General Overview and Incidence
Mastocytosis is no longer under the broad category of myeloproliferative neoplasm (MPN). Mastocytosis is a heterogeneous disease of clonal neoplastic proliferation and expansions of mast cells (MCs) that are CD117 + /CD25 + /CD2 + and CD34 negative or delete CD34, and involve the skin, bone marrow, spleen, gastrointestinal tract, liver, and lymph nodes with indolent to aggressive forms and can be associated with hematologic neoplasms, systemic mastocytosis (SM)-associated hematologic neoplasm (SM-AHN), further designated into myeloid or lymphoid neoplasms. , Myelodysplastic/myeloproliferative neoplasms (MDS/MPNs) include chronic neutrophilic leukemia (CNL), atypical chronic myelogenous leukemia (CML), myelodysplastic/myeloproliferative neoplasms with ringed sideroblasts and thrombocytosis (MDS/MPN-RS-T), chronic myelomonocytic leukemia (CMMOL-0, 1, 2), and juvenile myelomonocytic leukemia (JMML).
Incidence/Etiology
SM occurs in 1 in 10,000 or 0.89 per 100,000 people per year. MCs are physiologically activated by binding of stem cell factor to the extracellular domains of the Kit receptor with subsequent MC mediator release and/or infiltration of MCs into tissues. Aberrant KIT activation results in increased production of MCs in the skin and extracutaneous organs. Somatic mutations of the coding KIT gene cause autocrine dysregulation and lead to constitutive KIT activation even in the absence of its ligand stem cell factor.
Clinical Presentation
- •
Systemic (fatigue, general malaise, weight loss, anaphylaxis to bee or wasp venom)
- •
Cardiovascular (hypotension, syncope, light-headedness, tachycardia)
- •
Cutaneous (flushing, pruritus, urticaria, angioedema)
- •
Digestive (abdominal cramps, diarrhea, esophageal reflux, nausea and vomiting)
- •
Musculoskeletal (aches, bone pain, osteopenia and osteoporosis)
- •
Neurologic (anxiety, depression, decreased concentration and memory, insomnia and migraines)
- •
Respiratory (nasal congestion, nasal pruritus, shortness of breath, throat swelling, wheezing)
Diagnostic Features/Classification
The updated World Health Organization classification of mastocytosis with additional refined criteria is discussed and referenced. , ,
Laboratory Manifestations/Pathologic Features
- •
Anemia
- •
Thrombocytopenia
SM can involve:
- •
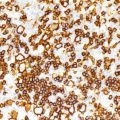
Bone marrow ( Fig. 6.1 )
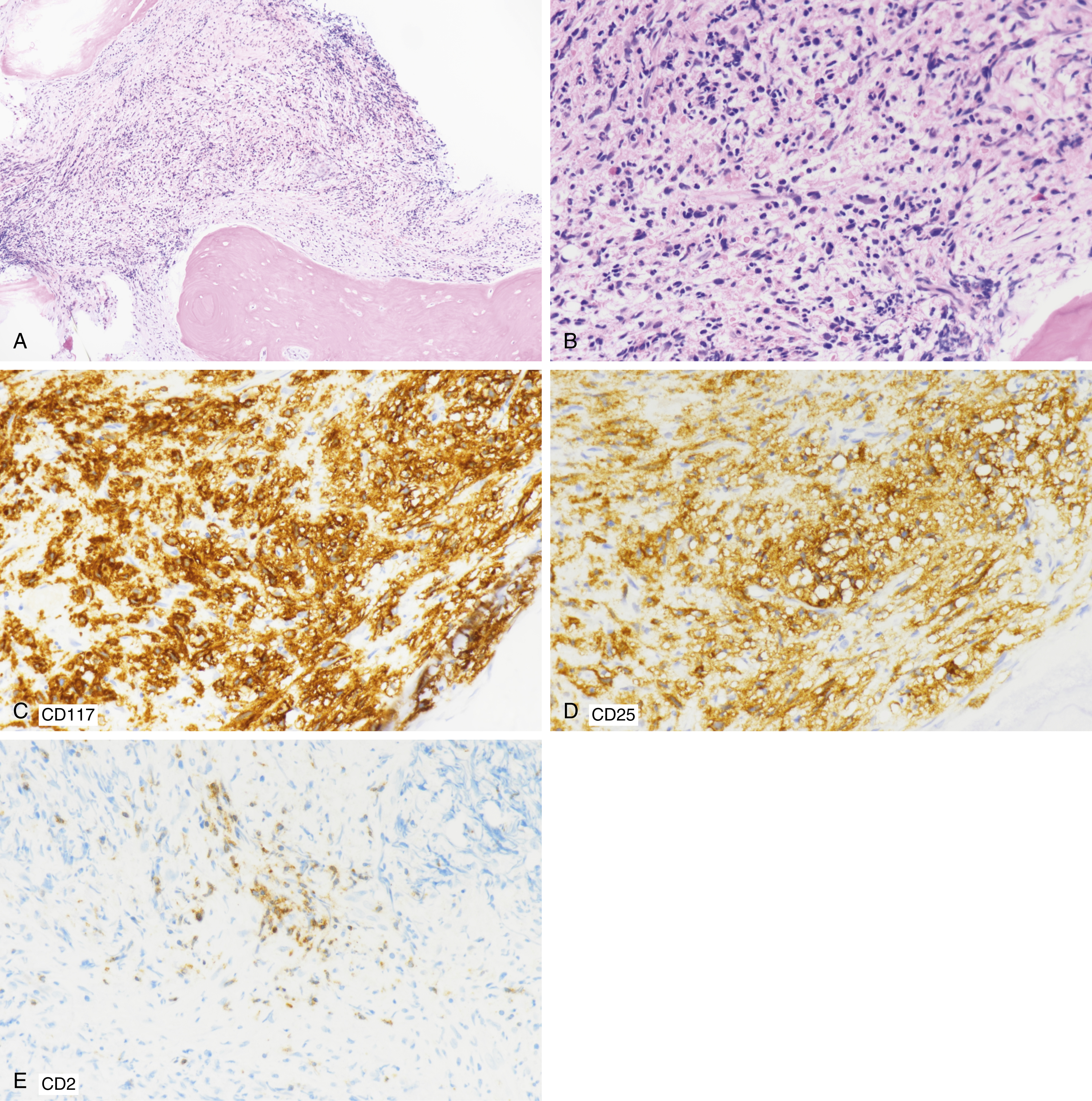
Fig. 6.1
(A) 62-year-old male with systemic mastocytosis. The iliac bone biopsy specimen was hypercellular with fibrosis and osteosclerosis. The clinical differential diagnosis included myeloproliferative neoplasm, myelofibrosis. (B) A 62-year-old male with systemic mastocytosis. The iliac bone biopsy specimen at higher power was hypercellular with fibrosis; scattered eosinophils; marrow with marked crush artifact, fibrosis, eosinophilia, atypical cells with round to slightly elongated nuclei, 70% marrow cellularity, rare megakaryocytes, hypercellularity for age, osteosclerosis, focal osteoblastic activity, and osteoclastic activity (not shown). (C) Immunohistochemical (IHC) staining shows positive CD117 + expression by mast cells. (D) IHC staining shows CD25 + expression by mast cells involving 30% of marrow cellularity, paratrabecular aggregate. Mast cells were also CD34 − , CD71 + erythroid elements, normal CD61 + megakaryocytes by IHC; special stains show 2+ reticulin fibrosis, focal trichrome-positive fibrosis, focal iron stores on PEARL stain (data not shown). (E) IHC shows CD2 + mast cells.
- •
Lymph node ( Fig. 6.2 )
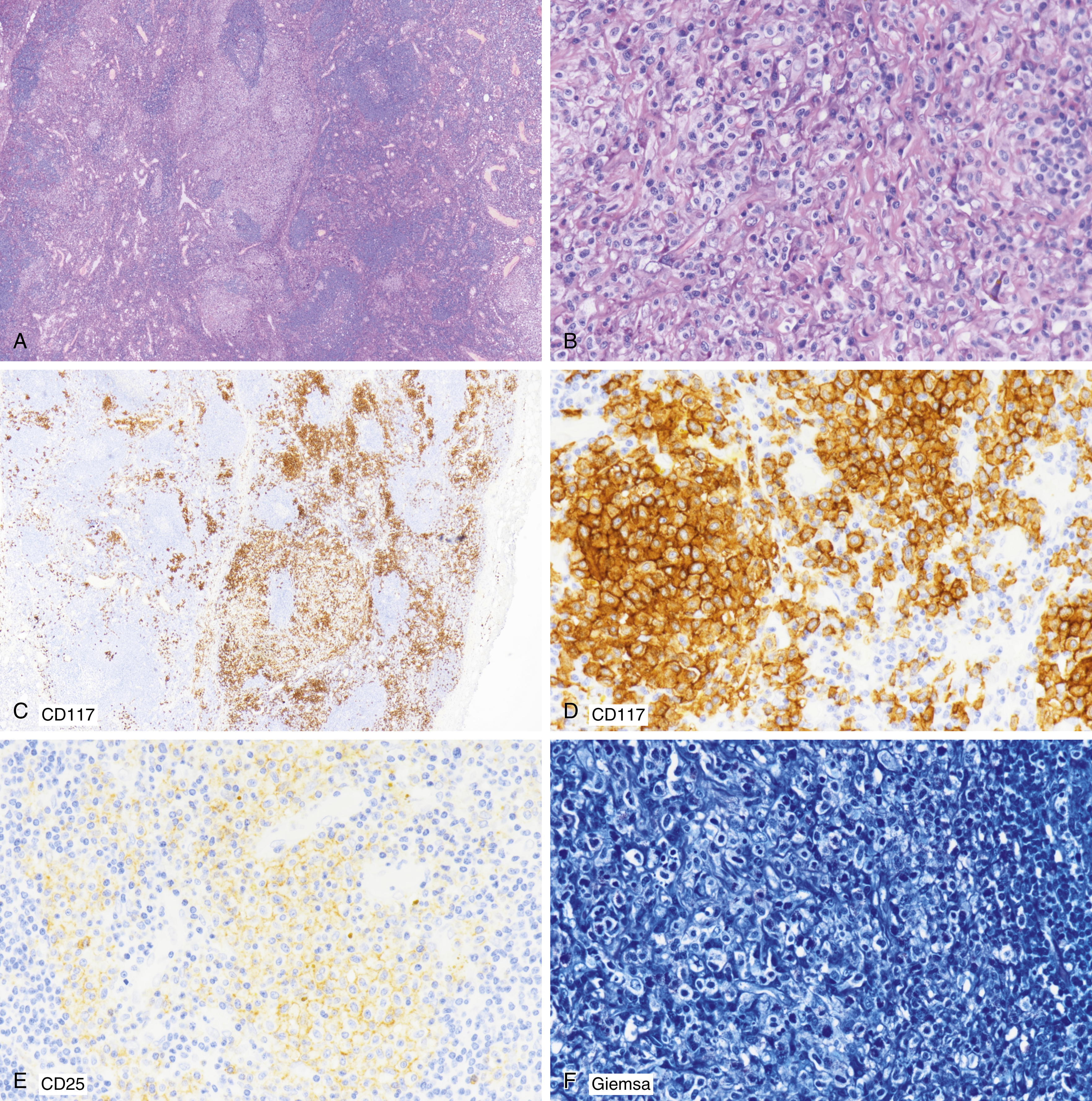
Fig. 6.2
(A) A 62-year-old male with systemic mastocytosis best seen in an accessory splenic lymph node, with paratrabecular mast cell aggregates; pale parafollicular aggregates are noted at low power. (B) Abundant cytoplasm, purplish granules are noted at higher power. (C, D) Immunohistochemical (IHC) staining shows parafollicular CD117 + mast cells. (E) IHC staining shows focal CD25 + mast cells. (F) Giemsa stain shows purple granules of mast cells. (G) This panel shows 1–2+ reticulin fibrosis in a lymph node.

- •
Spleen ( Fig. 6.3 )

Fig. 6.3
(A) 62-year-old male with systemic mastocytosis and splenectomy; splenomegaly, 1346 g; little white pulp with expanded red pulp showing extramedullary hematopoiesis, fibrosis, hemosiderosis, hemorrhage, congestion. (B) A 62-year-old male with systemic mastocytosis in spleen; eosinophils; atypical mononuclear cells with clear cytoplasm; CD117 + and CD25 + (not shown). (C) A 62-year-old male with systemic mastocytosis in spleen; eosinophils; atypical mononuclear cells with clear cytoplasm; CD117 + and CD25 + (not shown); focal fibrosis.
- •
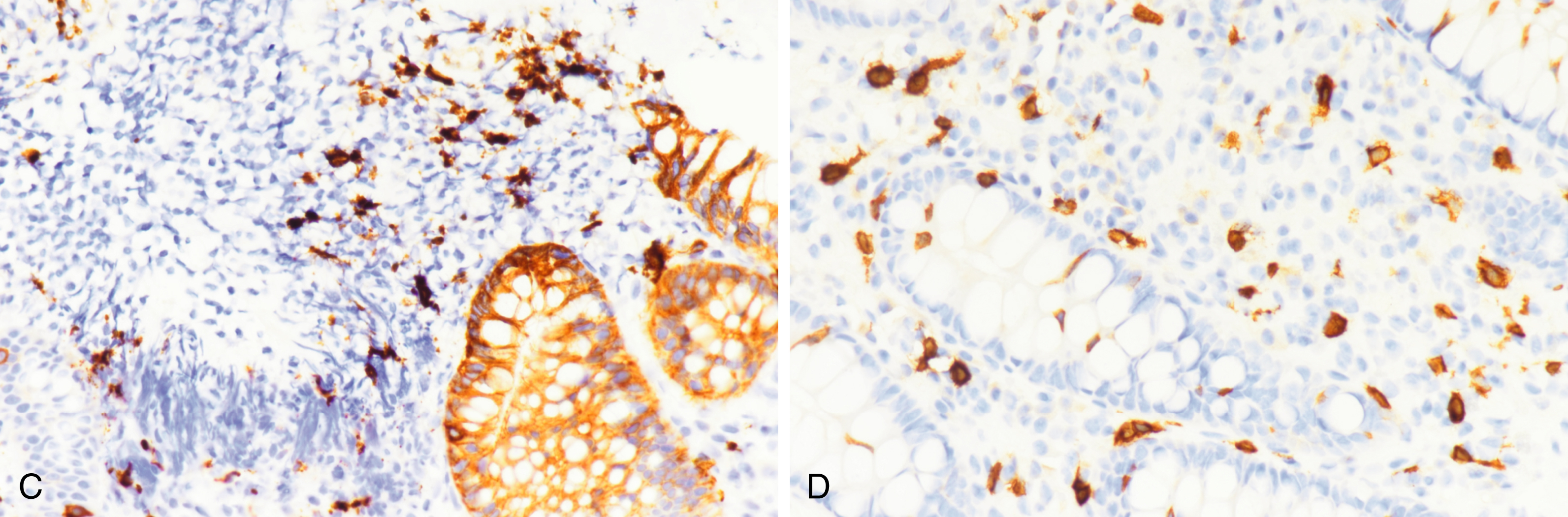
Gastrointestinal tract ( Fig. 6.4A–D )
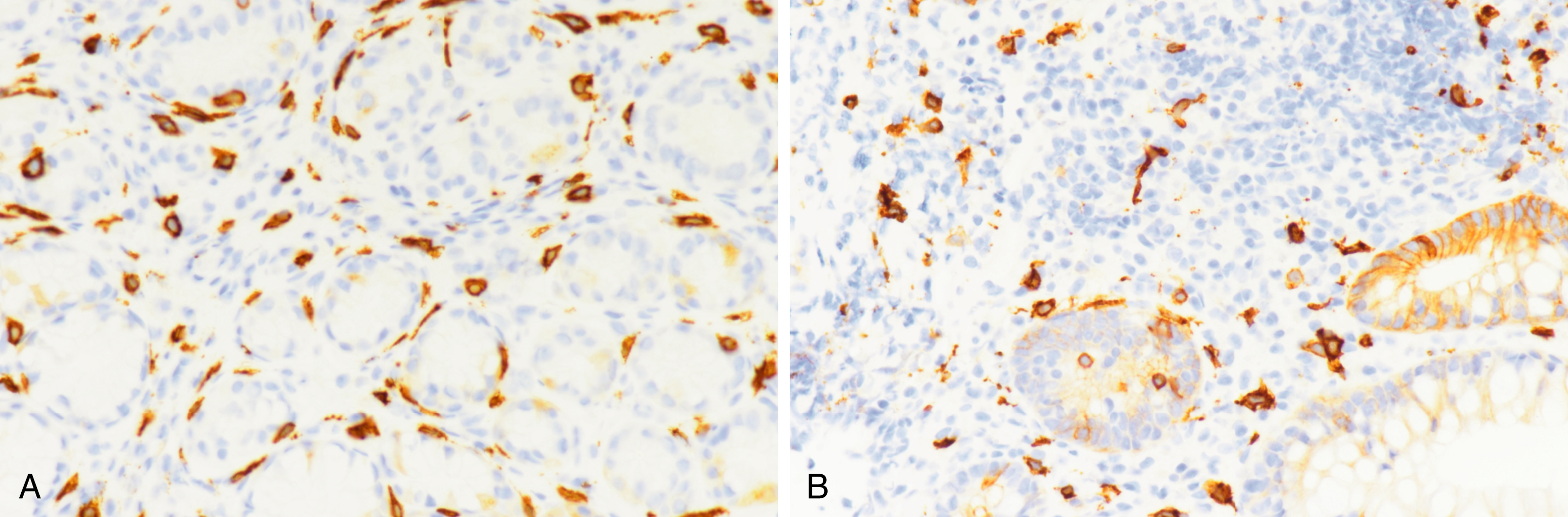
Fig. 6.4
(A) A 64-year-old male with esophagitis and gastritis, with CD117 mast cells in gastric biopsy specimen but did not meet clinical criteria for systemic mastocytosis. (B) A 24-year-old with rectal bleeding. Increased mast cells (CD117 + ) were found in rectal biopsy specimen but did not meet clinical criteria for systemic mastocytosis.
(C) A 24-year-old (same as in B) with rectal bleeding had increased mast cells in rectal biopsy specimen but did not meet clinical criteria for systemic mastocytosis. Mast cells are CD2 − . (D) A 47-year-old male who initially had diarrhea. Rectal biopsy results showed increased mast cells on CD117 but did not meet clinical criteria for systemic mastocytosis. (E) Mastocytosis involving liver; low power magnification shows portal atypical mononuclear proliferation, fibrosis. (F) Mastocytosis involving liver at high-power magnification. (G) CD117 + mast cells in liver involving portal and sinusoidal areas. The upper left corner shows a lower power view of a CD117 + stain of core.