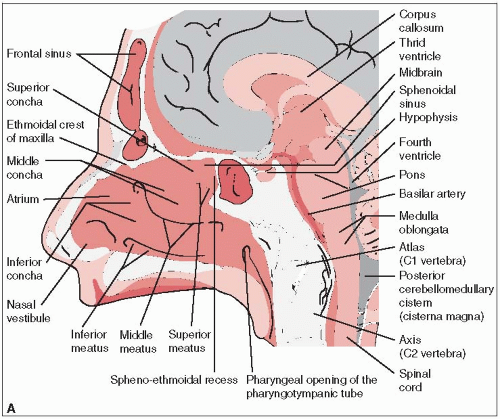
The nasopharynx is roughly cuboidal; its borders are the posterior choanae anteriorly, the body of the sphenoid superiorly, the clivus and first two cervical vertebrae posteriorly, and the soft palate inferiorly (Fig. 14-1).
The lateral and posterior walls are composed of the pharyngeal fascia, which extends outward bilaterally along the undersurface of the apex of the petrous pyramid just medial to the carotid canal. The roof of the nasopharynx slopes downward and is continuous with the posterior wall.
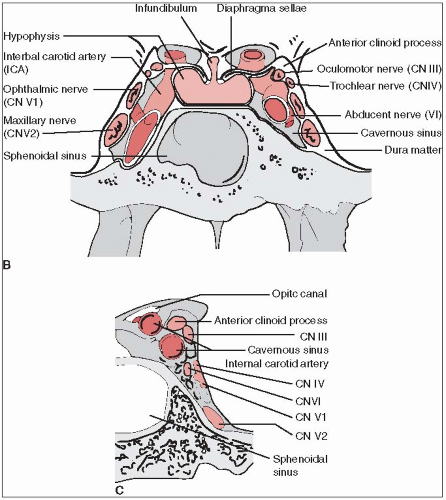
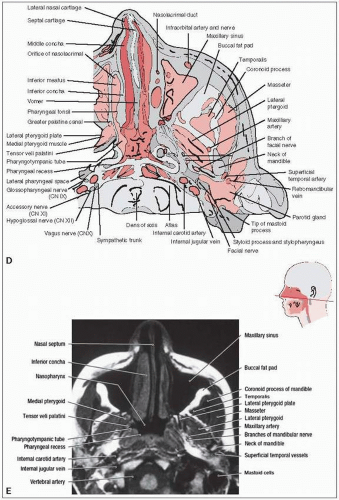
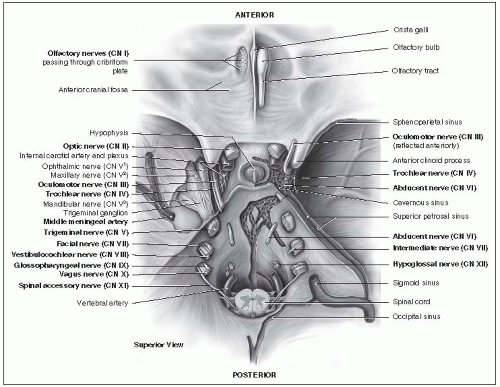
The eustachian tube opens into the lateral wall; the posterior portion of the eustachian tube is cartilaginous and protrudes into the nasopharynx, making a ridge just posterior to the torus tubarius. Just posterior to the torus tubarius is a recess called Rosenmüller’s fossa. Many foramina and fissures are located in the base of the skull, through which several structures pass (Fig. 14-2, Table 14-1). Some are potential routes of spread of nasopharyngeal carcinoma.
Lymphatics of the nasopharyngeal mucosa run in an anteroposterior direction to meet in the midline; from there they drain into a small group of nodes lying near the base of the skull in the space lateral and posterior to the parapharyngeal or retropharyngeal space. This group lies close to cranial nerves IX, X, XI, and XII, which run through the parapharyngeal space.
Another lymphatic pathway from the nasopharynx leads to the deep posterior cervical node at the confluence of the spinal accessory and jugular lymph node chains (10).
A third pathway leads to the jugulodigastric node, which is frequently involved in nasopharyngeal carcinoma, according to Lederman (19).
Carcinoma of the nasopharynx frequently arises from the lateral wall, with a predilection for the fossa of Rosenmüller and the roof of the nasopharynx.
TABLE 14-1 Foramina of the Base of the Skull and Associated Anatomic Structures | |||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| |||||||||||||||||||||||||||||||||||
Tumor may involve the mucosa or grow predominantly in the submucosa, invading adjacent tissues including the nasal cavity. In approximately 5% of patients, tumor extends into the posterior or medial walls of the maxillary antrum and ethmoids (21).
In more advanced stages, the tumor may involve the oropharynx, particularly the lateral or posterior wall.
Upward extension of the tumor through the basilar foramen results in cranial nerve involvement and destruction of the middle fossa.
Th e floor of the sphenoid occasionally may be involved.
Approximately 90% of patients develop lymphadenopathy, which is present in more than 70% at initial diagnosis (21).
The incidence of distant metastasis is not related to the stage of the primary tumor, but does correlate strongly with degree of cervical lymph node involvement. In 63 patients with NO necks, 11 (17%) developed metastatic disease, in contrast to 69 of 93 patients (74%) with N3 cervical lymphadenopathy (26). The most common site of distant metastasis is bone, followed closely by lung and liver (31).
Tumor growth into the posterior nasal fossa can produce nasal stuffiness, discharge, or epistaxis. Occasionally, the voice has a nasal twang.
The orifice of the eustachian tube can be obstructed by a relatively small tumor; ear pain or a unilateral decrease in hearing may occur. Blockage of the eustachian tube occasionally produces a middle ear transudate.
Headache or pain in the temporal or occipital region may occur. Proptosis sometimes results from direct extension of tumor into the orbit.
Sore throat can occur when tumor involves the oropharynx.
Although a neck mass elicits medical attention in only 18% to 66% of cases, clinical involvement of cervical lymph nodes on examination at presentation ranges from 60% to 87% (11, 19).
Some patients present with cranial nerve involvement. In 218 patients, 26% had cranial nerve involvement, although it caused presenting symptoms in only 3% (19). Leung et al. (23) reported a 12% incidence of cranial nerve involvement in 564 patients with primary nasopharyngeal carcinoma; incidence was higher in patients with computed tomography scans (52 of 177, or 29%).
Cranial nerves III through VI are involved by extension of tumor up through the foramen lacerum to the cavernous sinus. Cranial nerves I, VII, and VIII are rarely involved.
A complete history and physical examination includes detailed evaluation of extent of disease in the pharynx (Table 14-2).
Extent of neck node metastases must be assessed, and a search made for distant metastases.
Biopsies must be done of the nasopharynx and adjacent suspicious areas.
The multiplicity of staging systems makes comparison of results from different institutions extremely difficult.
The most commonly used staging system is the American Joint Committee (1) tumor-nodemetastasis (TNM) system (Table 14-3).
Approximately 90% of malignant tumors arising in the nasopharynx are epidermoid or undifferentiated carcinomas; the remaining 10% are mainly lymphoma but may also be plasmacytoma, tumors of minor salivary gland origin, melanoma, rhabdomyosarcoma, and chordoma.
Adenoid cystic carcinoma of the nasopharynx is extremely rare.
Sarcomas occasionally arise from embryonal, vascular, or connective tissue.
Most lymphomas of the nasopharynx are large-cell non-Hodgkin’s lymphomas.
TABLE 14-2 Diagnostic and Staging Workup for Nasopharyngeal Carcinoma | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
Race, age, and gender rarely have prognostic significance (7).
Cranial nerve involvement was not significantly associated with decreased survival in several series (7); however, Sham et al. (29) found it to be the only significant prognostic factor.
Survival decreases as cervical lymph node involvement progresses from the upper to the middle and lower nodes (27).
Bilateral cervical lymph node involvement is an ominous prognostic factor.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree