Major Concepts
Outbreaks
Marburg and Ebola hemorrhagic fevers are diseases of unusual severity and high mortality rates that emerged in the late 1960s and 1970s, respectively. While natural infection of humans and nonhuman primates occurs primarily in Africa, monkeys infected with Reston ebolavirus have originated in the Philippines, and their importation led to severe disease in animal colonies in the United States and Italy. Humans contracted fatal cases of Marburg hemorrhagic fever from monkeys brought into Germany and Yugoslavia, and a nonfatal case of infection was reported in the United States in a traveler returning from Africa. Large-scale outbreaks of both Marburg and Ebola hemorrhagic fevers occurred in Africa over the following decades, characterized by fatality rates that at times exceeded 80%, resulting in hundreds of human deaths. Epidemics of Ebola hemorrhagic fever also had a serious impact on populations of some nonhuman primates, such as gorillas, in parts of Africa.
Symptoms
Marburg and Ebola hemorrhagic fevers are similar in clinical presentation and are characterized by chills and high fever; apathy; nausea, vomiting, and diarrhea; disseminated intravascular coagulation leading to depletion of clotting factors; severe hemorrhaging into multiple organs; anemia; multiple organ failure due to loss of tissue oxygenation; shock due to decreased blood pressure; and death. Endothelial cells and monocytes, macrophages, and dendritic cells of the innate immune system are infected by the viruses and produce massive amounts of proinflammatory cytokines that greatly contribute to the pathology. Lymphocyte functions are suppressed by several viral proteins, allowing the viruses to evade the host’s defenses. The filoviruses are resistant to killing by IFN-α and IFN-β, two of the key antiviral cytokines, and also inhibit interferon production.
Infection
Marburg and Ebola hemorrhagic fevers are caused by filoviruses. The Lake Victoria marburgvirus causes Marburg hemorrhagic fever and the Zaire, Sudan, Ivory Coast, and Reston ebolavirus species cause Ebola hemorrhagic fever. Infection with Zaire and Sudan ebolavirus leads to severe disease in humans, whereas Ivory Coast ebolavirus has caused only one nonfatal case in humans, and fatal infection with Reston ebolavirus appears to be restricted to monkeys and apparently does not result in human disease. Filoviruses are enveloped viruses with regularly spaced protruding spikes. Their genome consists of one strand of linear negative-sense single-stranded RNA that contains a unique sequence (UAAUU) at the beginning of start sites and the end of stop sites.
Transmission
Filoviruses are present in high levels in body secretions and may be deposited on the skin by sweating. Marburg and Ebola viruses are transmitted between individuals via droplets of body fluids or through direct contact with infected individuals or objects contaminated with blood or tissue. After recovery, infectious virus may be transmitted sexually for up to seven weeks. Fruit bats are believed be a reservoir host, as infected bats have been captured in western Africa. The indicated species of fruit bats roosts in caves, and many of the outbreaks of Marburg or Ebola hemorrhagic fever have been associated with visits to bat-infested caves or mines.
Protection
Care for persons infected by filoviruses is generally supportive, as proven treatment options are limited. Antiviral compounds have not thus far been effective against these viruses. Administration of heparin, interferon, or human immune serum to patients may or may not increase survival. More recent work has focused on the use of antisense oligonucleotides and short interfering RNA (siRNA) molecules to decrease production of key viral proteins. Other treatment options seek to decrease symptoms such as disseminated intravascular coagulation. Research is progressing in the development of effective antifilovirus vaccines. Other preventive measures involve general improvements in the availability of regional health care and medical supplies and rapid communication to detect and halt outbreaks in their initial stages.
Fueled by movies and books such as Outbreak, The Hot Zone, and The Coming Plague and spurred by sporadic media attention, reports of Ebola and Marburg hemorrhagic fevers have generated fear and curiosity among the American public. While such accounts are often presented in a highly dramatic, graphic, and sensational manner, they have succeeded in periodically bringing public attention to the threat of emerging viral infections. Coverage of emerging infections, however, waxes and wanes in accordance with the general populace’s attention span, while the threat of emerging diseases continues unabated. The Ebola outbreak of 1995 received a great deal of media coverage, but subsequent large outbreaks in Gabon and Uganda went largely unnoticed by most of the world’s press, as were the preliminary stages of the AIDS pandemic in Africa. In addition to the threat of future outbreaks, which may continue to kill hundreds of humans in sub-Saharan Africa, thousands of members of endangered nonhuman primate species, including gorillas, have already died in their sanctuaries in West Africa, further challenging the survival of these animal populations.
The first known instance of Marburg hemorrhagic fever (MHF) occurred in 1967 in vaccine production facilities in Marburg and Frankfurt, Germany, and Belgrade, Serbia (at the time, part of Yugoslavia). The outbreak began among 25 persons working with African green (vervet) monkeys from Uganda (primary cases) and later spread to six of their family members or health care workers (secondary cases). Seven of the primary cases died (mortality rate of 28% among primary cases).
Another small outbreak occurred in 1975, originating with a tourist who had a history of recent travel in Zimbabwe and South Africa. Two cases of secondary infection resulted: a traveling companion and a nurse, both of whom survived. In 1980, two persons were infected in western Kenya. These people had visited the Kitum cave, which was believed to be the source of the infection. Later, researchers placed sentinel animals in the cave, but none of them became infected. A large number of different animal species were trapped in the vicinity of the cave (including rodents, bats, insects, grazing animals, and large African cats). These also had no sign of the causative virus. Laboratory tests did find, however, that the virus is able to replicate in experimentally infected bats. Lake Victoria marburgvirus (Marburg virus), the causative agent, has subsequently led to disease in several areas of Africa, including Uganda, western Kenya, South Africa, and Zimbabwe. Far more deadly epidemics of MHF occurred among gold miners near Durba in the Democratic Republic of Congo (DRC; formerly Zaire) in 1998–2000, with 154 cases and 128 deaths (mortality rate of 83%) and in the Uige province of Angola in 2004–2005 (374 cases, 88% mortality). An outbreak of MHF also occurred in 2008 in a bat-infested mine in Uganda. Disease spread in many of these outbreaks was amplified by unsanitary injections given in health care centers or private clinics or by self-administration in homes.
RECENT DEVELOPMENTS
Marburg viral RNA and antiviral IgG antibody were detected in a common species of fruit bat, Rousettus aegyptiacus, trapped in caves in Gabon in 2005 and 2006. Many of the human cases of MHF have been associated with caves. Unlike most fruit bats, this species is known to roost in caves, and its geographical range includes the locales in which outbreaks of MHF have occurred. This is the first naturally infected nonprimate species thus far identified with this virus and the first detection of the virus in that part of western Africa. This discovery follows the identification of asymptomatic infection of three species of fruit bats with the Ebola virus in Gabon and the Congo Republic in 2004.
The first case of MHF in the United States was detected in a traveler returning to Colorado from a trip to Uganda in January 2008. He had visited the bat-infested “python cave” in Maramagambo Forest, Queen Elizabeth Park, in the western part of that nation. The U.S. tourist recovered; however, another cave visitor from the Netherlands acquired a fatal case of MHF in July of that year. This cave is about 60 kilometers from the Kitaka gold mine, the source of a large disease outbreak in Uganda in 2008. The mine contains large numbers of fruit bats. A band was found in the python cave that had been used to tag a bat from the Kitaka mine, indicating that bats did indeed travel between the two sites.
A similar disease, Ebola hemorrhagic fever (EHF), emerged in 1976 in two simultaneous outbreaks involving over 550 persons in the DRC and Sudan. The mortality rate was very high—88% in Zaire and 53% in Sudan. The outbreak in the DRC began in a missionary hospital in Yambuku, in the vicinity of the Ebola River, and spread rapidly among patients, health care providers, and patients’ relatives. The patients were taken to a regional center in Kinshasa. Most of the primary cases (72 of 103, or 70%) were spread by the local hospital via improperly sterilized needles used for multiple patients. Of the persons infected by secondary contact with an infected person, 43% survived, compared to only 7.5% of those infected by a contaminated needle. In that outbreak, the Ebola strain was passed for four generations in humans and then disappeared for no apparent reason.
At approximately the same time, a separate epidemic of this hemorrhagic fever began in Maridi and N’zara in Sudan and rapidly spread to members of the medical staff. This outbreak had a lower mortality rate than that occurring concurrently in the DRC. An investigator in Porton Down, England, was subsequently infected with virus from this outbreak following an accidental injection into his thumb. He was given antifungal medication, interferon, and immune serum and survived the infection. The major risk factors in this outbreak were determined to be the performance of local rituals of preparing relatives’ bodies for funerals and association with the regional hospitals (nosocomial spread). Up to 30% of the health care workers became infected in this outbreak. N’zara had a population of approximately 20,000 and was the economic center of the area due to its cotton factory. This factory was infested with bats, rats, boll weevils, and spiders, and all of the early cases were among factory workers. This outbreak passed through at least eight generations in humans. Over 400 miles separated these epidemics in the DRC and Sudan. Due to the extremely poor road conditions at the time, the differences in mortality rates, and differential ability to survive multiple passages in humans, it is unlikely that the disease was spread to Sudan by a person traveling between the two areas; it is more likely that these were separate outbreaks involving different strains of the causative agent, which were later designated as Zaire ebolavirus (Ebola Zaire) and Sudan ebolavirus (Ebola Sudan).
FIGURE 12.1 Surveying for infection during the 1976 Ebola outbreak in Zaire
Source: CDC/J. Lyle Conrad.
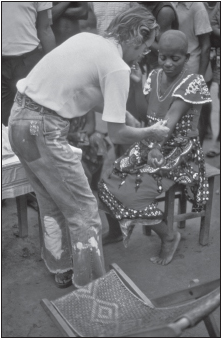
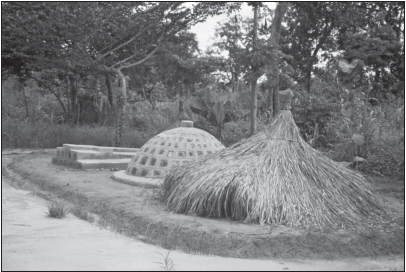
FIGURE 12.2 Graveyard containing some of the first victims of the Ebola outbreak in Sudan in 1976
Source: CDC/J. Lyle Conrad.
A second major epidemic of Ebola Zaire occurred in 1995 in Kikwit, Zaire, about 1,000 kilometers from the site of the previous outbreak. The index case was a surgical patient, and disease spread by nosocomial transmission to health care providers, others in the hospital, and family members, resulting in 245 deaths. In 1996–1997 (Gabon) and 2000–2001 (Gulu, Uganda), large outbreaks involved 98 persons with 66 deaths (67% mortality rate) and 425 people (83% mortality), respectively. EHF has occurred in other parts of Africa, such as the Central African Republic, Nigeria, the Ivory Coast, Liberia, Kenya, Congo Republic, and Cameroon, where antibodies to the virus were found in 15% of the local pygmies. Wild chimpanzees and gorilla populations (including mountain gorillas) have also suffered large losses.
A different subtype of Ebola is named after an outbreak among primates in Reston, Virginia, in 1989. It caused lethal infection of cynomolgus monkeys held in quarantine facilities in Virginia, Texas, and Pennsylvania. Many of the animals became severely ill and died, and the rest were euthanized. Several of the human caretakers were also infected, as evidenced by the production of antibodies, but no humans demonstrated disease symptoms. The monkeys in these outbreaks originated in the Philippines. This strain is known as Reston ebolavirus (Ebola Reston), and it is not virulent in humans, although it does share antigenic cross-reactivity with the other Ebola strains. Due to the spread of infection to animals in all parts of the quarantine facility, it is likely that Ebola Reston may have been spread by airborne transmission. On several subsequent occasions during 1989, 1990, and 1996, Ebola Reston killed monkeys in colonies in the United States. These animals had been purchased from the Ferlite Scientific Research monkey farm in the Philippines. Some of the people at the colony in Texas and several of the workers at the facility in the Philippines also produced antibodies to the virus but did not become ill. Ebola Reston was also found in cynomolgus monkeys imported from the Philippines in Italy in 1992.
The fourth subtype of Ebola virus, Ivory Coast ebolavirus (Ebola Ivory Coast, formerly Ebola Tai), was found in 1994 in a scientist performing an autopsy on a wild chimpanzee that had died of a hemorrhagic disease in the Tai Forest of the Ivory Coast. She developed a serious acute illness characterized by fever and rash, but no hemorrhage, and survived the infection. No subsequent cases of infection with Ebola Ivory Coast are known to have occurred.
Both the Marburg and Ebola viruses cause serious and often fatal hemorrhagic fever in humans and some nonhuman primates. Pathological responses entail an intense, systemic inflammatory response similar to septic shock, resulting from an overwhelming activation of infected monocytes, macrophages, and dendritic cells, which produce large amounts of proinflammatory cytokines. This hyperactivation of the innate immune system is responsible for much of the subsequent pathology induced by filoviruses. The severity of the symptoms and the high mortality rates associated with these diseases have made them popular topics for the media and for several best-selling movies and books.
Marburg Hemorrhagic Fever (MHF)
Marburg hemorrhagic fever (MHF) has an abrupt onset with severe headache, high fever, chills, and back pain. This is followed by severe watery or bloody diarrhea, abdominal cramping, vomiting, and a rash on the trunk. Severe bleeding (hemorrhaging) occurs from multiple sites, particularly the gastrointestinal tract, gums, eyes, and lungs, within five to seven days of onset. Disease manifestations include jaundice, inflammation of the pancreas, severe weight loss, delirium, central nervous system involvement, terminal shock, liver failure, pulmonary edema, and multiorgan dysfunction. Major lesions may be present in the liver (focal hepatic necrosis), spleen, lymph nodes (follicular necrosis), and kidneys and are accompanied by hemorrhaging in the gastrointestinal tract; the pleural, pericardial, and peritoneal spaces; and the renal (kidney) tubules. Laboratory findings include severe thrombocytopenia, leading to the hemorrhagic manifestations; hemoconcentration; and amylase, blood urea nitrogen, creatinine, and transaminase elevation, with aspartate aminotransferase (AST) greater than alanine aminotransferase (ALT). A profound leucopenia may result from apoptosis of lymphocytes; the resultant drop in immunity may lead to secondary bacteremia. Death may occur after 7 to 16 days due to shock resulting from severe decreases in blood pressure following hemorrhaging. The mortality rate ranges from 23% to 88%. MHF occurs in humans, Old World primates, and guinea pigs but not in mice or New World primates.
Ebola Hemorrhagic Fever (EHF)
Infection with the Ebola Zaire or Ebola Sudan virus results in a disease similar to MHF. Following an incubation period of 2 to 21 days (most commonly, 7 to 14 days), Ebola hemorrhagic fever (EHF)
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree