Summary of Key Points
- •
Multiple primary lung cancers (MPLCs) are increasing in incidence as imaging accuracies improve and resections are better tolerated.
- •
Differentiating MPLCs from intrathoracic metastatic disease is challenging and based primarily on clinical judgment.
- •
Molecular analysis for tumor clonality has the potential to increase accuracy of differentiation between MPLCs and intrathoracic metastatic disease.
- •
Complete resection is the treatment of choice for MPLCs, but preservation of pulmonary parenchyma is essential and therefore the use of sublobar resections is common.
- •
Survival rates following complete resection of synchronous MPLCs are reported as between 35% and 75% with prognosis being decreased in those with N1 and N2 involvement.
- •
Metachronous MPLCs are almost always diagnosed at an early stage in asymptomatic patients as part of surveillance imaging. Survival following resection is typically 40% and determined by the stage of the second cancer.
- •
Stereotactic body radiotherapy is an attractive treatment alternative for early stage MPLC because of its ability to preserve pulmonary parenchyma.
The concept of MPLCs was introduced by Beyreunther in 1924, but remained a rarity for many decades. From 1960 to 1990 only sporadic case series were reported, but it was not until the integration of computed tomography (CT) scanning into lung cancer care that the true magnitude was appreciated. Today, rapid improvements in imaging accuracy, decreased mortality associated with lung cancer resections, increased use of CT scans for routine postoperative surveillance, and integration of mutational analysis for resected cancers are all contributing to a growing cohort of MPLC. Whether presenting as synchronous or metachronous tumors, one of the greatest challenges is differentiating MPLCs from intrathoracic metastatic disease. The first step in that distinction is appropriately recognizing the frequency of MPLCs in the modern era. Rates of less than 5% of all nonsmall cell lung cancers (NSCLCs) from older series are now believed to greatly underestimate the true incidence of MPLCs. High-resolution CT scans also allow for the detection of ground-glass opacities, which are not evident on standard chest x-ray or early generation CT scans. These precancerous lesions and early stage adenocarcinomas have a lepidic growth pattern with a predilection for indolence and multiplicity. Risk factors and prognosis for multifocal adenocarcinomas are different from traditional MPLCs reported in older series. The management and treatment decisions for MPLCs follow the same general principles used for other early stage NSCLCs with special consideration for the preservation of pulmonary parenchyma and vigilant posttreatment surveillance.
Differentiating MPLCs from Metastatic Disease
Patients with multiple nodules at the time of NSCLC diagnosis or a new pulmonary nodule following successful treatment of an early stage NSCLC pose a significant clinical challenge due to the lack of clear criteria that differentiate intrapulmonary metastasis from MPLC. The most widely referenced definition is from 1975, from Martini and Melamed. It is applied most appropriately to metachronous tumors, or to those that have already been resected or found at autopsy, and relies heavily on cell type (i.e., adenocarcinoma or squamous cell carcinoma). Further factors used to refine the criteria include origin in an area of carcinoma in situ, lack of carcinoma in common lymphatics, and lack of extrathoracic metastasis ( Table 32.1 ). This definition is becoming outdated in an era when mutational and molecular analysis can differentiate tumors on a genetic basis.
| Metachronous | Different Histology | |
| Same histology if | Prolonged interval between tumors (typically >2 years) | |
| Development from separate area of carcinoma in situ | ||
Different lobes with:
| ||
| Synchronous | Different Histology | |
| Same histology if | Development from separate area of carcinoma in situ | |
Different lobes with:
| ||
Some investigators have suggested that individual adenocarcinomas can be distinguished based on differences in the proportion of histologic subtypes (i.e., lepidic, papillary, acinar, micropapillary). By contrast, other investigators report that mutational and molecular analysis of somatic changes in tumor DNA can better discriminate between MPLC and metastatic disease. Mutational analysis of the epidermal growth factor receptor and K-ras mutations can be used to differentiate between metastatic and second primary adenocarcinomas of the lung. The utility of this approach is limited by the facts that this type of analysis is only relevant to adenocarcinomas, not all adenocarcinomas harbor these mutations, and expression can be heterogeneous throughout the tumor. Cytogenetic profiles can be used to evaluate the clonal relationship between tumors. Genomic DNA copy number alterations are key events in tumor development and array comparative genomic hybridization can distinguish between clonal tumors (metastasis) and MPLCs. Investigators from the Massachusetts General Hospital reported on 68 patients with multiple resected adenocarcinomas whose tumors were classified as MPLC or metastasis by a comprehensive histologic profiling, including profiling using SNaPshot multiplex polymerase chain reaction. In their study, the 3-year survival rate was significantly improved in patients classified as MPLC by molecular profiling, but not by histologic profiling, indicating improved accuracy with molecular analysis. Although this molecular profiling appears to be more precise than histologic profiling, it is time consuming, expensive, and requires large amounts of genomic DNA. Molecular analysis may not currently be reasonable for use on a case-by-case basis, but it is helping to redefine the frequency and clinical characteristics associated with MPLCs.
Clinical judgment remains critically important in these cases, with biopsy typically having only a small and supplemental role. Patients are generally placed into management categories based on the appearance, location of nodules, and the presence of nodal or extra thoracic metastatic disease. Biopsies are often difficult and typically not helpful in differentiating metastasis and second primaries without molecular analysis because the majority of MPLCs are of the same histology.
MPLCs in the Lung Cancer Staging System
The previous editions of the tumor, node, and metastasis (TNM) classification for lung cancer have been somewhat vague with respect to the classification of lung cancer with multiple pulmonary sites of involvement, which has resulted in marked variability in how these tumors are classified. The creation of homogeneous groups is a goal of cancer staging, but this task is challenging when lung cancer occurs in different pulmonary sites, and the individual cancers exhibit distinct patterns of biologic behavior, recurrence, and survival. In previous lung cancer staging systems, there has been a lack of clarity regarding these distinct patterns of disease as well as ambiguity about how to best apply stage classification.
Definitions have evolved over time for multiple intrathoracic sites of lung cancer in the TNM system. Prior to 1993, all separate tumor nodules were classified as M1. They were then defined as T4 if in a different lobe. In 1997, separate tumor nodules were classified as T4 if in the same lobe and M1 if in a different lobe (ipsilateral or contralateral). In 2010, separate nodules were reclassified as T3 for a same lobe, as T4 if in a different ipsilateral lobe, and as M1 if in a contralateral lobe. However, none of these definitions addressed the concept of variability in appearance and behavior of these additional sites of disease. Furthermore, the seventh edition contained only an elusive mention of ground-glass or lepidic lesions (GG/L) and predated the classification of adenocarcinoma histologic subtypes.
In the eighth edition of TNM classification, four distinct disease patterns were identified for lung cancers with multiple sites of pulmonary involvement and clear instructions were provided on how to apply the TNM classifications to each pattern of disease. The four disease patterns include: (1) synchronous primary lung cancers, (2) multiple GG/L nodules, (3) solid primary lung cancer with one or more separate solid tumor nodule(s) of the same histologic type, and (4) pneumonic type of lung cancer, a diffuse form that is radiologically similar to pneumonia. The radiographic and pathologic features of each of these four disease categories are outlined in Table 32.2 . Second primary lung cancers and GG/L are each recognized as variants of MPLCs. In patients with second primary cancers, each tumor is staged with a unique TNM. GG/L cases are also viewed as independent tumors, but are more interrelated with a strong predilection for multiplicity and lack of lymphatic involvement and are therefore recommended to be staged with the T based on the highest T lesion and “#/m” indicating multiplicity and a single N and M designation. Solid tumors with separate solid nodules and pneumonic lung cancer are not variants of MPLC, but are rather variants of advanced intrathoracic spread of a single tumor and are therefore staged as T3 if spread is limited to a single lobe, T4 if spread is to a single lung, and M1 if bilateral.
| Multiple Primary Lung Cancer | Single Lung Cancer With Intrathoracic Spread | |||
|---|---|---|---|---|
| Eighth Edition Staging Category | Second Primary Lung Cancer | Multifocal GG/L Nodules | Separate Tumor Nodule | Pneumonic Type of Lung Cancer |
| Imaging Features | ≥2 distinct masses with imaging characteristic of lung cancer (e.g., spiculated) | Multiple ground-glass or part-solid nodules | Typical lung cancer (e.g., solid, spiculated) with separate solid nodule | Patchy areas of ground glass and consolidation |
| Pathologic Features | Different histotype or different morphology by comprehensive histologic assessment | Adenocarcinomas with prominent lepidic component (typically varying degrees of AIS, MIA, and LPA) | Distinct masses with the same morphology by comprehensive histologic assessment | Same histology throughout (most often invasive mucinous adenocarcinoma) |
| Staging | Separate cTNM and pTNM for each cancer | T based on highest T lesion with “#/m” indicating multiplicity; single N and M | Location of separate nodule relative to primary site determines if T3, T4, or M1a; single N and M | T based on size if in single lobe, T4 or M1a if in different ipsilateral or contralateral lobe; single N and M |
Synchronous Primary Lung Cancers
The improved resolution of CT imaging has led to increased rates of NSCLC patients presenting with multiple nodules at initial diagnosis. The definitions for synchronous MPLC remain ambiguous, even though treatment algorithms and prognosis are dramatically different from those for patients with multiple nodules from the same tumor. Prognosis for these patients is not as good as those who present with a single primary tumor, but far better than those with widely metastatic disease. Most feel that classifying all of these as intrathoracic metastatic disease greatly “over stages” a significant number of patients with synchronous primary early stage tumors, and denying local therapy may miss the potential for cure. The lack of uniformity for precise identification and definitions for synchronous primary NSCLC has resulted in a paucity of large series of homogeneously treated patients.
Patient Evaluation
Recent trials support an aggressive approach to the treatment of patients with more than one nodule suspicious for early stage NSCLC with the understanding that these may represent MPLC, but a thorough preoperative assessment is essential to rule out metastatic disease and assure the patient has adequate cardiopulmonary reserve to tolerate local therapy for both cancers. Preoperative assessment includes routine pulmonary function tests because these patients may require multiple resections, CT scan of the chest, and whole-body positron emission tomography (PET). Additional tests considered essential include brain imaging by magnetic resonance imaging (MRI) or CT and pathologic mediastinal staging, even in cases of CT-negative and PET-negative mediastinal nodes. Every attempt should be made to exclude the possibility that this may represent intrathoracic metastatic disease prior to local intervention.
Surgical Resection and Outcome
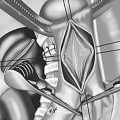
Once two nodules are deemed to be synchronous early stage MPLCs, careful planning is needed to adequately treat each while preserving pulmonary parenchyma. The vast majority of large series of synchronous MPLCs involve patients who undergo resection of both cancers. Five-year survival for resected patients ranges from 16% to 76% but is improved in more recent series and in those with a predominance of multifocal adenocarcinoma, which has a more indolent behavior ( Table 32.3 ). A 2013 meta-analysis specifically looked at prognostic factors and outcomes of resections for synchronous MPLCs. The authors specifically attempted to exclude carcinoid tumors and pure adenocarcinoma in situ from the analysis, because of their indolent nature. Tumors were considered synchronous if they occurred within 2 years of initial resection. Four hundred and sixty-seven patients were analyzed from six different studies conducted from 1983 to 2011, which coincides with the integration of CT scanning into NSCLC care. The majority of patients (67%) had the same histology in both tumors. Between 16% and 78% of patients were treated with at least one sublobar resection, and half of the tumors were unilateral. Two tumors were seen in most patients, but 11% had three or more. Median overall survival was 52 months, far more in line with survival for early stage than metastatic NSCLC. Risk factors for poor outcome included male gender, increasing age, nodal involvement, and unilateral tumors, with N2 involvement being the strongest predictor of poor outcome. Those patients with favorable status with regard to these four prognostic factors (gender, age, lymph nodes, and laterality) had a 5-year survival of 82% in a pooled survival estimate from the six trials compared with only 43% for those with any poor prognostic risk factors. Factors such as lung function, tumor size, and adjuvant therapies were not included in the analysis.
| Author(s) | Years | N | Multiple Adenocarcinoma (%) | Bilateral (%) | 5-y Survival (%) | Poor Prognostic Factors |
|---|---|---|---|---|---|---|
| Riquet et al. | 1983–2005 | 118 | 57.6 | 7 | 23.4 | Location in different lobe |
| Okada et al. | 1985–1996 | 28 | 21 | 25 | 70 | Stage III or IV |
| Trousse et al. | 1985–2006 | 125 | 52 | 27 | 34 | Low FEV 1 Sublobar resection Pneumonectomy Male pN1-2 symptoms |
| Vansteenkiste et al. | 1990–1994 | 35 | 14 | 20 | 33 | pN1-2 |
| Chang et al. | 1990–2006 | 92 | 87 | 12 | 35 | pN1-2 |
| De Leyn et al. | 1990–2007 | 36 | 12 | 100 | 38 | N/R |
| Bae et al. | 1990–2008 | 19 | 36 | 37 | 51 | Histologic discordance Primary tumor stage |
| Rostad et al. | 1993–2000 | 94 | 52 | 4 | 28 | Adenocarcinoma Male Older age Pneumonectomy |
| Finley et al. | 1995–2006 | 175 | 76 | 45 | 64 (3 y) | >Stage IA Male gender |
| Mun and Kohno | 1995–2008 | 19 | 84 | 100 | 76 | N/R |
| Fabian et al. | 1996–2009 | 67 | 31 | 66 | 53 | Higher clinical stage Incomplete preoperative staging |
| Shah et al. | 1997–2010 | 47 | N/R | 100 | 35 (3 y) | None identified |
| Zhang et al. | 2010–2014 | 285 | 88 | 33 | 78 | Male gender Symptoms LN involvement |
A consistent finding throughout the literature is that approximately one-third of synchronous MPLCs are detected incidentally at the time of resection. Frozen section is typically not informative in these circumstances because histology is typically the same. An R0 resection is recommended, and this typically requires a sublobar resection for one or both of the lesions. If an R0 resection is not possible, a diagnostic biopsy is recommended to help direct further care. Hilar and mediastinal lymph node evaluation is essential for these patients. As with other early stage NSCLC patients, there is a risk of a false-negative result on preoperative evaluation and N2 involvement is strongly associated with poor prognosis.
Metachronous Primary Lung Cancers
Incidence
Similar to synchronous MPLCs, the definition for metachronous tumors remains somewhat ambiguous. Increases in the incidence of metachronous MPLC in recent literature can be attributed to (1) more patients presenting with early stage NSCLC, (2) more patients surviving treatment for early stage NSCLC, and (3) increased use of CT scans as part of routine postoperative surveillance. Series of resected NSCLC patients prior to the year 2000 typically reported rates of 0.5% to 3.2% in resected patients. Large series from 2001 and 2002 reported rates of 4.1% and 4.6%, and a 2013 report of 1294 patients from the Memorial Sloan Kettering Cancer Center (MSKCC) found 7% incidence of second primary lung cancers. Although this was substantially higher than that reported by previous series, it is important to note that this is lower than the rate of recurrence within the same population (20%). In the MSKCC series, the rate of tumor recurrence following resection begins to decrease after 4 years, whereas the rate of a second primary NSCLC increased steadily over time, going from a rate of 3/100 person-years in the first 2 postoperative years to 6/100 person-years 5 years from resection. Most series report an average interval of 30 months to 50 months between initial and subsequent tumors ( Table 32.4 ).