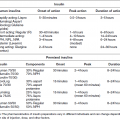
Chapter 3 Lewis W. Johnson, MD and Ruth S. Weinstock, MD, PhD Medical complications of diabetes are largely responsible for the increased morbidity, premature mortality, and economic burden associated with the disease. The total estimated cost of diabetes in the United States in 2012 was $245 billion, 43% of which was for hospital inpatient care and 18% of which was for prescription medications to treat the complications of diabetes [1]. There were $176 billion in direct medical costs and $69 billion in reduced productivity [1]. Acute serious medical complications can be immediately life-threatening and include diabetic ketoacidosis (DKA), the hyperglycemic hyperosmolar state (HHS), severe hypoglycemia, and acute infections. These are important to recognize and treat promptly because they can be fatal if left untreated [2–4]. Chronic complications are primarily classified as microvascular (retinopathy, nephropathy, and neuropathy) or macrovascular (coronary heart disease, cerebrovascular disease, and peripheral arterial disease). Additional medical conditions are also more frequently seen in people with type 1 and/or type 2 diabetes and are described below. Recommendations for the evaluation, management, and prevention of complications in people with diabetes are discussed in this chapter. DKA most frequently occurs in type 1 diabetes but occasionally develops in individuals with type 2 diabetes. It may be the first presentation of type 1 diabetes. In type 1 diabetes, DKA can be precipitated by omission of insulin or by any major stress such as infection or myocardial infarction. Because myocardial infarction can be silent, an electrocardiogram is indicated in all adults with DKA. Nausea, vomiting, abdominal pain, increased urination, and increased thirst are common presenting symptoms. The person may have a rapid respiratory rate and the fruity odor of ketones on the breath. Osmotic diuresis promotes loss of multiple minerals and electrolytes, including sodium, potassium, phosphate, calcium, magnesium, and chloride, all of which need to be replaced. A timely diagnosis is crucial because if untreated, DKA can progress to coma and death. Immediate hospitalization and treatment with insulin and intravenous hydration with electrolyte replacement are required. Most important in prevention of DKA is that the patient be appropriately educated in sick day care including continuing insulin therapy, intensifying glucose monitoring, checking urine or blood for ketones, and prompt consultation with his or her health care team whenever he or she has persistent hyperglycemia, ketonuria, or ketonemia. HHS most commonly occurs in older individuals with type 2 diabetes. There is almost always a precipitating event such as infection, myocardial infarction, or stroke. The patient usually presents with a history of polyuria, weight loss, and diminished oral intake that may result in mental confusion, lethargy, or coma. Abnormal thirst sensation or limited access to fluids facilitates the development of this syndrome. In contrast to DKA, the insulin deficiency is less severe and marked ketosis or severe acidosis is absent (Table 3.1). The plasma glucose is frequently greater than 1,000 mg/dl and the individual is severely dehydrated. As with DKA, hospitalization and intensive hydration are required. The precipitating event should be determined and treated as soon as possible. Even with proper treatment the mortality is high. Table 3.1 Hyperglycemic emergencies. Features of diabetic ketoacidosis (DKA) and the hyperglycemic hyperosmolar state (HHS). Hypoglycemia, the most common acute complication in diabetes, is discussed in Chapter 4. There is increased frequency and severity of bacterial and fungal infections with diabetes. Predisposing factors are hyperglycemic-related impairment of the immune response, vascular insufficiency, peripheral neuropathy, autonomic neuropathy, urinary dysmotility, and skin and mucosal colonization with pathogens such as Staphylococcus aureus and Candida species. Vaccine efficiency is adequate in most patients but those with type 1 diabetes and high HbA1c levels are most likely to exhibit hypo-responsiveness [5, 6]. Acute deterioration of glycemic control should trigger evaluation for possible infection. Diabetes and hyperglycemia are strong independent risk factors for hospitalization as a result of pneumonia, urinary tract infection, and skin infection [7]. The most frequent respiratory infections associated with diabetes are due to Streptococcus pneumoniae (pneumococcal pneumonia) and the influenza virus. People with diabetes are six times more likely to need hospitalization during influenza epidemics and develop serious complications [6]. Patients with diabetes have a high incidence of nasal carriage of Staphylococcus aureus. To reduce hospitalizations, death, and medical expenses, influenza and pneumococcal vaccination are recommended for all patients with diabetes [2]. Patients with diabetes are at higher risk of contracting tuberculosis than individuals without diabetes. Routine screening of patients with tuberculosis for diabetes and patients with diabetes for tuberculosis are also recommended [5, 8]. Although women with diabetes have greater prevalence of asymptomatic bacteriuria, the routine use of antibiotic therapy remains controversial [5]. Urinary tract infections are more prevalent and can evolve into more serious conditions. Acute pyelonephritis is four to five times more common in individuals with diabetes, and is more frequently bilateral. Additionally, people with diabetes are at increased risk for complications such as perinephric and/or renal abscesses. More than 90% of cases of emphysematous pyelonephritis occur in patients with diabetes. This entity can be diagnosed with a plain film of the abdomen and has a high mortality. Failure of fever to resolve after three to four days of treatment of a urinary tract infection in a patient with diabetes should arouse suspicion about the possibility of this uncommon complication. In addition to intravenous antibiotics, surgical drainage is usually required [9]. Mucosal colonization with Candida albicans is also common in people with diabetes who are overweight or are taking antibiotics. These infections can cause extreme discomfort and result in breakdown of the skin, which allows entry of more virulent organisms. Good glycemic control and local antifungal treatment usually resolve the problem. Women with diabetes who have poor glycemic control are prone to vulvovaginal candidiasis [4]. Patients with diabetes may develop yeast infections in the gastrointestinal (GI) tract, especially when glycemic control is poor. The most common agent is Candida albicans. Yeast infection in the mouth (thrush) is characterized by a thick white coating of the tongue and throat. If the infection extends further, esophagitis results, which may cause intestinal bleeding, pain, and difficulty swallowing. Oral Candida can be diagnosed by physical examination, but esophagitis usually requires endoscopy. Treatment is with topical and/or systemic antifungal medication. Emphysematous cholecystitis may be clinically similar to acute cholecystitis, but the proportion of males is higher, gangrene of the gallbladder and perforation are more frequent, and the overall mortality is higher. The diagnosis is established by radiographic demonstration of gas on X-ray or by abdominal computed tomography (CT). Emergency cholecystectomy, in addition to broad-spectrum antibiotics, is necessary [9, 10]. Patients with hepatitis C (HCV) are three times more likely to develop diabetes than individuals who are HCV negative. Patients with HCV who develop type 2 diabetes have more severe liver disease and increased fibrosis compared to those who do not have diabetes [5, 11]. Hepatitis B virus (HBV) infections have been reported among patients who shared blood glucose meters [12]. Acute HBV infection is twice as high among adults with diabetes. In 2012 the Centers for Disease Control and Prevention recommended HBV vaccination to adults with diabetes under 60 years of age [13]. The two most serious head and neck infections are invasive external otitis and rhinocerebral mucormycosis. Dental infections will be discussed in Chapters 6 and 8. Invasive external otitis is an uncommon infection of the ear canal that can extend to the skull and adjacent regions. It often affects the elderly, and the etiologic agent is usually Pseudomonas aeruginosa. The patient has severe pain, discharge from the ear canal, and hearing loss. Skull base osteomyelitis and cranial nerve involvement may occur. The best diagnostic method is magnetic resonance imaging. Treatment includes repeated debridement and antibiotic therapy [5, 10]. Rhinocerebral mucormycosis is a rare fungal infection of the nasal sinuses and brain. Approximately 50% of cases have diabetes. Ketoacidosis is the most important risk factor. Early manifestations include facial or ocular pain and nasal stuffiness. Diagnosis is established by biopsy and culture of necrotic tissue from the nasal passages or the palate. Surgical debridement of infected tissue and drainage of infected sinuses are key elements in achieving a cure. Control of diabetes and institution of amphotericin B are crucial [5, 10]. Furunculosis and subcutaneous abscesses are more common in diabetes and are usually due to staphylococcus infection. Treatment includes application of warm compresses and may require drainage and administration of antibiotics. Foot infections are the most common soft tissue infections in people with diabetes. All people with diabetes should be educated about proper foot care, inspect their feet daily, and seek medical attention immediately with signs of infection. Potential complications include osteomyelitis, which may result in amputation. The most common organisms are staphylococci, although they are frequently polymicrobial infections. Methacillin-resistant Staphylococcus aureus (MRSA) has begun to be increasingly important. Outpatient management of infected foot ulcers begins with surgical removal of the necrotic tissue and administration of antibiotics [5]. A multidisciplinary approach to treatment including surgical or podiatric consultation is recommended. Necrotizing fasciitis is a life threatening infection that starts in the subcutaneous space and spreads along fascial planes. The most common locations are the arms, legs, and abdominal wall. The degree of pain is disproportionate to the findings on physical examination. Marked signs of systemic toxicity are usually present. In diabetes, fasciitis is typically polymicrobial. The associated mortality is approximately 40%. Prompt, aggressive surgical debridement is crucial in decreasing mortality [10]. An association between diabetes and an increased risk of surgical site infections has been well established. Postoperative hyperglycemia is significantly associated with the development of surgical site infections [14]. One of the most devastating complications of cardiac surgery in patients with diabetes is deep sternal wound infection. The incidence of this complication is decreased by keeping the postoperative blood glucose below 200 mg/dl [15–17]. There is an increased risk of developing type 2 diabetes in people with human immunodeficiency virus (HIV). The increased risk of diabetes is related to the HIV itself or its treatment. Insulin resistance is the main mechanism implicated in the pathogenesis of diabetes in HIV patients; protease inhibitors also cause insulin resistance [5]. Patients with HIV should be screened for diabetes at diagnosis and during drug therapy. Chronic complications are responsible for most of the long-term morbidity and mortality associated with diabetes mellitus. The risk of developing both microvascular and macrovascular complications has been shown to be closely associated with the degree and duration of hyperglycemia. As the HbA1c increases from 5.5% to 9.5% there is a 10-fold increase in microvascular disease and about a two-fold increase in macrovascular disease. Reduction in chronic hyperglycemia prevents or delays the progression of retinopathy, nephropathy, and neuropathy but the evidence for this effect is less clear for macrovascular disease [18–22]. Other factors including hypertension, dyslipidemia, and cigarette smoking play major roles in the development and treatment of macrovascular complications. An emerging theory is that hyperglycemia leads to epigenetic changes and damage to the microvasculature of the retina, kidney, and nervous system. Specific cell types such as the capillary endothelial cells in the retina, mesangial cells in the renal glomerulus, and the vasa vasorum of peripheral nerves are prone to develop the tissue-damaging changes associated with hyperglycemia because they cannot limit the entry of glucose. Other cells, such as smooth-muscle cells, when exposed to hyperglycemia reduce glucose transport so that their internal glucose concentration remains constant. There are at least five pathways that may explain how hyperglycemia causes the chronic complications of diabetes [23]: The mechanisms underlying macrovascular disease are less clear but are associated with insulin resistance and elevated levels of circulating free fatty acids as well as hyperglycemia. Approximately 85% of people with type 2 diabetes have the metabolic syndrome which, in addition to insulin resistance, includes abdominal obesity, hypertension, and an atherogenic dyslipidemia, all of which are independent accelerating factors in the development of chronic complications. Genetic factors are also involved in the development of chronic diabetes-related complications. The Joslin 50–Year Medalist Study enrolled individuals who have had type 1 diabetes for more than fifty years without developing any significant complications. These patients are being actively evaluated in an attempt to identify possible reasons for this protection [24]. For each complication the following will be discussed: (1) the importance of the complication, (2) screening recommendations, (3) treatment goals, and (4) means of prevention (Table 3.2). Table 3.2 Chronic microvascular complications of diabetes mellitus. Screening recommendations. aGFR: Glomerular filtration rate (ml/min/1.73 m2). In the United States, diabetes is the leading cause of blindness in people between 20 and 74 years of age. There is a higher risk of retinopathy in type 1 diabetes but because type 2 is more common it accounts for more individuals with visual loss. Diabetic retinopathy is associated with progressive changes in the retinal microvasculature leading to areas of nonperfusion, increased vascular permeability, and the proliferation of new pathologic vessels. Diabetic eye disease is classified as nonproliferative retinopathy (NPDR), proliferative retinopathy (PDR), and macular edema. NPDR is usually asymptomatic and marked by microaneurysms, blot hemorrhages, and exudates. It is present in many if not most individuals who have had diabetes for more than 20 years, particularly if their glycemic control has been suboptimal. NPDR can be progressive and lead to retinal ischemia which is a potent inducer of angiogenic growth factors such as vascular endothelial growth factor (VEGF). PDR is characterized by neovascularization leading to vitreous hemorrhage, fibrosis, and retinal detachment. Other eye diseases including cataracts and glaucoma occur earlier and more commonly in people with diabetes. In poorly controlled diabetes, high blood glucose levels can cause osmotic lens swelling resulting in blurred vision. Corrective lenses should not be prescribed until the glycemic control has improved. Routine non-dilated retinal examinations performed by a primary care provider or diabetes specialist may not detect retinopathy and are therefore inadequate. Guidelines [2] recommend that adults and children with type 1 diabetes have a dilated eye examination by an ophthalmologist or optometrist within five years of the onset of diabetes. People with type 2 diabetes should have a dilated exam shortly after diagnosis because the duration of their disease is unknown. In the United Kingdom Prospective Diabetes Study (UKPDS) of type 2 diabetes, 35% of females and 39% of males had diabetic retinopathy at the time diabetes was diagnosed [25]. Patients with both type 1 and type 2 diabetes generally should have lifelong annual comprehensive eye exams by a qualified eye specialist. If retinopathy is present, close follow-up by an ophthalmologist experienced in the management of diabetic retinopathy is indicated. Pregnancy can cause retinopathy to progress rapidly [26]. Women with known diabetes who are planning pregnancy should have a dilated eye exam before conception and then be followed closely by an ophthalmologist during pregnancy and for one year after delivery. Gestational diabetes does not place the mother at increased risk for developing retinopathy. Serious retinopathy, if detected early, can be successfully treated with laser therapy [27, 28]. Newer therapies, including intraocular injection of a monoclonal antibody to VEGF and glucocorticoids, may halt the progression of neovascularization and macular edema, improve vision, and reduce the need for laser therapy in some patients [29]. Factors that favor the development and progression of diabetic retinopathy are duration of diabetes, poor glycemic control, nephropathy, and hypertension. To reduce the risk of developing or to slow the progression of retinopathy, glycemic and blood pressure control should be optimized [18, 19, 21, 22, 30]. The presence of retinopathy is not a contraindication to the use of aspirin for cardioprotection when indicated. Diabetic nephropathy occurs in 20–40% of people with diabetes and is the leading cause of end-stage renal disease (ESRD) in the United States. Nephropathy appears to be more common in type 1 diabetes, but because of the increasing number people with type 2 diabetes, more than 80% of people in renal replacement programs have type 2 diabetes. People with diabetic nephropathy commonly also have retinopathy. Like other microvascular complications, the pathogenesis of diabetic nephropathy is related to chronic hyperglycemia, but hypertension plays a major role in its development and progression. The classic progression of diabetic nephropathy begins with microalbuminuria (30–299 mg/gm creatinine), then macroalbuminuria (equal to or greater than 300 mg/gm creatinine), followed by a decrease in the glomerular filtration rate (GFR). Microalbuminuria is a marker not only for the development of nephropathy, but also for increased cardiovascular risk [31]. Screening recommendations are to perform an annual urine albumin: creatinine ratio in type 1 diabetes of equal to or greater than five year’s duration and in all type 2 patients starting at diagnosis [2]. In all adults with diabetes, the serum creatinine should be measured at least annually to calculate the GFR. The National Kidney Foundation classifies chronic kidney disease based on the calculated GFR (ml/min/1.73 m2): Renal dysfunction can occur in the absence of albuminuria, particularly in individuals with type 2 diabetes and hypertension. Nephrology consultation should be considered if the etiology of renal disease is uncertain (e.g., proteinuria in the absence of retinopathy) and for worsening renal function. Glycemic and blood pressure control are the cornerstones for preventing and treating diabetic nephropathy. The importance of better glycemic control for forestalling or preventing nephropathy in type 1 diabetes was shown in the Diabetes Control and Complications Trial (DCCT) and its follow-up epidemiologic study (DCCT/EDIC) [19, 32]. The UKPDS and its 10-year follow-up showed similar results in type 2 diabetes [21, 22]. The more recent Action in Diabetes and Vascular disease: PreterAx and DiamicroN Modified Release Controlled Evaluation (ADVANCE) trial demonstrated that greater improvement in the HbA1c (to 6.5%) in type 2 diabetes was associated with further reduction in renal events [33]. Blood pressure control appears to be the most important single intervention to prevent progressive nephropathy in both type 1 and type 2 diabetes. For example, in the UKPDS, a reduction in systolic blood pressure from 154 to 144 mmHg was associated with a 30% reduction in microalbuminuria [30]. Although guidelines suggest specific targets for blood pressure, there does not appear to be any threshold for renal protection. Agents that interrupt the renin-angiotensin system such as angiotensin converting enzyme inhibitors (ACEI) and angiotensin receptor blockers (ARBs) provide a benefit over other antihypertensive agents and are recommended if microalbuminuria is documented. Most patients require two or more drugs for blood pressure control. The role of lipid-lowering agents to prevent nephropathy is less clear but most individuals with diabetic nephropathy take a statin to prevent cardiovascular disease events. To date there is no evidence to suggest that statins reduce cardiovascular events in individuals who are on dialysis [34]. Fibrates are prescribed primarily to lower triglyceride levels in patients with hypertriglyceridemia. In a study of the effect of fenofibrate therapy on cardiovascular events in type 2 diabetes there was less albuminuria progression and less retinopathy needing laser treatment in the fenofibrate group [35]. Renal function can be worsened by the use of many drugs including over-the-counter nonsteroidal anti-inflammatory agents. Many medications require dose adjustments in the presence of renal dysfunction. Radiographic contrast agents can worsen renal function. Risk factors for contrast-induced nephrotoxicity are underlying renal disease and dehydration. It is recommended that metformin be discontinued before any procedure using contrast agents to prevent life threatening lactic acidosis and that the drug be resumed only when it has been ascertained that the creatinine has returned to baseline. Smoking can hasten the progression of renal dysfunction and cessation needs to be stressed.
Medical complications of diabetes mellitus
Introduction
Acute complications
Diabetic ketoacidosis
Hyperglycemic hyperosmolar state
DKA
HHS
Age
<40 years
>60 years
Duration of symptoms
<2 days
>5 days
Plasma glucose
250–600 mg/dL
>600 mg/dL
Serum sodium
125–135 meq/L (normal to ↓)
>135 meq/L (normal to ↑)
Serum potassium
Normal to ↑
Normal
Serum bicarbonate
<15 meq/L
>15 meq/L
Ketones (urine or blood)
Strongly elevated
Elevated or absent
Arterial pH
6.8–7.3
>7.3
Arterial pCO2
20–30 mm Hg
Normal
Serum osmolality
300–320 mOsm/ml
>330 mOsm/ml
Mortality
3–5%
10–20%
Hypoglycemia
Infections
Respiratory infections
Genitourinary infections
Gastrointestinal and liver infections
Head and neck infections
Skin and soft tissue infections
Surgical site infections
Human immunodeficiency virus
Chronic complications
Mechanisms of development of chronic complications
Microvascular complications
Complication
Screening Recommendations
Eye disease
Retinopathy
Macular edema
Glaucoma
Cataracts
Annual dilated eye exam (If excellent glycemic control and no retinopathy, this can be every two years)
Nephropathy
Albuminuria
Decreased GFR
End-stage renal disease
Annual spot urine for albumin/creatinine ratio
Annual serum creatinine and calculation of GFRa
Neuropathy
Distal symmetric polyneuropathy
Autonomic neuropathy
Annual exam for loss of protective sensation
Careful history at each office visit
Retinopathy
Nephropathy
Neuropathy
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree