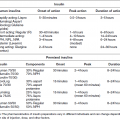
Chapter 5 Brian L. Mealey, DDS, MS Due to the high prevalence of diabetes mellitus in the population, it is common for people with diabetes, both diagnosed and undiagnosed, to seek care in the dental office. Patients with diabetes may require precautions before, during, and after dental treatment. Proper management of these patients in the dental office requires a thorough understanding of current diagnosis and medical treatment of diabetes. Laboratory tests used in the diagnosis and management of diabetes are discussed in Chapter 2, while Chapter 4 contains a thorough review of currently available medications used in diabetes. The purpose of this chapter is to provide clinical pathways of care for use in the dental office. Many studies reviewed in other chapters in this text have examined the impact of diabetes on periodontal health and the potential impact of periodontal therapy on metabolic control of diabetes. However, there is much less research examining the outcomes of periodontal therapy in periodontitis patients with diabetes compared to those without diabetes. In many of the studies of the effects of periodontal therapy in patients with diabetes, the average changes in probing depth and attachment level seen following scaling and root planing are similar in magnitude to studies of scaling and root planing performed in people without diabetes. However, these are not controlled trials of periodontal treatment in individuals with and without diabetes and therefore provide only low-level evidence that patients with diabetes as a group respond well to periodontal therapy. In a comparison of periodontitis patients without diabetes and those with well-controlled diabetes, the short-term clinical and microbiologic responses to scaling and root planing were similar three to four months after treatment [1, 2]. Whereas many patients with diabetes and chronic periodontitis show improvement in clinical periodontal parameters after scaling and root planing, patients with poor glycemic control may have a more rapid recurrence of deep pockets and a less favorable long-term response. In a study of patients with type 1 diabetes, four weeks after scaling and root planing, those with good glycemic control had similar reductions in probing depth, clinical attachment level, and bleeding on probing as patients without diabetes, and the improved parameters remained stable for 12 months. Conversely, those with poorly controlled diabetes showed initial improvement at four weeks but then had a greater recurrence of deep probing depths at 12 months than those with well-controlled diabetes or no diabetes [3]. Therefore, the short-term benefits of periodontal therapy may not be sustained in people with poorly controlled diabetes. There are few long-term studies of periodontal therapy in patients with diabetes. In one small longitudinal study, 20 people with diabetes (types 1 and 2) and 20 without diabetes received scaling and root planing, modified Widman flap surgery at sites with residual probing depths greater than 5 mm, and regular periodontal maintenance therapy [4]. Five years after the baseline examination, both groups of subjects had a similar percentage of sites demonstrating gain, loss, or no change in clinical attachment. Most of the patients with diabetes in this study were well controlled or moderately controlled at baseline, so the study does not address those with poor glycemic control. However, it does suggest that people with relatively well controlled diabetes have a positive response to periodontal treatment that can be sustained over extended periods of time as long as regular periodontal maintenance is performed. Progression of periodontitis and incident tooth loss were examined in 23 subjects with poorly controlled type 2 diabetes (mean glycated hemoglobin [HbA1c] = 9.1%), 23 with well-controlled type 2 diabetes (mean HbA1c = 6.1%) and 46 without diabetes [5]. Subjects were recalled for periodontal maintenance every four to six months following active periodontal treatment, which consisted of nonsurgical therapy with or without subsequent periodontal surgery. While there were no differences in clinical parameters between groups before treatment, at the five-year examination the subjects with poorly controlled diabetes had a higher mean probing depth, clinical attachment loss, bleeding on probing, and number of teeth lost compared to those with well-controlled diabetes or without diabetes. There were no differences between those with well-controlled diabetes and those without diabetes. Progression of periodontitis was defined as an increase of 3 mm or more in clinical attachment loss at two or more interproximal sites between study visits. After five years, the number of subjects with periodontitis progression was significantly greater in the poorly controlled diabetes group (39.2% of subjects) compared to either the well-controlled diabetes group (21.7% of subjects) or the group without diabetes (23.9% of subjects). Likewise, the percentage of sites with progressive attachment loss was significantly greater in poorly controlled diabetes (6.1% of sites) compared to either well-controlled diabetes (2.5% of sites) or no diabetes (2.8% of sites). Thus, the overall response to periodontal therapy may be less favorable in individuals with poorly controlled diabetes, whereas those with well-controlled diabetes appear to respond to periodontal therapy in a manner similar to patients without diabetes. The studies mentioned above generally involve a small number of subjects and study results are based on means of subject groups. Because not all patients in clinical practice reflect the mean and standard deviation in clinical studies, clinicians are advised to evaluate each subject individually with an understanding that each patient may or may not have responses to therapy similar to the “mean subject” in any given study. Further longitudinal studies of various periodontal treatment modalities in larger subject populations are clearly needed to determine the periodontal healing response in individuals with diabetes compared to individuals without diabetes and to assess the impact of glycemic control on the results of treatment. Diabetes affects bone metabolism via multiple different mechanisms that may impair bone healing and normal homeostatic bone turnover [6]. Elevated glucose levels may inhibit differentiation and proliferation of osteoblasts, with resulting decreased formation of bone matrix [6, 7]. Both type 1 and type 2 diabetes have been associated with increased risk of hip fracture, but HbA1c was not correlated with the rate of fractures [8]. Animal studies have shown that osseointegration is impaired in animals with chemically induced diabetes compared to animals without diabetes [9, 10]. However, human research on the impact of diabetes on dental implant failure or complications is equivocal. Some studies show that diabetes increases the risk of implant failure by two-fold to three-fold compared to patients without diabetes [11], while others show no difference in failure rates associated with diabetes [12–14]. Reviews of the overall body of evidence suggest that implant failures in patient with diabetes tend to occur early after placement; furthermore, the percentage of patients with diabetes who experience implant failures appears to be relatively high but the percentage of implants that fail is similar to that of patients without diabetes [15]. The impact of glycemic control on implant failures in people with diabetes is unclear. Most studies of implant therapy in diabetes fail to evaluate the level of glycemic control among the patients. The few studies that have gathered adequate HbA1c data on the patients with diabetes all had a small number of study subjects and included only subjects with type 2 diabetes [16–19]. Most of the studies report implant failure rates only in the short-term post-placement period [16, 18, 19]. There is little evidence from these studies that elevated HbA1c levels adversely affect short-term failure rates of dental implants, with the exception of patients with very poor glycemic control (HbA1c greater than 9%) [17]. Clinicians must recognize, however, that the evidence base is incomplete. Until further research is performed clinicians should proceed cautiously with implant therapy in diabetic patients having only moderate or poor levels of glycemic control. Further research on long-term implant outcomes in type 1 and type 2 diabetes is clearly needed. The U.S. Centers for Disease Control estimated in 2011 that approximately 25.8 million American have diabetes and that about 7 million of those individuals are undiagnosed [20]. Patients with undiagnosed diabetes are a major target population for the dental office, because signs and symptoms of diabetes may present initially in the oral cavity (chapters 6 and 8). Dentists and dental hygienists may be the first to recognize signs and symptoms such as advanced periodontal diseases or other infections, burning mouth, xerostomia, or parotid enlargement. The medical history must be reviewed thoroughly to determine if the patient has been previously diagnosed with diabetes or if the patient has risk factors for diabetes such as prediabetes, overweight/obesity, racial risk factors, family history of diabetes, history of gestational diabetes, or others discussed in Chapter 2. Diabetes is associated with an increased prevalence and severity of gingivitis and periodontitis, with the greatest risk in individuals with poor glycemic control [6, 21, 22]. Poor glycemic control also increases the risk of periodontal disease progression over time [23]. Signs and symptoms of undiagnosed diabetes may also be present in individuals with diagnosed diabetes in whom glycemic control is poor. These findings should initiate a clinical pathway of care directed toward medical evaluation of the patient’s diabetes condition. Interaction between the dentist and physician is a critical component of care. During the initial oral evaluation, the dentist should assess the periodontium for signs of potential undiagnosed or poorly controlled diabetes such as extensive gingival bleeding, presence of multiple simultaneously occurring periodontal abscesses, localized or generalized gingival swelling that may be accompanied by tissue that appears to proliferate out of the periodontal pocket, rapid progression of bone loss and attachment loss that is inconsistent with the level of plaque and calculus, or a poor wound healing response after periodontal therapy (chapters 6 and 8). If such signs are present, the dentist should thoroughly review the medical history again. This is a critical step that is often overlooked in the dental office. If the patient does not currently have a diagnosis of diabetes, the dentist needs to ask appropriate questions directed at those conditions commonly associated with undiagnosed diabetes [24] (Figure 5.1). It is best if these questions are part of the written medical history; if not, they should be asked verbally. It is important to first ask the patient directly, “Have you ever been diagnosed with diabetes?” If not, the dentist should ask whether the patient has any first degree relatives with diabetes; this includes the father, mother, sisters, or brothers. If the patient has first degree relatives with diabetes, there is an increased risk that the patient has diabetes. If the patient is female, the dentist should ask if she has ever been pregnant and, if so, whether or not she had gestational diabetes during any of her pregnancies. Also ask if the patient ever had a baby weighing more than 9 lbs. at birth. A positive history of gestational diabetes or birth of a child over 9 lbs. increases the risk of the patient developing type 2 diabetes later in life [21, 24]. In addition to questioning the patient for risk factors, the dentist should evaluate the patient’s race and body morphotype. Ethnic groups with higher risk for diabetes include African American, Latino, Native American, Asian American, and Pacific Islander [24]. Increased body mass index (BMI) is clearly associated with risk for type 2 diabetes [24]. Figure 5.1 Clinical pathway of care: Patient without a diagnosis of diabetes (initial assessment). It is important to remember that “increased risk” does not necessarily mean “presence of disease”; that is, just because a given patient has one or more risk factors for diabetes does not mean that this given patient actually has diabetes. However, the dentist and dental hygienist play a major role in assessing risk factors for diabetes, because many individuals visit the dentist’s office more frequently than they do the physician’s office. In the presence of intraoral signs and symptoms of possible undiagnosed diabetes, patients with one or more risk factors for diabetes should receive further evaluation. Following the review of the medical history and assessment of the patient’s physical features and race, the dentist should ask the patient about a history of polyuria (frequent urination), polydipsia (excessive sense of thirst) and polyphagia (excessive sense of hunger or inability to remain satiated after a meal), recent vision changes, or rapid weight loss (Figure 5.1). These are common signs and symptoms of undiagnosed diabetes. If the patient reports no such signs or symptoms, the dentist should look for other potential underlying medical conditions that might be associated with the oral findings noted in that patient; however, the dentist cannot rule out diabetes simply because these signs and symptoms are not present. Consultation with the patient’s physician may be indicated. Communication between dentist and physician offices is frequently poor, and patients may suffer due to the inability of dentists and physicians to communicate fully. A study of general dentists and periodontists demonstrated that 77% of periodontists and 44% of generalists always ask patients with diabetes what type of diabetes they have, and about 80% of periodontists and 56% of generalists ask about the patient’s medical management regimen or level of glycemic control [25]. However, only 35% of periodontists and 14% of general dentists consistently communicate with the diabetic patient’s physicians, and only 28% of periodontists and 14% of generalists objectively evaluate glycemic control by consulting the physician about laboratory test values such as the glycated hemoglobin (HbA1c) test, which is the gold standard for assessing the quality of glycemic control. It is important that the medical consultation sent by the dentist be clear, informative, and precise. The consultation should provide the patient’s age, gender, and race; a brief but clear description of the oral findings; and the specific signs and symptoms of possible diabetes noted for that patient (Figure 5.1). The dentist should then ask specifically what he or she wants the physician to do. For example, a consultation might say, “Mr. Smith is a patient of record in your office. He is a 57-year old African American male with a severe infection of the gum and bone tissues around his teeth (periodontitis) that is not consistent with the usual findings for such conditions. He reports a positive history of polyuria and polydipsia. He is significantly overweight. Mr. Smith reports that his mother and brother have type 2 diabetes. Please evaluate the patient for possible diabetes. I appreciate your evaluation of Mr. Smith and request that the results of your examination be sent to my office fax at 123-456-7890.” Such a consult does several things. First, it demonstrates for the physician that the dentist has evaluated the patient for risk factors such as race, body morphotype, and presence of known signs and symptoms of diabetes. Second, it provides to the physician the information about the patient’s oral health that initiated the dentist’s suspicion of undiagnosed diabetes in the first place. Finally, it makes a specific request of the physician to evaluate the patient for diabetes and to provide the results of that evaluation back to the dental office. This consultation generally leads to ordering and evaluating laboratory tests to determine a diagnosis of diabetes. The following lab values are all suggestive of diabetes: fasting plasma glucose of 126 mg/dl or greater, casual plasma glucose of 200 mg/dl or greater, two-hour postprandial glucose of 200 mg/dl or greater, or HbA1c value of 6.5% or greater [24] (Figure 5.1). These tests are discussed in detail in Chapter 2. If the patient indicates on the medical history that he or she has been previously diagnosed with diabetes, the dentist must first determine which type of diabetes the patient has. Simply ask the patient, “What type of diabetes do you have?” (Figure 5.2). The patient who says, “I have had type 2 diabetes for 12 years, and I take a combination of metformin and sitagliptin every day” understands her disease much better than the patient who replies, “I don’t know; is there more than one type of diabetes?” The purpose of the dentist’s question about the patient’s type of diabetes is designed to preliminarily assess the patient’s own understanding of his or her diabetes. Figure 5.2 Clinical pathway of care: Patient with a previous diagnosis of diabetes (initial assessment). In addition, the clinician should ask the patient to describe the level of glycemic control by asking, “How well is your diabetes controlled?” Often, patients give a reply such as, “Pretty good.” Conversely, a patient might say something like, “My control was good until two years ago when I lost my job, and it hasn’t been very good since then.” The purpose of asking the question is not to obtain an accurate evaluation of glycemic control from the patient. It is as inappropriate to use patient responses to definitively determine the level of glycemic control in patients with diabetes as it would be to use patient responses to accurately determine blood pressure levels in a patient with hypertension. Rather, these questions are used to assess the patient’s knowledge of his own condition before the clinician begins a course of therapy that may require communication with the physician and alterations in the diabetes management plan, or may involve dental treatment with outcomes that depend in part on the patient’s ability to maintain good glycemic control. An accurate determination of glycemic control will follow as part of the treatment planning process (see below). The pathophysiology and medical treatment regimens vary between type 1 and type 2 diabetes, and dental management may differ as well. After determining what type of diabetes the patient has, the clinician must obtain an accurate and detailed understanding of the patient’s medical management regimen. Simply asking the patient, “What medications do you take?” often elicits incomplete or inaccurate answers. The dentist can consult with the patient’s physician about the medication regimens, but this is often made difficult by the presence of multiple physician providers prescribing different medications for a single patient. Instead, the dentist may simply ask the patient to bring all of his or her medications to the next dental appointment, with a reminder being given to the patient the day before the dental visit when confirming the appointment by telephone. Doing this allows the dentist to make a list of all current medications being taken by the patient by directly examining the prescriptions rather than relying on patient memory to provide an accurate medication list. Patients with type 1 diabetes all take insulin by injection or by subcutaneous insulin infusion pump. Individuals with type 2 diabetes may also take insulin but are often managed with oral medications or a combination of oral agents and insulin. Because some diabetes medications are associated with a significant risk for hypoglycemic emergency, it is critical that the dentist determine exactly which medications the patient takes [21, 26]. A detailed discussion of hypoglycemia and its relationship to diabetes medications is below. After initial determination of the type of diabetes and medical management regimen, the dentist performs a thorough oral examination and develops a list of diagnoses. A preliminary treatment plan may also be formulated at this stage. If any acute lesions or conditions are found, they should be treated on an emergent basis (Figure 5.3). For example, if the patient has a periodontal abscess, it should be treated immediately in an appropriate fashion. The clinician should not delay treatment simply because the patient has diabetes. The presence of an acute infection may adversely influence glycemic control and should be treated as soon as it is recognized. The treatment done at this time is limited to managing the acute problem. To treat a periodontal abscess, the clinician may need to provide surgical or nonsurgical debridement of the defect, and systemic antibiotics may be indicated depending on the extent and severity of the infection. For routine dental treatment, there is little indication for routine use of prophylactic antibiotics in patients with diabetes. However, if an infection is present, antibiotics are generally indicated, especially if the patient’s glycemic control is poor. Figure 5.3 Clinical pathway of care: Treatment plan and therapy. Once acute problems have been managed, or if no acute problems exist, the next step in the pathway of care involves accurately determining the patient’s level of glycemic control over an extended period of time (Figure 5.3
Management of the patient with diabetes mellitus in the dental office
Outcomes of periodontal and dental implant therapy in patients with diabetes
Results of periodontal therapy
Results of dental implant therapy
Evaluation and management of patients with diabetes: pathways of care
The patient with undiagnosed diabetes
The patient with a diagnosis of diabetes
Treatment plan and therapy
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree