Fig. 14.1
Stage 1 osteonecrosis of edentulous mandible of a 73-year-old woman with osteoporosis treated with alendronate for 10 years. Note exposed bone on the lingual aspect of the mandible (blue arrow) and small fistula on the buccal aspect (black arrow)

Fig. 14.2
Stage 1 osteonecrosis showing exposed bone around lower premolar in right mandible (arrow) in a 81-year-old woman with osteoporosis treated with bisphosphonate for 51 months (48 months alendronate, 3 months Forsteo). She was treated by surgery including small local bone resection and removal of the tooth
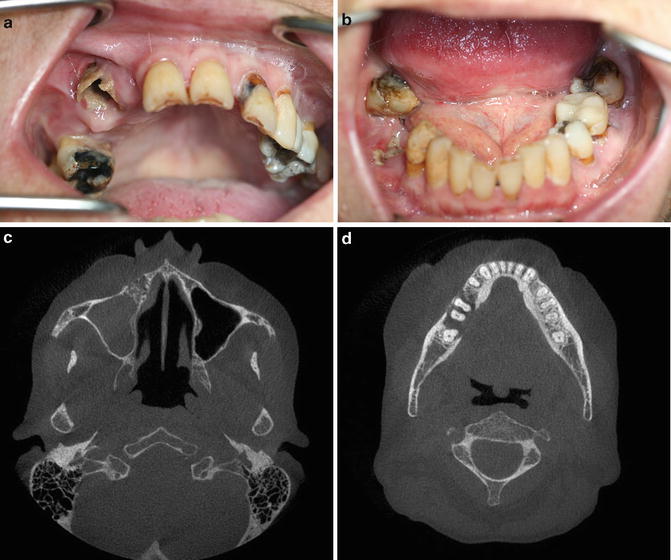
Fig. 14.3
Stage 3 osteonecrosis showing exposed bone in the maxilla and mandible in a 51-year-old woman with osteoporosis, chronic obstructive lung disease, alcohol problem, and liver disease. The patient had severe extraoral fistulas with pus secretion from the mandible. She had been treated with alendronate (36 months), aclasta (18 months), and denosumab (36 months) for a total of 90 months. Notice infection on right maxillary sinus. After hospitalization and feeding until sufficient weight (from 35 kg to 42 kg), she had a continuity resection done in the lower jaw and partial resection in the upper jaw. She became free of symptoms and was cured of her ONJ
Two thirds of ONJ lesions occur in the mandible, one third in the maxilla, and a small percentage occur in both jaws [13–15].
The presences of mandibular exostosis (tori) or maxillary exostosis (palatal tori) are risk locations for ONJ (Fig. 12.6). These cases are often spontaneously occurring. Another local risk area is the lingual aspect of the mandible at the wisdom tooth area, both in dentate and in edentulous patients. It is important to visually inspect these areas carefully, as the lesions are easily overlooked (Fig. 14.1).
When exposed bone after tooth extraction has been left without treatment, the necrotic lesion may expand and involve the neighboring teeth, which then usually cannot be saved (Fig. 14.3).
Another clinical presentation is lack of visible exposed bone but only a fistula, sometimes with pus coming out on pressure, on the alveolar process (Fig. 14.4a). These cases are so-called non-exposed ONJ . Other types of non-exposed ONJ are even more difficult to diagnose as there may be only pain and swelling but no exposed bone and no fistula. Useful imaging techniques in addition to radiograph include CT or cone beam scans and bone scintigraphy, sometimes combined with CT (SPECT–CT) (see Fig. 14.4). These patients should always have a dental examination, and a common periapical infection around a tooth should be excluded; see also diagnostic criteria of non-exposed ONJ (Table 13.2).
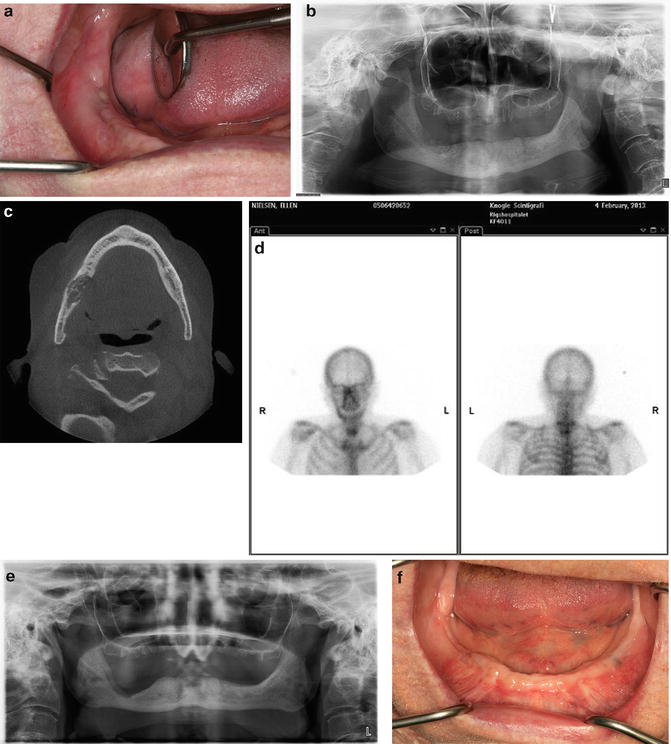
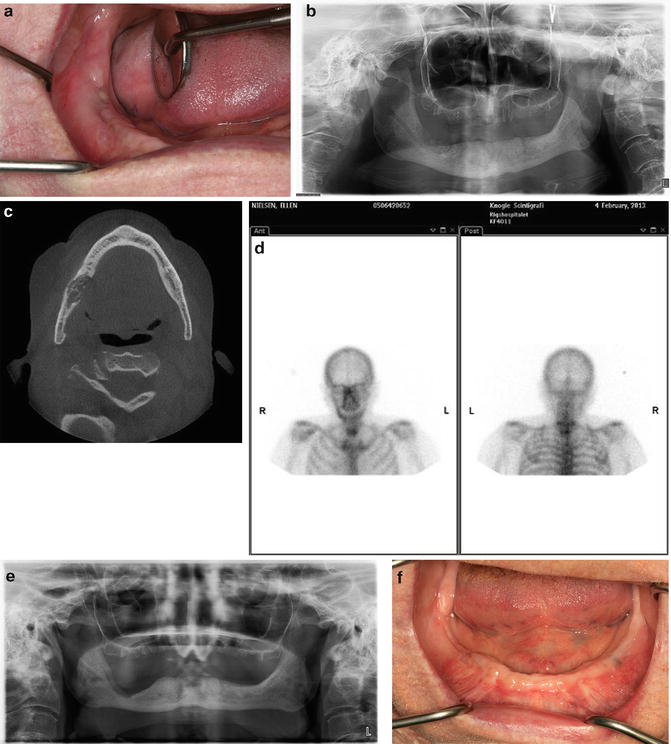
Fig. 14.4
(a) Stage 2—non-exposed type of osteonecrosis of the lower jaw in a 70-year-old woman with osteoporosis. She was treated with alendronate 70 mg/week p.o. for 3 years followed by aclasta i.v. yearly for 3 years, thus a total of 6 years of bisphosphonate treatment before onset of osteonecrosis. Notice the fistula with pus on the top of the alveolar process (arrow) in the lower right (edentulous) mandible. There is no exposed bone in the jaws. (b) Preoperative panoramic radiograph of the patient from Fig. 14.3a showing sequester in the alveolar process of right lower mandible (arrow). (c) Cone beam CT scan of the mandible of the patient shown in Fig. 14.3a. Notice the extensive necrotic area in the lower mandible extending through the lingual aspect of the jaw (arrow). The alveolar nerve was affected by the necrosis. (d) Scintigraphy of the jaws showing moderately increased signal in the right mandible. (e) Postoperative radiograph after block resection and removal of sequester in right mandible (arrow). (f) Postoperative healing. The patient was free of symptoms 1 week postoperatively and still without symptoms and without recurrence of osteonecrosis after 1.5 years observation time
A nonhealing socket after tooth extraction presenting with exposed bone is usually without symptoms or sign of infection in the beginning. Other lesions may start at the marginal bone around the tooth (Fig. 14.2). When symptoms and signs of infection occur the lesion is classified as stage 2; see Fig. 14.4.
Stage 3 (cf. Tables 13.1 and 13.2) refers to the advanced cases which are widespread, often with multiple sites of exposed bone (Fig. 14.3) and involvement of the maxillary sinus (Fig. 14.3b), in the mandible extending to the inferior nerve canal, showing extraoral fistula, or present with a spontaneous jaw fracture (see also below).
Severe Clinical Manifestations
These features only occur by definition in ONJ stage 3 (see Tables 13.1 and 13.2). A number of patients present with a cutaneous fistula as the first sign of ONJ. Fistulas may appear submandibularly or on the chin or cheek. Usually, but not always, fistulas are associated with severe bone exposure intraorally. A submandibular or intraoral abscess as sign of acute infection is another manifestation, which is rarely the first symptom, but during long-term course may occur in 30 % of the cases [13] and thus quite common. There may be varying degree of suppuration from the fistulas. Cutaneous fistulas occur in 5–10 % of ONJ cases [13, 15].
Paresthesia, numbness, or hyposensation of the lower lip indicating mandibular alveolar nerve involvement occur in around 11 % of ONJ at initial examination [13]. During operation, necrosis of the bone surrounding the nerve is often evident. Spontaneous fracture of the mandible is rarely seen (3–4 %) [13, 16]. Severe ONJ lesions of the maxilla often involve the maxillary sinus (Fig. 14.3c).
Imaging of ONJ
The imaging of ONJ has improved during the last decade (see also Chap. 12). The traditional orthopantomograph is the basis of imaging of the jaws. However, most patients will have a CT scan or cone beam scan of the jaws. Bone scintigraphy is useful, either the traditional type or combined as SPECT–CT or PET–CT. MR scans may have value evaluating the soft tissue changes including suspected abscesses, and other types of imaging will most likely find its way to the diagnostic tools [17, 18]. None of the imaging methods can stand alone. ONJ is still a clinical diagnosis, and it is not expected that imaging will be the gold standard of diagnosis in the near future. However, imaging is tremendously important for evaluating a given ONJ lesion and for the planning of treatment as well as for monitoring natural history and treatment results.
Radiographs
The reader is also referred to Chap. 12. First, ONJ lesions may present on orthopantomograph in several ways. The typical sequester is a demarcated area of radiopaque or normally looking (dead) bone surrounded by an osteolytic zone (Fig. 14.4b). In patients who have had a tooth extracted, the dental socket is not healing within half a year as in normal patients but may stay open for months to years after extraction. This is the effect of the bisphosphonate reducing the remodeling of the bone. A characteristic sign of long-term bisphosphonate treatment is the thickening of the lamina dura surrounding the teeth. The widening of lamina dura is not a sign of ONJ but only indicates the long-term effect of bisphosphonate and places the patient in the “at-risk” classification (Table 13.1). Other manifestations are radiopacities, either focally or more widespread.
Often a mix of radiolucent and radiopaque areas is seen, which may in fact be necrotic. In these cases, additional imaging in the form of a CT scan or cone beam scan should be considered mandatory.
CT Scans
CT scans including cone beam scans give the possibility to map the osteonecrosis in detail including evaluating the involvement of mandibular alveolar canal and the maxillary sinus (Fig. 14.3).
Scintigraphy
Bone scintigraphy utilizing a radioactive technetium tracer alone or combined with CT scans (SPECT–SCAN) may map the extent of the lesions. Often, there is a good correlation between the clinical and radiographic features of a given ONJ lesion (Fig. 14.4d). As the tracer depends on active bone formation, the signal is almost certainly due to the periosteal reaction of the ONJ lesion and is thus not a feature of the dead bone itself. This may also explain why some patients show little signal on scintigraphy. The importance of the scintigraphy is that lesions extending further than the clinical or radiologic lesion may be identified [18].
Pathogenesis of ONJ
The pathogenesis of ONJ is complex and partly unknown (see also Chap. 12). Most likely, the onset of ONJ is based on a multifactorial combination of local and systemic risk factors.
Bisphosphonate and denosumab, although acting through different pathways, both lead to a reduced remodeling of the skeletal bones and increased bone mineral content. The pathogenesis may involve a changed turnover of bone modeling, different response of osteoclasts to cytokine stimuli, as well as genetic factors [19, 20].
It is noticeable that tooth extractions or other oral surgical procedures precede the onset of ONJ in a high proportion (50–75 %) of the cases [13, 21]. However, it has been proposed that it is the infection that leads to the tooth extraction rather than the tooth extraction itself, which may be of importance [12, 16, 21, 22]. Cell culture experiments seem to indicate that the acidic environment in infectious areas as well as release of free BP might be of importance [12]. Epithelial healing following oral ulceration decreased due to alendronate in BP treatment [23].
Histopathology of ONJ
The pathology of affected ONJ specimens shows bone necrosis with loss of osteocyte nuclei. Osteocyte lacunae are empty, and the haversian channels reveal necrotic tissue. The jaw bone marrow spaces are necrotic, sometimes showing signs of active infection with pus, i.e. neutrophils and other inflammatory cells (Fig. 14.5). The exposed bone surface is commonly covered with bacteria and colonies of actinomyces colonies, which also may occur in the central bone marrow areas. Operation specimens may show varying degree of necrosis with some vital bone cells or bone marrow at the periphery, indicating a periosteal reaction [25]. Resection specimens may show a considerable periosteal reactive new bone formation on the surface of the central necro tic bone tissue [25].
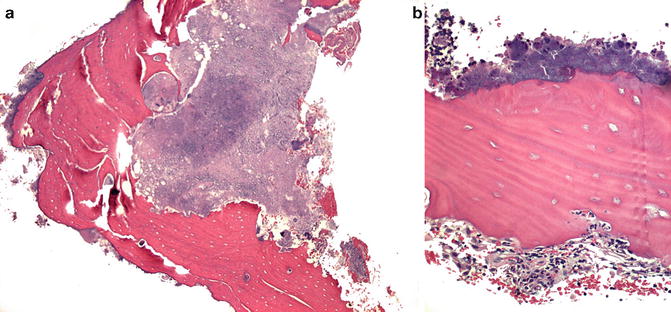
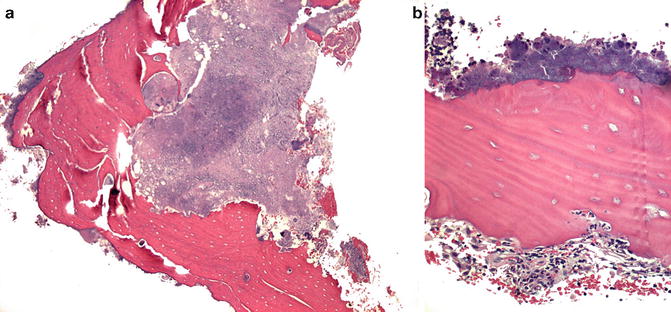
Fig. 14.5




(a) Sequester removed from osteonecrosis lesion of the jaw. Notice bacteria on the surface to the left. The bone marrow is replaced with inflammatory cells, necrotic tissue, and bacteria. (b) High power of histology of sequester removed from the jaws showing dead bone with bacteria on the surface. The osteocyte lacunae are empty and in the marrow space inflammatory cells and erythrocytes are seen (Photos courtesy of Dr. Jesper Reibel, Department of Odontology, University of Copenhagen, Denmark)
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree






