to be due in part to the higher prevalence of smokers in the West. LKB1 mutations often occur concurrently with KRAS mutations (up to 20% of KRAS mutants) or BRAF mutations (up to 25% of BRAF mutants, particularly non-V600 types). Expression of the glucose transporter GLUT1 is elevated in LKB1 mutant tumors, which results in increased glycolysis and the clinical observation of increased avidity on fluorodeoxyglucose-positron emission tomography scanning.
In a meta-analysis of published data on individual and coincident mutations in NSCLC, LKB1 / KRAS double mutants were found in approximately 5% of adenocarcinomas in the western world and thus represent a distinct subset of NSCLC with epidemiologic and therapeutic relevance. The degree of activation of the MAPK pathway in the LKB1/KRAS double mutants in vivo appeared to be decreased compared with KRAS mutants with wild-type LKB1 status, and signaling was shown to occur primarily through the AKT, FAK, and SRC pathways. That the signaling circuitry is shunted away from MAPK in KRAS and BRAF mutants when LKB1 is inactivated explains why preclinical models of LKB1/KRAS double mutants were resistant to the combination of docetaxel and the MEK inhibitor selumetinib, which otherwise showed synergism in KRAS mutants with wild-type LKB1 . It has been reported that dual LKB1/KRAS mutants exhibited a vigorous apoptotic response to phenformin, a mitochondrial inhibitor as an analog of metformin, regardless of the presence of other additional unique mutations (e.g., P53 loss or PIK3CA mutation). However, efficacy is not sustained beyond 4 weeks, which suggests that the emergence of resistance and/or cellular adaptation will render monotherapy ineffective.
Heat Shock Protein 90
Heat shock protein 90 (HSP90) is one of the most abundant cellular proteins even under nonstress conditions, and at baseline it constitutes 1% to 2% of the total cellular protein content. HSP90 is named after its characteristic upregulation in response to temperature stress (to 4% to 6% of the total cellular protein content) as well as its molecular weight of about 90 kd. This housekeeping protein is an evolutionarily conserved, specialized molecular chaperone with an intrinsic ATPase activity that, along with the assistance of various cochaperones such as the kinase-specific cochaperone Cdc37, ensures the proper folding of nascent polypeptides and the proper assembly of multimeric proteins to prevent aggregation of immature proteins. HSP90 stabilizes and activates more than 200 client proteins, which fall into three main categories: protein kinases (including various mutant oncoproteins discussed previously), steroid hormone receptors, and proteins not involved in signal transduction, such as the transcription factor hypoxia-inducible factor-1alpha. Research suggests some functional selectivity of HSP90 toward regulating most tyrosine kinases and tyrosine-like kinases, in contrast to other protein kinase families wherein nonclient proteins may be found in higher proportions. In addition, members of the PI3K/AKT pathway are subject to regulation by HSP90 throughout the pathway, in contrast to the MAPK pathway (i.e., ERK is not a client protein). Conversely, HSP90 itself is subject to posttranslational modification from client protein kinases such as BRAF and WEE1; this phenomenon is thought to represent a positive feedback loop ensuring chaperone function.
HSP90 is often overexpressed in cancer cells; their reliance on this protein stems from the fact that mutant oncoproteins are often less stable and that additional cellular stresses are often incurred to maintain the malignant phenotype. Inhibition of HSP90 can preferentially affect the mutant oncoproteins compared with their wild-type forms, such as EGFR, HER2, and BRAF, particularly since in some cases, the wild-type form (such as EGFR) may not be a client protein itself and is resistant to degradation induced by the HSP90 inhibitor. This differential protein stability and reliance on HSP90 function of mutant oncoproteins in NSCLC provides a rationale for investigating the role of HSP90 inhibition in this disease, particularly in combination approaches to overcome or prevent the oncogenic switch that is often seen as a mechanism of acquired resistance to kinase inhibitors used in the clinic. Moreover, inhibition of HSP90 has activity against tumor cells with gatekeeper or multiple other secondary mutations mediating acquired resistance to various kinase inhibitors. HSP90 inhibitor monotherapy, such as with AUY992 or retaspimycin, has shown clinical activity in patients with ALK gene rearrangement, including patients with acquired resistance to crizotinib.
Intrinsic resistance to HSP90 inhibitors may occur when specific mutant oncoproteins are innately not sensitive to these agents. Various tumor suppressors are also subject to HSP90 regulation, and their inhibition may adversely spur the proliferation of clones harboring low-penetrant tumor suppressors. WEE1 phosphorylation of HSP90 positively affects HSP90 function, but negatively affects binding of HSP90 inhibitors. Pharmacologic inhibition of WEE1 sensitizes cancer cells to HSP90 inhibitors and thus provides a rationale for this combination. One mechanism of acquired resistance to HSP90 inhibition may arise through feedback activation of the heat shock transcription factor HSF1, a predictable response to currently available HSP90 inhibitors, which results in the induction of other heat shock proteins such as HSP70, HSP27, and HSP90 itself. Lastly, an in vitro model showed that acquired resistance may arise by mutations that increase ATPase activity of HSP90.
HSP90 as a drug target had eluded successful clinical development, largely because of issues regarding drug formulation, toxicities, and modest clinical responses seen with early-generation compounds, such as geldanamycin and its derivatives (17AAG/tanespimycin, 17-DMAG/alvespimycin). The hepatotoxic effects were thought to be related to the nucleophilic reactions arising from the quinone component in the geldanamycin chemotype. Next-generation compounds such as ganetespib, with different structural backbones, were thus developed. A randomized phase II study of docetaxel with or without ganetespib in patients with advanced lung adenocarcinoma showed improved overall survival among patients who received the drug combination, regardless of EGFR or KRAS mutation status. The incidence of febrile neutropenia was higher in the combination group, but no treatment-related deaths were seen. The phase III trial of this combination in the treatment of patients with adenocarcinoma of the lung in the second line was terminated early for futility.
Cyclin-Dependent Kinase
Cyclin-dependent kinases (CDKs) are serine/threonine kinases that, along with their associated cyclins, mediate cell cycle progression and transcription events. According to the classic model, CDK4 or CDK6 and D-type cyclins regulate events in the early G1 phase of the cycle; CDK2–cyclin E triggers the S phase; CDK2 or CDK1–cyclin A regulates the completion of the S phase; and CDK1–cyclin B is responsible for mitosis. Although recurrent mutations of CDKs are rare, gene amplification or protein overexpression of the cyclin partners such as cyclin D1 is frequently encountered in various malignancies, including lung cancer. In turn, the tumor suppressor that negatively regulates the cyclin D1–CDK4 complex, p16INK4 , is often inactivated in lung cancer, most commonly by homozygous deletion, followed by promoter-region methylation, and rarely by point mutations. Cyclin D-dependent kinases (CDK4 and CDK6) phosphorylate retinoblastoma, thereby inhibiting its growth-repressive effects that occur during its hypophosphorylated state. Thus, cells with endogenous expression of functional p16 or mutant retinoblastoma are thought to be mechanistically insensitive to CDK4/6 inhibitors.
Although early-generation pan-CDK inhibitors failed in clinical development because of toxicity, dramatic clinical results and a favorable toxicity profile have been reported in breast cancer using the small-molecule CDK4/6 inhibitor palbociclib (PD0332991), was approved by the US FDA in combination with letrozole for first-line treatment of estrogen receptor positive, HER2-negative advanced breast cancer. These results have renewed interest in this class of agents. As discussed earlier, CDK signaling, particularly of CDK4, appears to be essential for proliferation of KRAS -mutant lung adenocarcinoma. Inhibition of CDK4/6 also appears to be synergistic with trastuzumab in HER2 -amplified breast cancer cell lines, suggesting the potential for similar activity in NSCLC cells with activated HER2 signaling. A single-arm phase II study of palbociclib in patients with previously treated NSCLC with wild-type retinoblastoma and inactive p16 was closed to accrual after no responses were observed in 16 evaluable patients. The Lung Cancer Master Protocol for patients with squamous cell carcinoma of the lung includes an arm with palbociclib.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree