Neurologic Oncology
ASTROCYTOMAS
Parisa Momtaz
Thomas J. Kaley
Definition
Astrocytoma is the most common type of gliomas
Classified under a grading system: Grade 1 (typically benign), grade 2 (low-grade astrocytomas), grade 3 (anaplastic), & grade 4 (glioblastoma multiforme)
Epidemiology/Risk Factors
Clinical Manifestations
Sx related to mass effect, parenchymal infiltration, hydrocephalus, tissue destruction
Associated nausea, vomiting, focal neurologic deficits
Seizures (30%), more common w/low-grade tumors
Diagnosis
Treatment Principles
Surgery
Goal is to obtain histologic dx, reduce mass effect while preserving neurologic function, debulking; can be curative for benign tumors
Stereotactic bx, open bx (primarily for tumors in critical areas where resection would lead to neurologic deficit)
Debulking procedure, subtotal resection, maximal resection
RT
Chemotherapy
Most commonly used agent is temozolomide as it penetrates the blood-brain barrier
Nitrosoureas (eg, carmustine, lomustine), platinum-based therapies
Procarbazine, Lomustine, Vincristine (PCV) for oligodendroglial tumors
Limited benefit; used in combination w/surgery & radiation
Other therapeutic agents
Corticosteroids, anticonvulsant agents, anticoagulation meds
Pathology/Grading Classification
WHO classification as a four-tiered grading system based on key histologic features: ↑ cellularity, mitoses, endothelial proliferation, necrosis
Grade 1
Typically benign. Eg, pilocytic astrocytoma, pleomorphic xanthoastrocytoma, subependymal giant cell astrocytoma
Grade 2: Low-grade Astrocytomas
Diffuse infiltrating low-grade tumors w/only ↑ cellularity
Poor Px factors: Age ≥40 y, tumor ≥6 cm, tumor crossing midline, presence of neurologic deficit prior to resection
Typically are nonenhancing, low attenuation lesions on CT & MRI therefore T2-weighted or FLAIR MRI scans are preferred
Poorly circumscribed, invasive & can transform to higher grade astrocytomas (50% pts will undergo anaplastic transformation in 5 y)
Median survival is approx. 5 y
Tx:
Surgery w/gross total excision w/o compromising function
No consensus on the timing of EBRT. Standard radiation dose is 45-54 Gy.
Limited data for temozolomide as adjuvant Rx.
Grade 3: Anaplastic Astrocytomas
Presence of mitoses distinguishes anaplastic from low grade
Can be both contrast enhancing & noncontrast enhancing on MRI
High propensity to undergo transformation to glioblastoma multiforme
Median survival 24 mos
Tx:
Maximum surgical debulking w/o compromising function
Adjuvant RT prolongs survival
Adjuvant chemotherapy role unclear; single-agent carmustine & PCV have shown prolonged survival in some series & meta-analysis, temozolomide
Recurrence: Temozolomide (Yung WK J Clin Oncol 1999;17:2766) & nitrosourea-based regimens
Grade 4: Glioblastoma Multiforme
Most common & most malignant of the 1° brain tumors
Onset of sx is abrupt & due to mass effect
Pathologic features: ↑ cellularity, endothelial proliferation, tumor necrosis
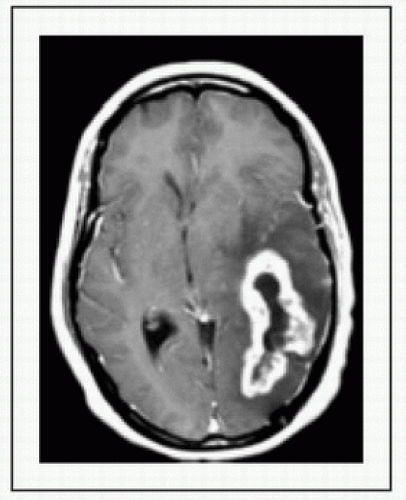
T1-weighted MRI scans w/the use of gadolinium show a ring-enhanced mass
Tx:
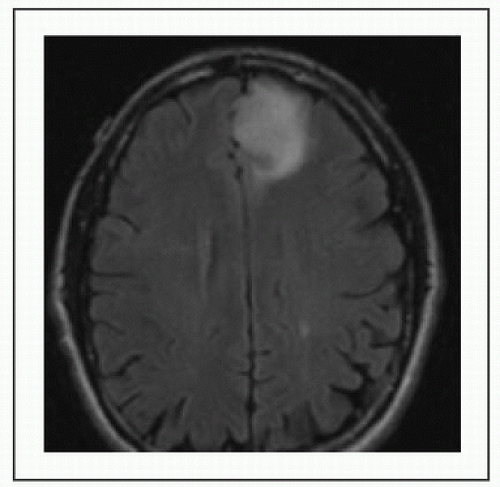 Figure 21-2 Low-grade Astrocytoma T2 FLAIR MSKCC. Courtesy of Dr. T. Kaley |
OLIGODENDROGLIOMAS
Elizabeth Won
Thomas J. Kaley
Definition
1° brain tumors arising from oligodendrocytes
Oligodendrocytes form myelin & provide support for axons
Epidemiology
Incidence 3 per 1000000 in US
Typically seen in fourth to fifth decades; low-grade tumors occur at earlier age
Etiology and Clinical Manifestations
A/w genetic syndrome: Neurofibromatosis-1, tuberous sclerosis, RB1, Li-Fraumeni, & Turcot syndrome
Pathology
Morphology:
Low-grade tumors: “Fried egg” appearance seen on paraffin but not frozen section
High grade (anaplastic oligodendroglioma): High cell density, mitosis, nuclear atypia, microvascular proliferation, & necrosis
Molecular biology:
1p/19q codeletion seen in 60-70% classical oligodendrogliomas, help to distinguish from other types of gliomas. A/w better response to Rx & improved survival in both low-grade & anaplastic tumors. 1p/19q testing recommended in all pts w/oligodendrogliomas. (J Natl Canc Inst 1998;90:1473)
Chromosome 10q loss: A/w poorer response to tx & shortened survival
Workup and Evaluation
MRI brain & spine w/contrast:
Low-grade tumors show ↑ signal on T2 images w/o enhancement. On CT, these tumors appear as low density masses w/o enhancement. Calcifications are suggestive but not specific for oligodendrogliomas.
Anaplastic oligodendrogliomas: Typically characterized by contrast enhancement, but absence does not exclude anaplastic tumor.
|
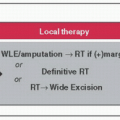
Initial Treatment for Oligodendrogliomas
Optimal management is controversial for low-grade oligodendrogliomas, w/c can be very indolent tumors.
Surgery: When possible, maximal safe resection is recommended. Surgical resection appears to confer survival benefit based on available retrospective data & may delay malignant progression & recurrence. No randomized data comparing surgery vs. conservative approach of delayed surgery after POD in low-grade tumors. Extent of resection should be documented w/a T2-weighted or FLAIR MRI scan w/in 72 h of surgery
Adjuvant Radiation: No consensus on timing of postoperative EBRT. RT is often reserved for tx of recurrent disease. EORTC 22845 trial randomized pts w/lowgrade gliomas to either 54-Gy postoperative radiation or no immediate Rx. 5-y DFS was better w/immediate post-op radiation (44 vs. 37%, p = 0.02); however OS was similar. Long-term follow-up showed no OS benefit, but seizures were better controlled in pts receiving immediate post-op RT (EORTC 22845, Int J Radiat Oncol Biol Phys 2002;52:316 & Lancet 2005;366:985)
Radiation dose: No benefit for higher dose RT, standard is 45-54 Gy.
Adjuvant Chemotherapy: Temozolomide or Procarbazine, lomustine, & vincristine (PCV)
Management of Recurrent or Progressive Disease
Surgery is recommended (if resectable) followed by radiation or chemotherapy if pt already received RT.
Radiation for recurrence if not used in adjuvant setting.
Reirradiation to be considered if recurrence > 2 y after prior RT, new lesion outside of prior RT field, or small lesion
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree