Metabolic Complications
Harold E. Carlson
I. HYPERCALCEMIA
A. Mechanisms. Cancer is the most common cause of hypercalcemia in hospitalized patients. Hypercalcemia usually results from excessive bone resorption relative to bone formation.
1. Bone metastases. Most tumors capable of bone metastasis (see Chapter 33, Section I) can also produce hypercalcemia. Local production of various substances by tumor cells may stimulate osteoclastic bone resorption.
2. Ectopic parathyroid hormone (PTH) secretion appears to be rare.
3. Humoral hypercalcemia of malignancy is caused by production of a PTH-like substance called PTH-related peptide (PTH-RP) by a variety of carcinomas (squamous tumors of many organs, hypernephroma, parotid gland tumors). PTH-RP has bone-resorbing activity and interacts with the renal PTH receptor to stimulate renal calcium resorption. PTH-RP is not measured in serum PTH assays.
4. Vitamin D metabolites (e.g., 1,25-dihydroxyvitamin D) may be produced by some lymphomas; these metabolites promote intestinal calcium absorption.
5. Prostaglandins and interleukin-1 produced by various tumors may occasionally cause hypercalcemia, perhaps by enhancing bone resorption.
6. Tumors rarely or never associated with hypercalcemia despite high frequencies of bone metastases:
a. Small cell lung cancer
b. Prostate cancer
c. Colorectal cancer
B. Diagnosis
1. Symptoms of hypercalcemia depend both on the serum level of ionized calcium and on how fast the level rises. Rapidly rising serum calcium levels tend to produce obtundation and coma with only moderately elevated serum calcium levels (e.g., 13 mg/dL). Slowly rising serum calcium levels may produce only mild symptoms, even with serum levels exceeding 15 mg/dL.
a. Early symptoms
(1) Polyuria, nocturia, polydipsia
(2) Anorexia
(3) Easy fatigability
(4) Weakness
b. Late symptoms
(1) Apathy, irritability, depression, decreased ability to concentrate, mental obtundation, coma
(2) Profound muscle weakness
(3) Nausea, vomiting, vague abdominal pain, constipation, obstipation
(4) Pruritus
(5) Abnormalities of vision
2. Differential diagnosis of hypercalcemia. Idiopathic hypercalcemia is not a tenable diagnosis in adult patients. More and more often, benign causes of
hypercalcemia are recognized to occur in patients with cancer. The possible etiologies of hypercalcemia include the following:
hypercalcemia are recognized to occur in patients with cancer. The possible etiologies of hypercalcemia include the following:
a. Malignancy
(1) Metastases to bone
(2) Secretion of PTH-like or other humoral factors
(3) Production of vitamin D metabolites
b. Primary hyperparathyroidism
c. Thiazide diuretic therapy
d. Vitamin D or vitamin A intoxication
e. Milk-alkali syndrome
f. Familial benign hypocalciuric hypercalcemia
g. Others
(1) Immobilization of patients with accelerated bone turnover (e.g., Paget disease or myeloma)
(2) Sarcoidosis, tuberculosis, and other granulomatous diseases
(3) Hyperthyroidism
(4) Lithium administration
(5) Adrenal insufficiency
(6) Diuretic phase of acute renal failure
(7) Severe liver disease
(8) Theophylline intoxication
3. Laboratory studies. All patients with cancer and polyuria, mental status changes, or gastrointestinal symptoms should be evaluated for hypercalcemia.
a. Routine studies
(1) Serum calcium, phosphorus, and albumin levels
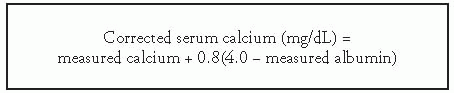
(a) Ionized calcium constitutes about 47% of the serum calcium and is in equilibrium with calcium bound to proteins, especially to albumin. Roughly 0.8 mg of calcium is bound by 1 g of serum albumin. An alkaline pH (e.g., resulting from repeated vomiting because of hypercalcemia) tends to decrease the fraction of ionized calcium. When serum albumin is low, the measured serum calcium can be corrected (to a normal albumin concentration of 4 g/dL) using the following formula:
(b) Long-standing hypercalcemia with hypophosphatemia suggests primary hyperparathyroidism.
(2) Serum alkaline phosphatase. Elevated levels may be due to either hyperparathyroidism or metastatic disease to the bone or liver. Normal levels are typical in cases of hypercalcemia produced by myeloma.
(3) Serum electrolytes. Serum chloride concentrations are frequently elevated in primary hyperparathyroidism. Renal tubular acidosis may complicate chronic hypercalcemia.
(4) Blood urea nitrogen (BUN) and serum creatinine. The direct effect of hypercalcemia on the kidneys can result in nephrogenic diabetes insipidus with defective renal tubular water conservation (i.e., symptoms of polyuria) leading to dehydration and azotemia.
(5) Electrocardiogram (ECG). Hypercalcemia results in relative shortening of the QT interval and prolongation of the PR interval. The T wave widens at blood levels above 16 mg/dL, paradoxically lengthening the QT interval.
(6) Radiographs of the abdomen and bones
(a) Nephrolithiasis is rare in hypercalcemia caused by malignancy and suggests hyperparathyroidism.
(b) Nephrocalcinosis and other ectopic calcifications are common in long-standing hypercalcemia.
(c) Subperiosteal bone resorption is pathognomonic of hyperparathyroidism, but diffuse osteopenia is the most common radiologic finding in this condition.
b. Further studies. Results from preliminary evaluation may indicate the need for measuring serum PTH levels or for performing other tests.
(1) Evidence for concomitant primary hyperparathyroidism
(a) Documented long history of hypercalcemia or renal stones
(b) Radiographic evidence of hyperparathyroid bone disease (subperiosteal reabsorption, osteitis fibrosa cystica, or salt-and-pepper skull)
(c) Hyperchloremic acidosis, particularly with a serum chloride-tophosphate ratio ≥34
(d) Elevated serum PTH level in the presence of hypercalcemia
(e) Absence of hypocalciuria; if the ratio of calcium clearance to creatinine clearance in a 24-hour urine specimen is <0.01, the patient probably has familial hypocalciuric hypercalcemia, which can otherwise mimic primary hyperparathyroidism. Note, however, that vitamin D deficiency must first be corrected in order to accurately assess urinary calcium excretion.
(2) Evidence for humoral hypercalcemia of malignancy
(a) Low or low-normal serum PTH levels in the presence of hypercalcemia
(b) Elevated serum level of PTH-RP
(c) Metabolic alkalosis
(d) Low serum level of 1,25-dihydroxyvitamin D
4. When should neck surgery for primary hyperparathyroidism be considered? Both primary hyperparathyroidism and humoral hypercalcemia of malignancy are characterized by hypercalcemia and, with many cancers, elevated urinary excretion of cyclic adenosine monophosphate. Parathyroid surgery is justified if all of the following apply:
a. Clinical and laboratory findings (see earlier) suggest hyperparathyroidism.
b. The malignancy is under control, and the patient’s expected survival is reasonably long.
c. The general condition of the patient makes the surgical risk acceptable.
d. The hypercalcemia is severe enough to warrant treatment. Mild hypercalcemia (e.g., ≤11.5 mg/dL) caused by primary hyperparathyroidism may remain stable and asymptomatic for many years and may never produce clinically significant complications during the patient’s remaining life span.
e. Parathyroid scanning with technetium-99m sestamibi or neck sonography demonstrates a probable parathyroid adenoma. Neck exploration may also be undertaken in patients with negative radiologic studies but convincing biochemical findings of primary hyperparathyroidism; however, in such cases, one must carefully weigh the possible benefits of surgery
against the possibility of greater surgical morbidity and resultant chronic hypocalcemia.
against the possibility of greater surgical morbidity and resultant chronic hypocalcemia.
C. Management
1. Acute, symptomatic hypercalcemia should be treated as an emergency.
a. Hydration and saline diuresis. Achieving and maintaining normal intravascular volume and hydration are the cornerstones of promoting urinary calcium excretion. Normal saline containing potassium chloride (KCl; 10 mEq/L) is given at a dosage of 2 to 3 L per day IV.
(1) Fluid intake and output and body weight are carefully monitored. Patients are evaluated for evidence of congestive heart failure two or three times daily. Patients with a history of congestive heart failure or renal insufficiency should be monitored with central venous pressure (CVP) measurements. If necessary, furosemide may be given to treat volume overload.
(2) Blood levels of calcium, potassium, and magnesium are measured every 8 to 12 hours, and concentrations of cations in the IV solutions are adjusted.
(3) Treatment is continued until the blood calcium concentration is below 12 mg/dL. Central nervous system manifestations in elderly or comatose patients may not improve until normal blood calcium levels are maintained for several days.
(4) More vigorous administration of fluids (e.g., 12 to 14 L over 24 hours) and diuretics (e.g., every 1 to 2 hours) requires excellent cardiac and renal function and necessitates close monitoring in an intensive care unit. Treatment at this intensity is rarely necessary for patients with malignancies.
b. Bisphosphonates are potent inhibitors of osteoclast activity and are effective in the treatment of hypercalcemia of malignancy. These drugs are relatively free of significant adverse effects. Zoledronate (Zometa) is the most effective of the available drugs; it is given as a single IV infusion of 4 mg in 100 mL of normal saline over 15 minutes. Pamidronate (Aredia) is slightly less effective; it is given as a single IV infusion of 60 to 90 mg in 250 to 500 mL of normal saline over 2 to 4 hours. With either drug, significant reductions in serum calcium occur in 1 to 2 days and generally persist for several weeks. Common side effects of both drugs include fever, nausea, and constipation; both drugs may also cause hypocalcemia, hypophosphatemia, and increased serum creatinine. Patients should be well hydrated both before and after administration of IV bisphosphonates. Doses may be repeated every 7 to 30 days.
A potential adverse effect of bisphosphonates is osteonecrosis of the jaw. In this condition, patients typically develop a painful area of exposed, necrotic bone, usually on the medial aspect of the mandible. The majority of cases have occurred after repeated IV administration of potent bisphosphonates for malignancy and may be precipitated by dental surgery; poor oral hygiene may also play a role. Although prospective data are scanty, some authorities have recommended that patients about to begin IV bisphosphonate therapy have routine dental care performed before treatment starts and biannually thereafter; patients who have already received >3 months of drug therapy have been cautioned to avoid or postpone extensive dental surgery, if possible. Treatment of osteonecrosis of the jaw usually consists of antibiotics and oral rinses; it is not yet clear if discontinuation of bisphosphonates is beneficial.
c. Gallium nitrate (Ganite), a potent inhibitor of bone resorption, is given intravenously in a dose of 200 mg/m2 daily for 5 days. Serum calcium levels fall within a few days and remain normal for about 1 week. Renal function may worsen during gallium nitrate therapy, and the drug should not be given if the serum creatinine level is higher than 2.5 mg/dL.
d. Mithramycin (plicamycin). This drug inhibits bone resorption by reversibly poisoning osteoclasts. Mithramycin, 25 µg/kg, is given by rapid infusion into a well-established IV line; serum calcium levels are lowered in 24 to 48 hours. The dose may be repeated every 3 to 4 days. Hypocalcemia is averted by measuring blood calcium levels every 1 or 2 days or when mental status changes or tetany develops. Other important toxicities of mithramycin are discussed in Chapter 4, Section III.I. The drug is contraindicated in the presence of severe thrombocytopenia or severe hepatocellular dysfunction. In patients with renal failure, mithramycin may be given in lower doses (10 µg/kg), but calcitonin is preferred in these cases.
e. Calcitonin is useful for rapid reduction of blood calcium levels. Calcitonin can be given when diuresis or other drugs are contraindicated or ineffective (e.g., in severe thrombocytopenia, renal failure, congestive heart failure). The drug inhibits bone resorption and increases renal calcium clearance. Blood calcium levels are decreased within 2 to 3 hours of administration. The effect is transient but may be prolonged to 4 or more days by concurrent administration of prednisone, 10 to 20 mg given three times daily. Allergy is the only important complication of therapy. Synthetic salmon calcitonin is given in a dose of 4 U/kg (Medical Research Council Units) SC or IM every 8 to 12 hours; the dose may be increased to 8 U/kg every 8 to 12 hours if needed.
f. Dialysis. Peritoneal dialysis and hemodialysis rapidly lower blood calcium levels but are rarely used.
g. Dangerous therapies that have little clinical usefulness and are not recommended:
(1) Intravenous phosphates (extraosseous calcification)
(2) Intravenous sodium sulfate (hypernatremia, heart failure)
(3) Calcium-chelating agents (severe renal damage)
2. Chronic hypercalcemia. Ambulation is encouraged to minimize bone resorption that accompanies immobilization. Liberal fluid intake (2 to 3 L/d) is prescribed. Foods containing large amounts of calcium, such as milk products, are avoided. Thiazide diuretics aggravate hypercalcemia and should not be taken. Treatment of the underlying malignancy may be beneficial.
a. Glucocorticoids. Prednisone, 20 to 40 mg PO daily, or hydrocortisone, 100 to 150 mg IV every 12 hours, may be used for patients with tumors that are sensitive to glucocorticoids (e.g., lymphoma, multiple myeloma). Glucocorticoids also increase renal calcium excretion.
b. Bisphosphonates. Zoledronate (4 mg IV) or pamidronate (60 to 90 mg IV) may be given every 7 to 30 days as needed to control hypercalcemia (see Section I.C.1).
c. Phosphates given orally lower blood levels by binding calcium in the gut. Because this may compromise renal function, effects of therapy should be monitored. Diarrhea nearly always accompanies phosphate therapy and is treated with diphenoxylate (Lomotil), 2 to 5 mg PO, with each dose of phosphate. Diarrhea may also be reduced by diluting the liquid or powder forms. The daily dose is 1 to 6 g of phosphate. One gram of inorganic phosphate is supplied by the following preparations:
(1) Fleet Phospho-soda, liquid, 6.7 mL
(2) Neutra-Phos, four capsules or 1 teaspoon of powder (Neutra-Phos-K contains no sodium)
(3) K-Phos Original Formula, six tablets (contains no sodium)
d. Prostaglandin inhibitors, such as aspirin and indomethacin, produce variable and inconsistent lowering of calcium levels but may be tried in patients with refractory hypercalcemia.
II. HYPOCALCEMIA
A. Mechanisms
1. Paraneoplasia. Hypocalcemia is an extremely rare paraneoplastic syndrome.
a. Rapid uptake of calcium. Patients with osteoblastic bone metastases may occasionally develop hypocalcemia due to uptake of calcium in the bone lesions. In addition, patients with bone metastases from prostate or breast cancer who are treated with hormonal agents may develop hypocalcemia, supposedly because of rapid bone healing. Calcifying chondrosarcoma is a rare tumor that has been associated with hypocalcemia.
b. Calcitonin production by medullary carcinoma of the thyroid rarely causes hypocalcemia.
2. Magnesium deficiency. Magnesium is necessary both for the secretion of PTH and for its peripheral action. Hypomagnesemia results in hypocalcemia that does not respond to calcium replacement therapy. Magnesium deficiency occurs in the following circumstances:
a. Patients who have prolonged nasogastric drainage
b. Patients who receive parenteral hyperalimentation without magnesium replacement
c. Cisplatin therapy-induced renal tubular dysfunction with urinary magnesium loss
d. Chronic diuretic therapy or diuresis due to glycosuria
e. Chronic alcoholism (alcohol interferes with renal conservation of magnesium)
f. Chronic diarrhea
3. Other causes of hypocalcemia
a. Therapy for hypercalcemia, especially if using IV bisphosphonates or mithramycin
b. Hypoalbuminemia
c. Hyperphosphatemia (see Section III)
d. Pancreatitis
e. Renal disease
f. Hypoparathyroidism
g. Pseudohypoparathyroidism
h. Rickets and osteomalacia
i. Sepsis
B. Diagnosis
1. Symptoms and signs are aggravated by hyperventilation or other causes of alkalosis.
a. Tetany is the most prominent symptom of hypocalcemia and is manifested by paresthesias (especially numbness and tingling of the face, hands, and feet), muscle cramps, laryngospasms, or seizures. Other problems include diarrhea, headache, lethargy, irritability, and loss of recent memory. Chronic hypocalcemia may be well tolerated, however, with few symptoms.
b. Dry skin, abnormal nails, cataracts, and papilledema may develop in long-standing cases.
c. Chvostek sign: twitching of muscles around the mouth, nose, or eyes after tapping the facial nerve.
d. Trousseau sign: spasm of the hand during 3 to 4 minutes of exercise while a blood pressure cuff on the arm is inflated midway between systolic and diastolic pressures.
2. Laboratory studies. Serum levels of calcium, phosphorus, magnesium, electrolytes, BUN, creatinine, albumin, intact PTH, and 25-hydroxy-vitamin D should be obtained. The ECG may show a prolonged QT interval; the ECG is monitored during therapy.
3. Differential diagnosis of hypocalcemia
a. Severe alkalosis resulting from prolonged nasogastric suction, vomiting, or hyperventilation
b. Severe muscle cramps resulting from vincristine or procarbazine therapy
C. Management
1. Severe, acute, symptomatic hypocalcemia (blood calcium ≤6 mg/dL) is generally managed in an intensive care setting with ECG monitoring.
a. Calcium gluconate or calcium chloride, 1 g, diluted in 50 mL of either D5W or normal saline, is given every 15 to 20 minutes as long as tetany persists.
b. Magnesium sulfate, 1 g IV or IM every 8 to 12 hours, is also administered if the blood magnesium level is unknown or <1.5 mg/dL until the calcium or magnesium blood levels have normalized.
c. Hyperventilating patients should breathe into a paper bag to decrease respiratory alkalosis.
d. Serum calcium levels are obtained every 1 to 2 hours until the serum calcium level exceeds 7 mg/dL.
2. Moderate hypocalcemia (blood calcium between 7 and 8 mg/dL)
a. Calcium may be given either PO or, if the patient is severely symptomatic, IV.
(1) Calcium carbonate, 2.5 g/d, or calcium citrate, 4 to 5 g/d PO; either form will provide about 1,000 mg of elemental calcium daily.
(2) Calcium gluconate, 2 g IV in 500 mL of 5% dextrose in water, is given every 8 hours.
b. Hypomagnesemia (<1.5 mg/dL) is treated with magnesium sulfate, 1 g IM or IV once or twice daily, until the blood level is normal.
c. Patients recovering from hypercalcemia who were treated with IV bisphosphonates or mithramycin are in jeopardy of recurrent life-threatening hypocalcemia for as long as 4 days after treatment is stopped.
d. Patients with postthyroidectomy hypoparathyroidism are discussed in Chapter 15, Section III.F.1.a.
III. HYPERPHOSPHATEMIA
A. Mechanisms. Hyperphosphatemia (>4.5 mg/dL) is a rare complication of treatment of certain tumors, notably leukemia and lymphoma (especially Burkitt lymphoma). Rapid tumor lysis releases large amounts of potassium, phosphate, and nucleic acids (which are metabolized to uric acid). Elevated blood phosphate levels may not be observed until 2 days after beginning tumor therapy; elevations may persist for 4 to 5 days and can exceed 20 mg/dL.
B. Diagnosis. The serum phosphate level itself does not cause symptoms. Renal damage or acute renal failure results from precipitation of calcium phosphate in the kidneys. Tetany and seizures may develop if the ionized calcium concentration becomes inordinately reduced (e.g., with alkalosis from bicarbonate administration or vomiting).
1. Laboratory studies. Serum phosphate, calcium, and other electrolyte levels should be measured regularly in susceptible patients during the initial course of antitumor therapy.
2. Differential diagnosis
a. Hypoparathyroidism
b. Renal failure
c. Rapid tissue breakdown after muscle trauma or burn
d. Tumor lysis syndrome (see Section XIII)
e. Large oral or rectal doses of phosphates
C. Management. High phosphate levels must be lowered rapidly to avoid or reverse renal damage. Serum chemistries are monitored every 4 to 6 hours. The following methods are used simultaneously until the phosphate concentration reaches 5 mg/dL:
1. An IV infusion of 20% dextrose containing 10 U/L of regular insulin is administered at a rate of 50 to 100 mL/h until the blood phosphate level falls below 7 mg/dL. When insulin drives glucose into cells, it moves phosphorus along with it; as soon as glucose enters a cell, it is phosphorylated to glucose-6-phosphate. The extracellular volume is expanded by infusing half-normal saline at 100 to 200 mL/h. Potassium is added to the solution if the serum level is <4 mEq/L.
2. Oral phosphate binders are given to bind phosphate in the intestine.






