There is no cure for metastatic pheochromocytoma or metastatic paraganglioma (PPGL). The first step in the management of metastatic PPGL is to assess the rate of tumor progression and, once determined, provide a proportionate treatment. Herein we demonstrate the role for gallium 68 (Ga-68) 1,4,7,10-tetraazacyclododecane-1,4,7,10-tetraacetic acid (DOTA)-octreotate (DOTATATE) positron emission tomography (PET) computed tomography (CT) in assessing total tumor burden.
Case Report
The patient was a 58-year-old woman seen in endocrine consultation for metastatic pheochromocytoma. She underwent left adrenalectomy 3 years previously for the removal of a 3-cm adrenal pheochromocytoma. Before surgery both metanephrine and normetanephrine were increased above the upper limit of the reference ranges in the blood and urine and they reportedly normalized postoperatively. She had no other follow-up until the current visit, when she presented with paroxysmal symptoms. Her spells, 15 minutes in duration, started with a shaky sensation followed by head pulsations; she said it felt like “my head is going to pop.” There was no family history of pheochromocytoma. She had a history of right thyroid lobectomy for a goiter that proved to be Hashimoto thyroiditis. She had chronic hypertension that was treated with a β-adrenergic blocker (carvedilol 6.25 mg daily), angiotensin-converting enzyme inhibitor (enalapril 5 mg daily), and a mineralocorticoid receptor antagonist (spironolactone 50 mg daily). On physical examination her body mass index was 40.9 kg/m 2 , blood pressure 126/74 mmHg, and heart rate 76 beats per minute.
INVESTIGATIONS
The laboratory tests confirmed recurrent pheochromocytoma ( Table 48.1 ). She declined germline genetic testing.
| Biochemical Test | Result | Reference Range |
| Sodium, mmol/L | 142 | 135–145 |
Potassium, mmol/L | 4.8 | 3.6–5.2 |
Creatinine, mg/dL | 1.1 | 0.6–1.1 |
Plasma metanephrine, nmol/L | 4.1 | <0.5 |
Plasma normetanephrine, nmol/L | 8.0 | <0.9 |
24-Hour urine: | ||
Metanephrine, mcg | 2402 | <400 |
Normetanephrine, mcg | 2771 | <900 |
Norepinephrine, mcg | 107 | <80 |
Epinephrine, mcg | 34 | <20 |
Dopamine, mcg | 278 | <400 |
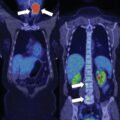
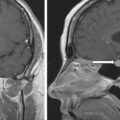
CT scan of the abdomen and pelvis revealed no sign of recurrent pheochromocytoma. F-18 fluorodeoxyglucose (FDG) PET-CT scan showed moderate FDG uptake (maximum standard unit value 5.7) in the left acetabular roof, right thyroidectomy and enlarged residual left thyroid lobe with intense FDG uptake, and focal moderate FDG uptake in the gastric antrum near the pylorus ( Fig. 48.1 ). Thyroid ultrasound confirmed Hashimoto thyroiditis and explained the thyroid FDG uptake. Thus the FDG-PET-CT showed minimal disease and did not adequately account for the markedly abnormal laboratory findings. Magnetic resonance imaging of the pelvis showed a well-marginated lesion within the left acetabulum that measured 2.3 cm in maximum dimension. In addition, multiple small round areas of T2 hyperintensity were present throughout the pelvis and spine, the largest of which were in the left posterior iliac crest, the left iliac wing, sacrum, and right ilium—all consistent with metastases. The findings on MRI confirmed the suspicion that FDG-PET scan was not detecting the full extent of her disease. I-123 metaiodobenzylguanidine (MIBG) scintigraphy showed innumerable foci of MIBG uptake involving the thorax, abdomen, pelvis, and left thigh ( Fig. 48.2 ). CT of the left femur showed a 2.3 × 2.3 × 2.6–cm marrow replacing lesion in the distal left femoral meta-diaphysis compatible with metastasis.