3 The blood neutrophil (Fig 3.1a) is the end-product of an orchestrated sequence of differentiation in the myeloid cells of the bone marrow. The mature cell has a multi-lobed nucleus and four different types of granules in the cytoplasm. Neutrophils have a limited lifespan of around 5–6 days in the blood. Approximately half the cells are included in a normal blood count (the circulating pool), the remainder being in the ‘marginal pool’. The essential function of all these cells is to enter the tissues and combat infection. This requires both migration to the site of infection or tissue injury (chemotaxis) and the destruction of foreign material (phagocytosis). Normal chemotaxis is dependent on the release of chemotactic factors generated by bacteria and leucocytes already present at the infection site. Neutrophils may migrate intravascularly as they navigate healthy tissues to reach the site of tissue injury. Fig 3.1 Leucocytes in the blood. In clinical practice an increase in neutrophils in the blood (‘neutrophil leucocytosis’ or ‘neutrophilia’) is a common accompaniment to infection and tissue injury (Table 3.1). The strain on the neutrophil compartment often leads to younger ‘band forms’ being discharged from the marrow into the bloodstream and the appearance of toxic changes, including coarsened granulation and vacuolation. Occasionally, phagocytosed bacteria are visible (Fig 3.1b).
Neutrophils, eosinophils, basophils and monocytes
Neutrophils
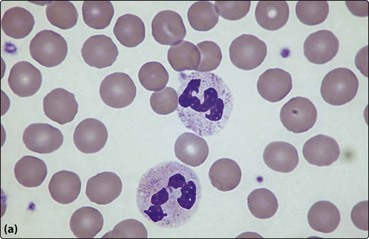
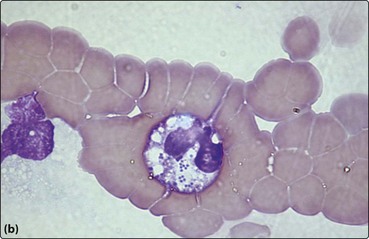
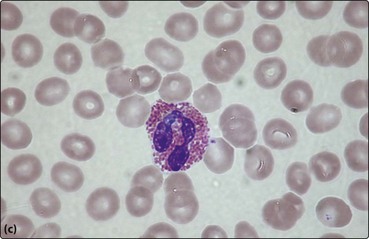
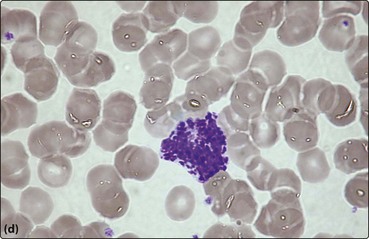
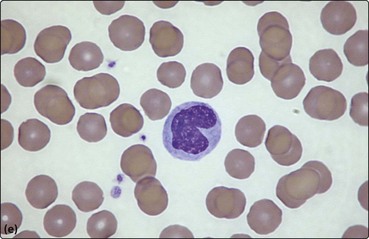
(a) Neutrophils; (b) neutrophil with phagocytosed bacteria; (c) eosinophil; (d) basophil; (e) monocyte.
Neutrophils, eosinophils, basophils and monocytes





