Maternal Hemostatic Disorders and Obstetric Hemorrhage
Philippe De Moerloose
FranÇOise Boehlen
Jean-Christophe Gris
This chapter reviews conditions associated with disorders of the hemostatic system, which can affect the mother and lead to obstetric hemorrhage, excluding mechanical causes of antepartum hemorrhage (e.g., abnormal placentation, uterine rupture, vasa previa, infections, polyps, or trauma) or postpartum hemorrhage (PPH) (retained placenta, uterine atony, or cervical or vaginal lacerations).1, 2 In the latter situations, coagulation disorders are usually a consequence and not a cause of obstetric hemorrhage.
PLATELET DISORDERS
Thrombocytopenia is the most common hemostatic disorder encountered in pregnancy, and can be considered as isolated and mainly asymptomatic or part of a complex clinical context.
Isolated Platelet Disorders
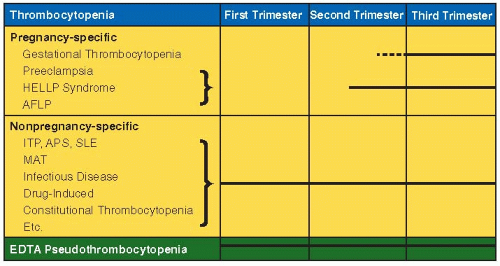
The differential diagnosis of thrombocytopenia discovered during pregnancy is wide and varies with gestational age and is similar to that of nonpregnant women, but some are unique to pregnancy (FIGURE 118.1), 3, 4, 5, 6 notably the “physiologic” decrease of platelet count.7, 8, 9 Thrombocytopenia, defined as platelet count <150 G/L, is a very common and most often an incidental finding during pregnancy, occurring in 5% to 12% of pregnant women,7, 9, 10, 11 but a platelet count <100 G/L is present in only about 1% of pregnant women.10, 12
Incidental Thrombocytopenia
Gestational thrombocytopenia of pregnancy is responsible for 75% to 80% of all pregnancy-associated thrombocytopenias,4, 10, 11, 13 occurring mainly in late pregnancy, in distinction to immune thrombocytopenia (ITP), which is the most common diagnosis during the first trimester of pregnancy. It is important to distinguish incidental thrombocytopenia from ITP, the implication for the pregnancy and the newborn being very different, but it often is not possible to distinguish between these two entities. Incidental thrombocytopenia is a diagnosis of exclusion,14 requiring the following five criteria15, 16:
Asymptomatic, mild thrombocytopenia: typically >70 G/L (most often between 130 and 150 G/L)
Occurrence typically in third trimester
No prior history of thrombocytopenia (except possibly during a previous pregnancy)
No fetal thrombocytopenia
Spontaneous resolution after delivery
According to these criteria, the diagnosis can be confirmed only after birth. Incidental thrombocytopenia being by definition a mild thrombocytopenia, there is no risk for the mother. Indeed a platelet count of more than 70 G/L is usually considered as safe for a locoregional anesthesia and is not associated with an increased hemorrhagic risk during pregnancy and the postpartum period.17, 18 There is no risk for the newborn too since by definition this diagnosis implies that the newborn will have no thrombocytopenia.10, 16, 19, 20
The mechanism of this thrombocytopenia is still uncertain. It could be a physiologic condition due to dilution and/or an increased platelet turnover.21
Immune Thrombocytopenia
ITP is an acquired immune-mediated disorder characterized by isolated thrombocytopenia,22 a platelet count of <100 G/L now considered as the threshold for diagnosis.23 ITP occurs in approximately 1 per 1,000 pregnant women, accounts for 3% to 5% of pregnancy-associated thrombocytopenias,4, 10, 11, 13, 24 and is the most common cause of isolated thrombocytopenia in the first trimester.4, 13 According to the retrospective analysis of Webert et al.,25 most women with ITP have only a mild to moderate decrease of platelet count; 30% to 50% of women with ITP are first diagnosed during pregnancy.25, 26 The diagnosis of ITP is essentially one of exclusion,6, 15, 16, 27, 28 the most difficult distinction being from incidental thrombocytopenia of pregnancy. Search for antiplatelet antibodies has failed to differentiate these two pathologies.12 The two most important points are the monitoring of maternal platelet count during pregnancy and after delivery and control of the newborn’s platelet count at birth and during the 1st days of life. In general, as detailed in the next paragraphs, (a) the evolution of the platelet count during pregnancy is usually unpredictable;28 (b) the risk of maternal hemorrhage depends upon the severity of thrombocytopenia;25 (c) the risk of severe neonatal thrombocytopenia is relatively low;10 (d) there is no way to predict the severity of fetal/neonatal thrombocytopenia;10 and (e) maternal treatment does not influence the newborn’s platelet count.29
Bleeding risk during pregnancy. Women have no bleeding symptoms (65.6%) or only mild or moderate symptoms (respectively 12.9% and 18.1%), and only 3% to 4% of pregnant women have severe symptoms (3.4%).25 The “safe” platelet number allowing spinal or epidural anesthesia (without risk of epidural hematoma) remains controversial, and there are no data to support a minimum required platelet count.30 However, as proposed in international consensus, a platelet count ≥70 to 80 G/L is usually considered as safe.17, 18, 28
Management
Treatment is recommended in case of bleeding symptoms or when the platelet count is below 20 to 30 G/L.15, 31 When the delivery date approaches, it is usually recommended to introduce
treatment to attain a platelet count of >50 G/L to allow good hemostasis during vaginal delivery or cesarean section and to avoid PPH. It is possible that a lower platelet count is acceptable for vaginal delivery without locoregional anesthesia.6, 13, 15, 31, 32 Indeed, in a report of 92 women with ITP (119 pregnancies), the median platelet count at delivery was 85 G/L. In this report, 15% of these women had a platelet count <50 G/L and 6% had a platelet count <20 G/L. Hemorrhagic complications were reported in only four women (nonrequiring red cell transfusions) and were not related to the severity of thrombocytopenia.25
treatment to attain a platelet count of >50 G/L to allow good hemostasis during vaginal delivery or cesarean section and to avoid PPH. It is possible that a lower platelet count is acceptable for vaginal delivery without locoregional anesthesia.6, 13, 15, 31, 32 Indeed, in a report of 92 women with ITP (119 pregnancies), the median platelet count at delivery was 85 G/L. In this report, 15% of these women had a platelet count <50 G/L and 6% had a platelet count <20 G/L. Hemorrhagic complications were reported in only four women (nonrequiring red cell transfusions) and were not related to the severity of thrombocytopenia.25
Treatment options for the management of ITP in pregnancy are usually similar to those proposed in the general population.13 First line therapy is usually based on corticosteroids and/or intravenous immunoglobulins.6, 27, 28, 31 Classically, oral prednisone is initially administered at the dosage of 1 mg/kg/d based on the pregestational weight. This treatment can be associated with side effects for the mother during the gestational period (pregnancy-induced hypertension, gestational diabetes, weight gain, psychosis, etc.) and rarely for the fetus (suppression of the fetal adrenal glands).31 To limit these side effects, prednisone could be started at a lower dose (e.g., 10 to 20 mg/d), and the dose can be progressively increased to obtain a safe platelet count according to the gestational age.27 High doses of immunoglobulins (2 g/kg) may be safer than a high dose of prednisone with a similar efficacy but they need to be administered every 3 to 6 weeks.13, 31, 33 In case of refractoriness, high dose of methylprednisolone could be used.28, 31, 34, 35, 36 Azathioprine may be administered safely during pregnancy, but there are no available studies in the case of ITP.31, 37, 38, 39 Anti-RhD immunoglobulins have been proposed as second line therapy28, 40 but they have to be used with precaution, particularly with a careful monitoring of the neonate although complications are uncommon (neonatal jaundice, anemia, positive direct antiglobulin test after delivery).28, 40 Danazol has been used but only for short-term treatment.41 Other immunosuppressive agents (such as cyclosporine or cyclophosphamide) cannot be used during pregnancy.39 Experience with rituximab during pregnancy is limited and its safety for the fetus is uncertain (category C drug for FDA). It is therefore recommended to avoid rituximab during pregnancy unless the mother’s health is critically dependent upon use of this medication.39, 42, 43, 44 There are no available data on the use of thrombopoietin receptor agonists in pregnancy. Splenectomy can be safely performed during the second trimester.45, 46
If severe thrombocytopenia is diagnosed near delivery, acute treatment with intravenous immunoglobulin 1 g/kg/d for 2 to 3 days combined with methylprednisolone 1 g/d for 3 days will usually result in an increased platelet count within 24 to 48 hours.22, 32 In case of acute obstetric hemorrhage, for example, in a laboring woman, the treatment will differ. Intravenous immunoglobulin and methylprednisolone have to be considered and in addition platelet transfusion should be given.47
Due to the decreased survival of the transfused platelets in the case of ITP, the increase in platelet count will be low. In case of unresponsiveness to this therapy and persistence of hemorrhage, recombinant factor VIIa (rFVIIa) should be considered.48
Risk of Neonatal Thrombocytopenia
Maternal antiplatelet antibodies can cross the placenta and cause fetal/neonatal thrombocytopenia. There is no relation between maternal and fetal/neonatal platelet count, a severe neonatal thrombocytopenia can be observed in the newborn of a mother with a mild thrombocytopenia and newborn from a mother with a severe thrombocytopenia can have a normal platelet count at birth.11, 25, 49, 50, 51 Data about the relation between neonatal thrombocytopenia and the presence or absence of detectable maternal antibodies are controversial.49, 51, 52 So the detection of maternal antibodies has not been proven useful for making predictions about the fetal/neonatal platelet count.12, 16, 53, 54 Corticosteroids given to the mother have no effect on the neonatal platelet count.29, 49, 55 Some data have shown that there is an increased risk of neonatal thrombocytopenia in women with a past history of splenectomy, particularly those who are refractory to splenectomy.55, 56, 57 The best predictor of neonatal thrombocytopenia is a history of thrombocytopenia in a prior sibling.25, 55, 57 Fetal blood sampling by cordocentesis or scalp blood sampling in early labor is not recommended due to the risk of erroneous result and also the risk of fetal distress associated with an invasive procedure.15, 49
Mode of delivery of women with ITP is controversial. Historically, cesarean section was recommended based on a perinatal mortality of 12% to 21% resulting from birth trauma and intracranial hemorrhage (ICH).28, 58 More recent studies suggested that the neonatal mortality is much lower, around <1%.25, 49 Large prospective studies have then confirmed that the incidence of severe neonatal thrombocytopenia (defined as a platelet count <50 G/L) varied from 5% to 20%, and ICH occurring in 0% to 3% of newborn.10, 25, 51, 52, 53, 56, 59, 60 There is no evidence that cesarean section is safer for the thrombocytopenic fetus compared with uncomplicated vaginal delivery (which is usually also safer for the mother).28, 53 Cesarean delivery should be determined essentially by obstetric indications.15, 31, 56
Neonatal platelet count should be determined in cord blood immediately after delivery and followed during the 1st week after birth (nadir being often between day 2 and 5 leading to hemorrhagic complication not directly related to the delivery).6, 25, 28, 31, 49 Indeed, it is important to underline that platelet counts of infants born to mothers with ITP may decrease deeply several days after birth.56, 59 It is therefore crucial to alert the pediatricians.25, 31
Nonisolated Platelet Disorders
Thrombotic Microangiopathies: Thrombotic Thrombocytopenic Purpura—Hemolytic Uremic Syndrome
The term thrombotic microangiopathies (TMAs) encompasses a spectrum of clinical syndromes in which common pathologic feature is the widespread formation of hyaline thrombi in the nonvenous microcirculation, the arterioles, and capillaries. They share thrombocytopenia and Coomb’s negative, microangiopathic hemolytic anemia (MAHA) with the presence of schistocytes on the peripheral blood smear. The emblematic thrombotic thrombocytopenic purpura (TTP) and hemolytic uremic syndrome (HUS) are extremely rare, afflicting 1 in 100,000 pregnancies,61, 62, 63 are not placenta related, are often unexpected and initially confused with obstetric diagnosis: pregnancy can be continued without impairing the rate of therapeutic response,64 and hemorrhagic complications are unusual. Nevertheless, a delay in diagnosis of TTP/HUS may result in life-threatening maternal and fetal consequences.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree