Borderline breast lesio(ns diagnosed on core needle biopsy
Upgrade to malignancy
Upgrade to malignancy
Increase relative risk of breast ca
DCIS (%)
IDC (%)
30–40
20
4–6
Lobular neoplasia
20*
4–5
30*
8–12
40–60 (ILC)
Columnar cell lesions
25–33*
9–15*
Papillary breast lesion
Intraductal papilloma (IDP) [15]
8*
5–9*
1.8–3
18–30**
Patient counseling following identification of a borderline breast lesion must take into account an assessment of concordance between the clinical suspicion and CNB result, an estimation of the risk and implications of associated lesions of greater clinical significance (such as malignancy), and knowledge of the natural history of the specific high-risk lesion identified. The Gail risk model, along with other risk assessment models, has been increasingly used to estimate future breast cancer risk based on the results of breast biopsy [21, 22]. Utilizing the Gail model in clinical trial enrollment, the NSABP P-1 study first showed a significant reduction in the incidence of breast cancer in women at higher risk, including those with ADH and lobular neoplasia, when tamoxifen therapy was administered. Subsequently, risk assessment along with individual care plans for borderline breast lesions has become standard of care [23, 24]. In the clinical management of borderline breast lesions today, risk assessment assists in informing appropriate follow-up, prevention, and screening discussions, including the use of breast MRI [25]. When these high-risk lesions are identified by CNB, management may include structured observation, repeat CNB, or surgical excision, and the chosen care pathway must represent a practice of informed discussion with the patient and shared decision-making.
Atypical Ductal Hyperplasia (ADH)
Atypical ductal hyperplasia (ADH) is described as a breast lesion involving the epithelial cells within the ductal system that is felt to be not only a precursor on the continuum from normal breast tissue to breast carcinoma but also a risk factor for future breast cancer. The model for a linear progression from hyperplasia to invasive breast carcinoma was initially described by Wellings and Jensen [26]. This model proposes a natural progression along a histologic continuum through an accumulation of molecular changes, ultimately resulting in an invasive phenotype. Flat epithelial atypia (FEA), ADH, and DCIS are accepted as the non-obligate precursors to invasive ductal carcinoma. This model is supported by morphologic, immunohistochemical, and transcriptional profiling data [27]. For example, ADH is described as a ductal epithelial lesion containing some, but not all, of the features of DCIS. A diagnosis of ADH on CNB is complicated by its similar appearance to low-grade DCIS, with only quantitative differences.
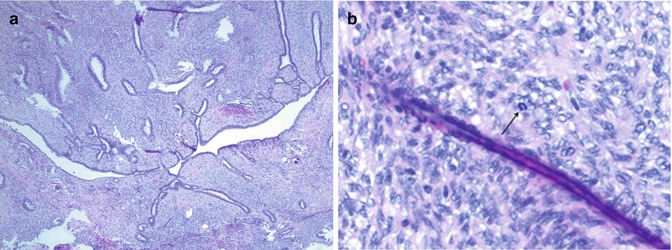
Typically, ADH is detected by screening mammography as microcalcifications in an asymptomatic patient, and ADH represents 10 % of radiographically detected lesions [4]. Morphologically, a diagnosis of ADH requires atypical but uniform epithelial cells which partially or completely fill the ductal spaces, with a maximal dimension of 2 mm for each focus, distinguishing it from low-grade DCIS [5, 10, 28] (Fig. 5.1a, b). Due to the limited tissue sampling with CNB and the varied benign and malignant lesions associated with ADH, a diagnosis of ADH by CNB has a well-recognized potential for coexistent DCIS or invasive cancer that is related to sampling size [28] (Fig. 5.1c, d). Furthermore, FEA, ADH, and DCIS have been shown to display similar genetic alterations and chromosomal aberrations, such as loss of 16q, and progression to invasive cancer has been proposed to occur along potentially multiple such pathways through the acquisition of genetic alterations under selective pressure [27]. As a result, ADH is commonly found to be coexistent in the setting of other high-risk breast lesions as well as DCIS and invasive carcinoma [5, 10, 28].
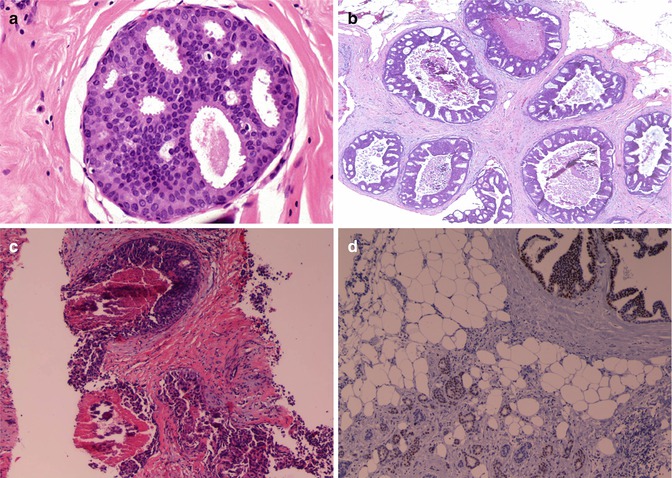
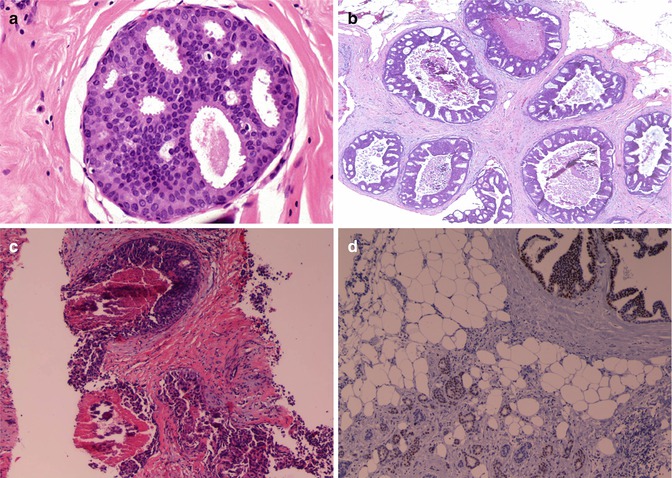
Fig. 5.1
(a) Single duct with monotonous, atypical, but uniform epithelial cells which partially or completely fill the ductal spaces with maximal dimension of 2 mm consistent with ADH. If more ducts like this present or expanded duct measures more than 2 mm, then it qualifies as low-grade cribriform DCIS. (b, c) DCIS with central comedo necrosis and calcification in the middle, in purple. (d) Cribriform DCIS (upper right) and invasive ductal carcinoma both strongly positive with nuclear estrogen receptor (Courtesy of Marina Mosunjac, MD Emory University Atlanta)
At the same time, ADH also represents a marker for elevated risk of future cancer. Even in the absence of synchronous associated malignancy, a diagnosis of ADH incurs at least a four to five times relative risk of subsequent breast cancer diagnosis, perhaps as high as sixfold in premenopausal women [6]. This increased risk is evident in both the ipsilateral and contralateral breast [4, 7]. When malignancy is found in a surgical excision following a CNB diagnosis of ADH, an “upgrade” in diagnosis is said to have occurred. A wide range of upgrade percentages have been reported in the literature, with rates as low as 4 % and as high as 87 % [5]. One of largest recent retrospective studies looking at 422 CNB diagnoses of ADH reported an upgrade percentage of 31.3 %, with the majority upgrading to DCIS (22.7 %) [7].
Additionally, the presence of multiple radiographic foci of ADH has been shown to increase the rate of associated malignancy identified if excisional biopsy is subsequently performed (7 % for 1–2 foci vs. 39 % for >2 foci) [4]. In addition to discussion of the risk of concurrent malignancy, management of ADH must also include an estimation of the implied relative risk for future diagnosis of breast cancer. Lifestyle modifications, including avoiding risk factors such as prolonged use of hormone replacement therapy and increasing protective factors such as low fat diet and exercise, are believed to impart a modest risk reduction for development of future breast cancer. The original report of the breast cancer prevention trial, NSABP P-1, in 1998 [23] established the efficacy of tamoxifen use in reducing the risk of future breast cancer in patients with above-average risk by almost 50 %. Importantly, ADH patients in this trial received the most benefit, reducing risk of cancer by 86 %. Meanwhile, prophylactic surgery for the diagnosis of ADH alone is controversial [29, 30]. In summary, when ADH is identified by CNB, excision should be strongly considered in order to evaluate for coexistent malignancy. When malignancy is not identified following excision, informed discussion should include an estimation of future risk of malignancy as well as an acceptable plan for surveillance and risk reduction, including lifestyle modifications and chemoprevention with hormonal therapy.
Lobular Neoplasia: Atypical Lobular Hyperplasia (ALH) and Lobular Carcinoma In Situ (LCIS)
Lobular proliferative lesions include atypical lobular hyperplasia (ALH) and lobular carcinoma in situ (LCIS). LCIS was first describe by Ewing in 1919, and later the term lobular neoplasia (LN) was coined by Haagensen in 1978 to encompass both ALH and LCIS [31]; however, the term has not gained universal acceptance. Linear progression models for lobular breast changes are less well studied than their ductal counterpart, although some recent genetic and molecular studies have displayed similar genetic changes in ALH and LCIS with both IDC and invasive lobular carcinoma (ILC) [27]. LN represents a continuum from ALH to pleomorphic LCIS (pLCIS), the most aggressive subtype of LCIS [8]. LN is characterized by atypical epithelial cells with intraepithelial lobular proliferation of terminal duct-lobular units with differing degrees of filling and atypia. ALH and LCIS can be distinguished by the amount of acini involvement. LCIS is diagnosed by acini involvement of more than half with no central lumina where ALH has less than half of the acini affected [8, 10] (Fig. 5.2a, b). When unable to differentiate ductal versus lobular features, particularly important in the pleomorphic variant, the cellular adhesion molecule E-cadherin is utilized. Negativity for E-cadherin is a hallmark molecular feature of lobular histology (Fig. 5.2c, d).
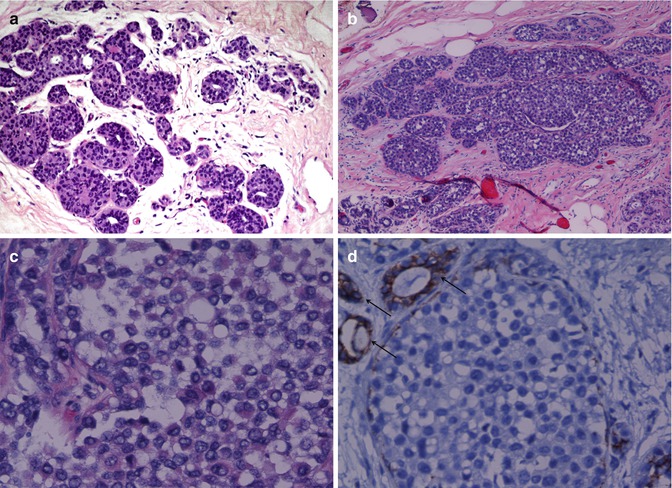
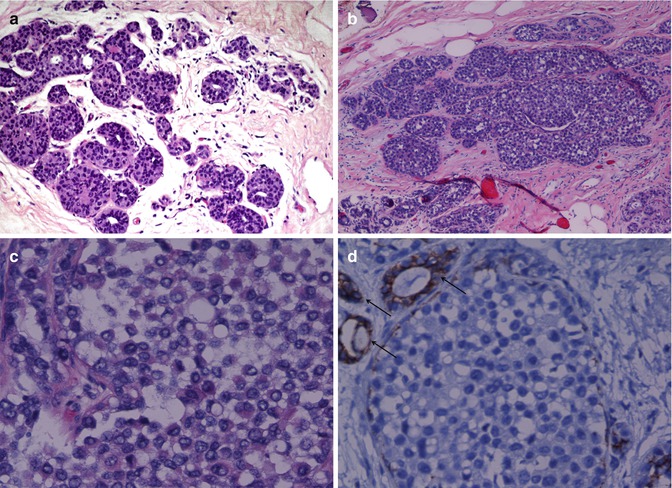
Fig. 5.2
(a) Atypical lobular hyperplasia ALH with mildly expanded lobules with monotonous smaller cells, not enough for LCIS. (b) Lobular carcinoma in situ. Extended lobules filled with small dyscohesive uniform cells. There is a feel of “bag of marbles,” and if you were to turn the slide upside down, the marbles would fall out, different from DCIS where cells usually are more tightly packed. (c) Lobular carcinoma in situ: at higher power, the dyscohesiveness of the LCIS cells. (d) E-cadherin, membranous stain, not staining LCIS but staining adjacent ducts (Courtesy of Marina Mosunjac, MD Emory University Atlanta)
Pleomorphic LCIS, which can be thought of as a separate entity due to its aggressive natural history, is distinguished by its approximately four-times larger nuclei and significant nuclear pleomorphism. Although LCIS and pLCIS are normally ER/PR positive (pLCIS can be negative), and E-cadherin negative, pLCIS may show HER2 overexpression, p53 positivity, and an elevated Ki67 index compared with LCIS. pLCIS also shows similarities to DCIS with occasional chromosomal deletions and ontogenesis. These features have significant implications when evaluating upgrade percentage and breast cancer risk with pLCIS, which is universally considered as a precursor lesion to breast cancer [8, 10]. LN is typically an incidental diagnosis without specific physical exam or radiographic findings, although it may be associated with microcalcifications in the pLCIS subtype. When LN is diagnosed, up to 85 % are multicentric and 50 % are multifocal, with up to one third with LN identified in the contralateral breast [4, 10].
LN has classically been considered a marker of future breast cancer risk, and not a precursor lesion, and management is still somewhat controversial, particularly in cases without a radiographic abnormality. The average age for the diagnosis of LN is between 44 and 47 years. It is 12 times more common in white than black patients [32]. The relative risk for the development of breast cancer in a patient diagnosed with LN is four- to fivefold for ALH and about eight- to ninefold for LCIS [9]. With LCIS, the cumulative risk of ipsilateral and contralateral breast cancer is similar (18 % and 14 %, respectively) with 40 % being ILC and 60 % IDC [11]. When excised, an upgrade in diagnosis from LN to malignancy is reported to occur at rates ranging from 0 to 50 % [8]. This wide range is likely related to the limited radiographic findings, variable indications for excision, and inherent differences between the subtypes of LN. A recent meta-analysis of over 1,200 LN patients displayed upgrade percentages of 19 % of the ALH cases, 32 % of the LCIS cases, and 41 % (40–60 % in the literature) of the pLCIS cases [8].
Management of LN diagnosed by CNB must start with an assessment of clinical and pathologic concordance, as the diagnosis of LN often is not related to the underlying clinical findings. LN typically presents with limited suggestive history or exam and imaging findings (excluding the pLCIS subtype), indicating a need to consider the possibility of misdiagnosis following CNB and the possibility for alternative diagnoses following any proposed excision. Management of pLCIS is unique from management of LN in general. Due to its high associated underlying risk of invasive lobular carcinoma of about 40–60 %, it is considered a precursor lesion, and excision with negative margins should be recommended in all patients when seen on CNB.
For the remaining LN lesions, surveillance may be appropriate when another concordant benign pathologic lesion, such as a fibroadenoma, is identified in the CNB specimen. Repeat biopsy or surgical excision may be considered appropriate in the setting of clinical-pathologic discordance, identification of another associated high-risk lesion, or presence of unusual histologic features such as mitoses or necrosis. In such instances, underlying DCIS and invasive carcinoma are more likely to be identified [5]. Compared to the general population, ALH carries 4- to 5-fold and LCIS 8- to 12-fold greater lifetime risk of developing invasive cancer [33, 34]. When ALH or LCIS is diagnosed, an informed discussion must also include an established plan for surveillance, including possible MRI, lifestyle modifications, chemoprevention with hormonal therapy, and bilateral prophylactic mastectomy.
Columnar Cell Lesions: Flat Epithelial Atypia and Columnar Cell Hyperplasia with Atypia
Columnar cell lesions (CCLs) were first described in the literature in 1979 [35, 36] as “monomorphic clinging carcinoma in situ,” and the term flat epithelial atypia (FEA) was more recently recognized by the World Health Organization to describe CCLs with atypia. The overall incidence of finding CCLs by CNB has been increasing recently with a current prevalence of 3.7–10 % [13]. CCLs are not normally diagnosed on physical exam, but radiographically they can be associated with pleomorphic calcifications [4]. Histologically, CCLs are characterized by enlarged terminal ductal-lobular units with dilated acini lined with columnar cells and with associated apical snouts. Columnar cells are epithelial cells that are columnar in shape, giving them their name (Fig. 5.3a, b). Elongated nuclei and intraluminal secretions are also noted. Cytologically, CCLs are composed of similar progenitor cells to ADH and DCIS and include a spectrum of lesions, including columnar cell change (CCC), columnar cell hyperplasia (CCH), and FEA. As previously discussed, these lesions, particularly FEA, are felt to be early in the spectrum from normal breast tissue to carcinoma. CCC is distinguished by having only two layers of cells, without atypia, lining the ductal components, while CCH exhibits greater than 2 layers of cells, and FEA displays associated atypia (Fig. 5.4a, b).
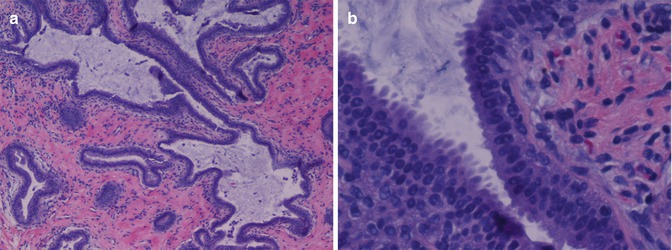
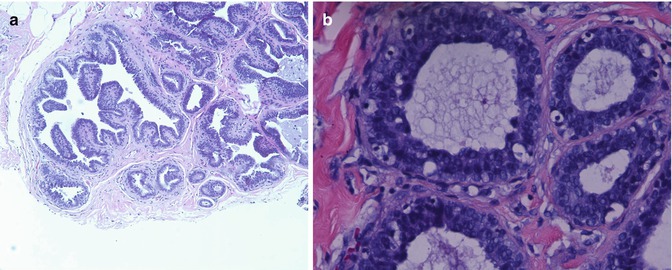
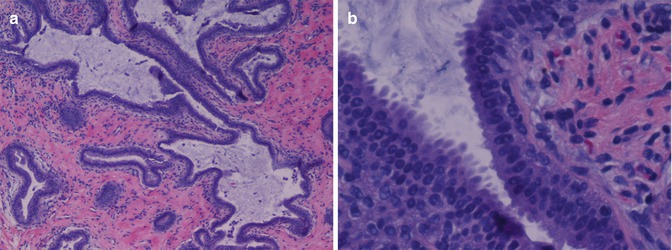
Fig. 5.3
(a, b) Columnar cell lesions are characterized by enlarged terminal ductal-lobular units with dilated acini lined with columnar cells and with associated apical snouts. Columnar cells are epithelial cells that are columnar in shape, giving them their name (Courtesy of Marina Mosunjac, MD Emory University Atlanta)
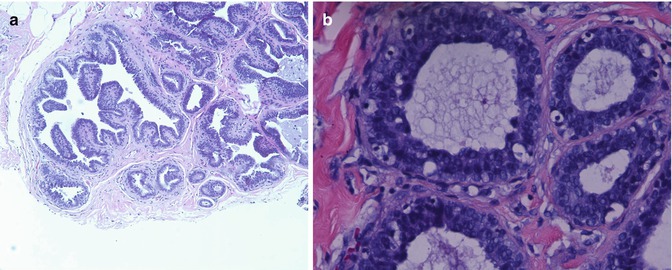
Fig. 5.4
(a) Columnar cell hyperplasia. Cysts lined by orderly columnar cells with minimal atypia. (b) Flat epithelial atypia (FEA) cysts lined by pseudostratified slightly disordered larger atypical cells (Courtesy of Marina Mosunjac, MD Emory University Atlanta)
A grading system (low, medium, high) has been proposed to describe the degree of atypia noted [10, 13]. ADH is distinguished from columnar cell lesions (CCLs) by the degree of cytonuclear atypia and abnormal architecture [13]. The majority of CCLs display ER/PR positivity. While considered benign lesions, CCLs have a known association with other high-risk benign lesions and malignancy. The diagnosis of CCLs may possibly represent a risk factor for and/or early precursor to carcinoma, although this is yet to be proven [5, 13, 27]. When excised, CCLs with atypia are found to occur concurrently with other high-risk benign lesions 25–33 % of the time, with associated ALH and ADH being identified at a rate of 5 and 3.5 %, respectively [4, 5, 12].
Additionally, the reported rate of upgrade in diagnosis to in situ or invasive cancer following excisional biopsy for CCLs has been reported at rates ranging from 0 to 26 %. These rates have been shown to be significantly higher for CCH (20 %) and FEA (9 %) when compared to CCC; however, the true rate of associated malignancy is difficult to estimate, as many lesions are managed without excision [13, 14]. In practice, the management of CCH and FEA often differs from the management of CCC based on the described disparity in associated risk. Surgical excision should be presented as the preferred management whenever CNB of a breast lesion yields a diagnosis of CCH or FEA. Occasionally, continued surveillance is also discussed with patients in the setting of an informed discussion. Interval clinical and imaging follow-up is more often practiced following a CNB diagnosis of CCC.
Papillary Lesions
Papillary breast lesions (PBLs) span a wide pathologic spectrum ranging from benign to malignant and include intraductal papilloma (IDP), atypical papilloma, intracystic papillary carcinoma, and invasive papillary carcinoma. PBLs present with a diverse clinical behavior and radiographic presentation. Radiographically, PBLs can present as architectural distortion, asymmetric density, and occasionally a palpable breast mass with or without associated microcalcifications, or microcalcifications alone. However, mammography and ultrasonography cannot reliably distinguish benign from malignant PBLs [37]. The hallmark of PBLs is the formation of papillary structures composed of two layers of cells, one epithelial and one myoepithelial, on a fibrovascular core (Fig. 5.5a–c). Distinguishing among the spectrum of papillary lesions, such as an atypical papilloma versus DCIS arising within a papilloma, can be very challenging for the pathologist. Additionally, other proliferative lesions can be present at the periphery of the suspicious mass or area, further complicating the diagnosis.
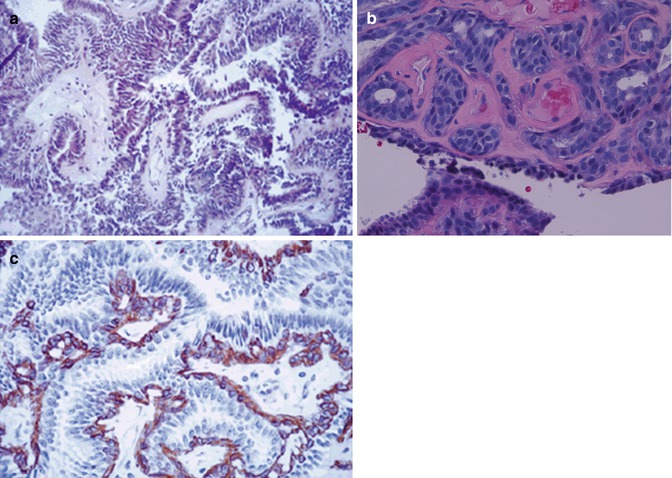
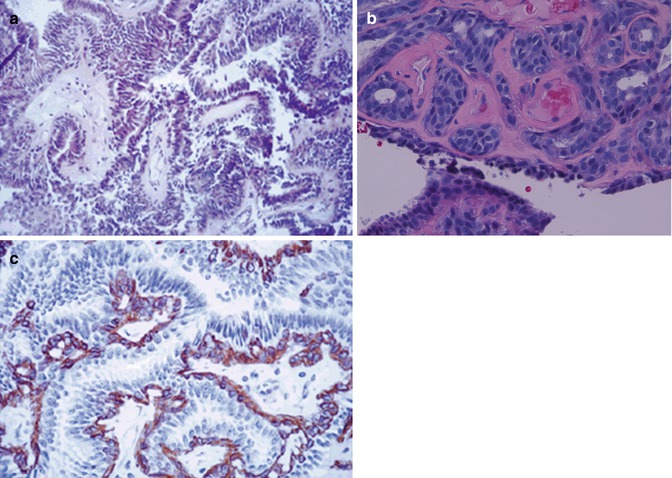
Fig. 5.5
(a, b) Benign intraductal papilloma (IDP) of the breast showing fibrovascular cores lined by two distinct layers of cells, myoepithelial cells and ductal cells. (c) Calponin stain (×400) specifically delineates myoepithelial cells in a benign IDP (Courtesy of Marina Mosunjac, MD Emory University Atlanta)
Moreover, the accurate diagnosis on CNB can be difficult because of fragmentation, limited material, sampling error, or presence of other nonneoplastic proliferations, such as florid papillomatosis, radial sclerosing lesions (RSLs), and micropapillary hyperplasia [10]. Yet, as percutaneous stereotactic or ultrasound-guided CNB has been used increasingly in the diagnosis of clinically occult and palpable breast lesions, recent data have suggested that benign papillary lesions (mainly IDPs) can be diagnosed accurately by CNB [38, 39]. In spite of the inherent limitations of CNB, papillary lesions account for approximately 5–10 % of all CNBs, and the subsequent decision about clinical treatment is now based largely on the CNB diagnosis [40, 41].
A number of studies have been published on the management of atypical papillary lesions, inclusive of IDP with atypia or IDP with associated ADH, with most recommending surgical excision based upon the increased risk of associated DCIS and invasive carcinoma [37, 40–42]. In contrast to atypical papillary lesions, the management of benign IDP remains controversial, with no clear consensus on the optimal approach to management. The reported incidence of finding a more advanced lesion (ADH, DCIS, and invasive carcinoma) on follow-up excisional biopsy after the diagnosis of benign IDP on CNB ranges from 0 to 25 % [43]. In one retrospective review [44] of 276 consecutive cases of IDP undergoing surgical excision, there was a clear higher rate of upgrade in diagnosis to DCIS/IDC when compared to isolated IDP, 33 %/5 % vs. 8 %/1 %, respectively. For isolated IDP, an 18 % upgrade in diagnosis to ADH was also noted. Therefore, even when CNB demonstrated benign IDP, an upgrade in diagnosis to a lesion of greater clinical significance was demonstrated 27 % of the time following excisional biopsy [44]. While the clinical significance of identifying IDC/DCIS is appreciated, an upgrade in diagnosis to a benign lesion such as ADH can have significant patient management implications. Surgical excision is the current recommendation considered as optimal management for all breast papillary lesions identified on CNB.
Radial Sclerosing Lesions: Radial Scar and Complex Sclerosing Lesions
Radial sclerosing lesions (RSLs) of the breast are a group of benign, stellate-appearing breast lesions, with the incidence of radial scars identified on CNB ranging from 4 to 26 %. These lesions have been referred to by several different names, including scleroelastotic lesion, indurative mastopathy, nonencapsulated sclerosing lesion, and sclerosing papillary proliferation [45]. RSLs are often categorized by size as either radial scar (<1 cm) or complex sclerosing lesion (>1 cm). These lesions can have a clinical and radiologic presentation as well as gross pathologic appearance resembling that of carcinoma [10]. Typically, patients diagnosed with RSLs have no particular exam or imaging findings, and RSL is often an incidental finding on CNB biopsy for another concordant abnormality. However, patients may also present with a palpable breast mass. Mammographic findings, when present, usually display a spiculated lesion with dense radiolucent cores and thin spicules radiating out from the core, which can be nearly impossible to distinguish from carcinoma [15, 46] (Fig. 5.6a, b). Histologically, RSL are characterized by fibroelastotic cores with ducts and lobules radiating centrifugally with typical or atypical epithelial proliferative changes or cysts [10, 15, 45].
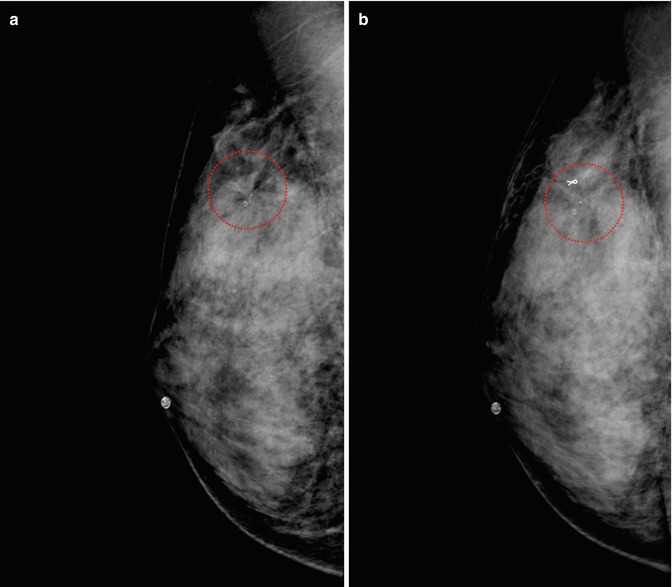
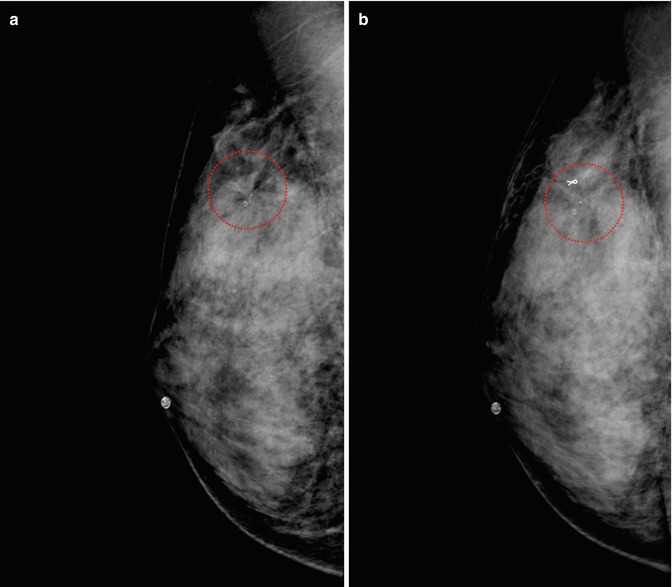
Fig. 5.6
Forty-three-year-old asymptomatic female presenting with an abnormal screening mammogram showing architectural distortion (circle) with radiating spicules (a). She underwent ultrasound-guided core needle biopsy with clip placement. Pathology from the core needle biopsy showed a radial scar (b) (Courtesy Dr Michael Cohen Emory University Atlanta)
The clinical significance of RSLs lies in both the implicit associated increase risk of developing breast cancer in the future and the associated risk of concurrent malignancy. The relative risk increase imparted by a diagnosis of RSL ranges from 1.8 to 3 [47, 48], and a diagnosis of associated malignancy following excision has been reported at a rate of 0–40 % [10]. Due to the similarities in clinical appearance to carcinoma and the potential risk of associated breast cancer, RSLs have traditionally been treated with excisional biopsy. The more recent literature showing percutaneous underestimation rates of malignancy in the 5–9 % range makes management more complex, with options for surveillance seeming more acceptable, particularly in higher operative risk or multiply-comorbid patients [15, 46]. The absence of cytologic atypia, increased number of cores taken at the time of CNB, and extensive sampling with vacuum-assisted needle biopsy have all been described as methods to identify patients that may safely be monitored. However, no clear clinical radiographic predictors have been identified to determine lesions at increased risk for associated malignancy, and surgical excision recommendations should be made independent of imaging findings [45]. For most patients of acceptable operative risk, optimal management continues to be complete surgical excision.
Fibroepithelial Lesions with Cellular Stroma
Fibroepithelial tumors of the breast represent a varied group of lesions containing both mesenchymal and epithelial components. The epithelial elements contain Ck5/14-positive progenitor cells with their glandular and myoepithelial progeny, whereas the stromal component shows vimentin/CD34 positivity with potential for multi-lineage differentiation as seen in spindle cell lesions of the breast [16, 17]. The proliferation of fibroepithelial elements along divergent pathways gives rise to fibroadenomas, phyllodes tumors, sclerosing lobular hyperplasia, and hamartomas.
Fibroadenoma is the most common benign breast tumor and clinically presents as a palpable mass or as an abnormal imaging finding. Lesions may be identified in women at any age, typically presenting during early adolescence, with a mean age of 30 at presentation. Multiple fibroadenomas can be identified at presentation approximately 15 % of the time. When palpable, fibroadenomas are typically small, smooth, mobile, and firm or rubbery masses with >90 % smaller than 4 cm. Fibroadenomas may develop into very large masses particularly in adolescent girls and young women, often called juvenile giant fibroadenomas (Fig. 5.7a, b) [49]. On mammography, fibroadenomas appear as well-defined round, oval, or lobulated masses, which may be calcified. On ultrasound, fibroadenomas are well-circumscribed, uniform hypoechoic or isoechoic ovoid masses, and the lesions are typically wider than tall with a well-demarcated margin [50].
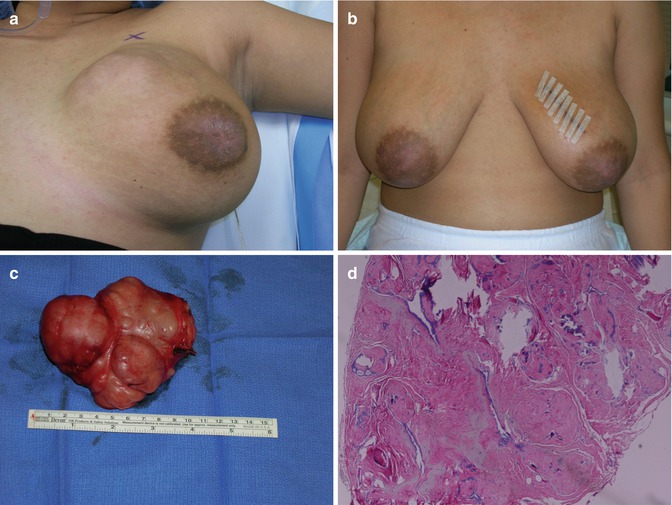
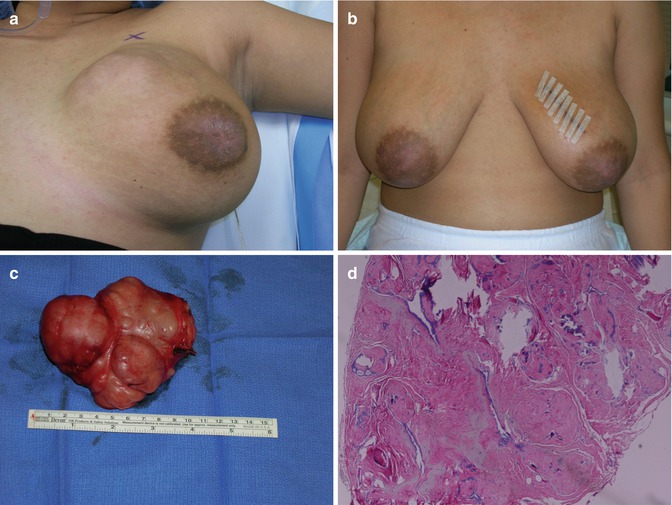
Fig. 5.7
Juvenile giant fibroadenoma of the breast. (a) Eighteen-year-old female at presentation. (b) One week after surgery. (c) Surgical specimen 12 × 11 × 8 cm. (d) Microscopically, the fibroadenoma showed mainly a hyalinized component (Courtesy of Monica Rizzo, MD and Marina Mosunjac, MD Emory University Atlanta)
Fibroadenomas arise from the epithelium and stroma of the terminal duct-lobular unit, with pathologic findings typically revealing well-defined borders consisting of elongated ducts lined with two layers of epithelium and situated in a stroma with low cellularity. When the diagnosis is made by CNB, a decision must be made whether to monitor or excise the lesion. In rare cases, fibroadenomas can progress in both epithelial and stromal directions to malignant tumors [51]. However, most fibroadenomas tend to be self-limited or even regress, and it is not necessary to remove them all, while percutaneous excisional or ablative treatment may be appropriate in select patients as defined recently by the ASBrS. Size (greater than 2.0–2.5 cm), growth, symptoms, positive family history, discordance, and age (greater than 35 years) are reasonable indications for surgical excision. It should be discussed that there is a potential for upgrade in the final pathologic diagnosis to a phyllodes tumor, in situ, or even invasive carcinoma in rare instances [51].
Phyllodes tumor is an exceedingly rare lesion with an estimated incidence of 2.1 per million women. Presentation typically occurs between the ages of 45 and 49, typically about 15 years later in age compared to fibroadenomas [52]. The presentation of a phyllodes tumor is clinically indistinguishable from that of a fibroadenoma [53]. Phyllodes tumor is felt to arise from the perilobular-periductal stroma. Microscopically, a circumscribed lesion with mixed epithelial and mesenchymal components is seen with a double-layered epithelial component and overgrowth of a hypercellular stromal component. FNA and CNB typically cannot discriminate between fibroadenoma and phyllodes tumor; however, the diagnosis may be suggested [54, 55]. Several systems for grading of phyllodes tumors exist, and while many authors use a three-tiered system to distinguish between benign, borderline, and malignant cases, others omit the intermediate category [56, 57].
A benign phyllodes tumor is characterized as having few mitoses in a high-power field (HPF), <2 per 10 HPF; no more than mild atypia, and no stromal overgrowth. Borderline phyllodes tumor has 2–5 mitoses per 10 HPF, more atypia with no stromal overgrowth. Malignant phyllodes tumor has marked atypia, more than 10 mitoses per HPF and stromal overgrowth (Fig. 5.8a, b). The grading system reflects the clinical behavior, with local recurrence and rare metastases noted in benign cases and distant metastases more common in malignant cases. When phyllodes tumor is diagnosed by CNB, the ability to differentiate benign, intermediate, and malignant lesions is unreliable [56]. Wide local excision with the intent of removing >1 cm margins is the preferred treatment of a phyllodes tumor (Fig. 5.9a, b). There is a relatively high incidence of local recurrence, reported from 8 to 46 % in cases of positive surgical margins [57]. Often, the diagnosis of phyllodes tumor is not made until excisional biopsy has been performed. When excising a fibroadenoma, removal of a rim of normal breast tissue around the lesion is acceptable, in case an upgrade in diagnosis to a phyllodes tumor does occur.