Malignant Bone Lesions
Francis R. Patterson
Timothy A. Damron
Carol D. Morris
Malignancies involving bone include metastatic disease, myeloma, lymphoma, and bone sarcoma. Treatment options include surgery, radiotherapy, and chemotherapy. This chapter will focus on the treatment principles involved in choosing the appropriate surgical treatment along with appropriate adjuvant radiotherapy and/or chemotherapy according to the diagnosis.
Surgical Treatment
Surgical Indications/Contraindications
Indications for surgical intervention of bone malignancies vary according to the underlying disease process (Table 4.3-1).
Biopsy for diagnosis
Indications: plays a role in diagnosing nearly all bone malignancies, although multiple myeloma may often be diagnosed by serum or urine protein electrophoresis (SPEP or UPEP).
Prophylactic stabilization
Indications: Impending pathologic fractures merit prophylactic fixation in many cases of metastatic disease, myeloma, and lymphoma.
Contraindications: Except in unusual circumstances, bone sarcomas should be treated by wide excision, as instrumentation will potentially disseminate tumor locally and possibly systemically.
Open reduction and internal fixation (ORIF) pathologic fractures
Same as for prophylactic stabilization
Extended intralesional curettage with adjuncts
Indication: low-grade chondrosarcomas without soft tissue extension (as an alternative to wide resection)
Contraindication: more aggressive-appearing chondrosarcomas (soft tissue extension and/or intermediate or high grade), all other bone sarcomas
Resection for extensive destruction
Indications: Extensive symptomatic bony destruction that is not amenable to stabilization may warrant resection and reconstruction in the setting of metastatic disease, myeloma, and lymphoma.
Especially proximal femur and proximal humerus
Endoprosthetic reconstructions favored
Appropriate surgical margins range from intralesional to marginal or wide in this situation, as resection is not for cure.
Contraindications: When internal fixation will suffice in metastatic disease, myeloma, and lymphoma, ORIF is preferred.
Resection for cure
Indications
Solitary bone metastases (Box 4.3-1)
Most bone sarcomas (except intraosseous low-grade chondrosarcomas)
Resection of major segments of bone should not be undertaken without considering (1) whether limb-sparing surgery or amputation should be done, (2) whether reconstruction will be needed for the defect left after limb-sparing surgery, and (3) what reconstructive options should be considered.
Table 4.3-1 Roles for Surgical Treatment According to Disease Process | |||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
Limb Salvage Versus Amputation
The most important goal of the surgical treatment of bone sarcoma is complete resection of the tumor with a wide margin. Maximizing function and salvaging the limb are secondary but important considerations in surgical planning. The decision to perform limb salvage versus amputation is dependent on several factors.
Indications for Limb-Sparing Surgery
Wide resection (complete resection of the tumor) must be attainable.
Function of the salvaged limb must be at least as good as the function of the limb after amputation at the appropriate level required for complete tumor resection (Fig. 4.3-1).
Reconstructed limb must be stable and durable.
There must be adequate skin and soft tissue after resection of the tumor to allow for coverage of the limb/reconstruction.
Local rotation of tissues and the use of free tissue transfer have broadened the indications for limb salvage.
Usually major neurovascular bundles must not be involved or surrounded by tumor.
Box 4.3-1 Diagnoses for Which Resection of a Solitary Bone Metastasis may be Considered for Oncologic Purposes
Renal carcinoma
Thyroid carcinoma
Bone sarcoma
Soft tissue sarcoma
Evaluation and Management of Possible Neurovascular Involvement
Magnetic resonance imaging (MRI) is the gold standard for imaging to determine the relationship of the tumor to the surrounding structures.
Major vessel resection en bloc with the sarcoma and reconstruction with vein graft or artificial vessel graft is possible.
Resection of major nerves is allowable as long as the predicted function of the limb is at least as good as an amputation with prosthesis.
Upper extremity: As a general rule, any function saved is better than an amputation
Lower extremity
Patients without a sciatic nerve can walk; may require ankle–foot orthosis (AFO) and/or assistive device.
Femoral nerve resection/loss of extensor mechanism is not an indication for amputation, as patients can walk without active knee extension.
Relative Contraindications to Limb Salvage
Displaced pathologic fracture, due to tumor contamination throughout extent of fracture hematoma
Not absolute, as there is literature to support limb salvage after pathologic fracture if there is a good response to chemotherapy and the fracture heals
Misplaced biopsy site or prior “nononcologic” procedure performed with contamination of surrounding tissues
Reconstruction of limb not possible to allow function equivalent to an amputation
Poor response to chemotherapy
Vital neurovascular structures encased by tumor and not reconstructible or amenable to bypass
Amputation
Primary goal of amputation, like limb salvage surgery, is to resect the entire tumor with adequate “wide” margins.
Secondary goals of amputation are functional:
Must result in a stump that will allow for fitting of a prosthesis
Prosthetic fitting and rehabilitation is an important part of recovery and can be difficult while patient is still undergoing postoperative chemotherapy.
Risk of surgical complications is lower than for limb-sparing surgery.
Sometimes required after failed limb salvage attempts (e.g., infection, prosthesis failure, fracture)
Expendable Bone
After determining that limb-sparing surgery is indicated, the decision of whether to reconstruct or not must be weighed next. The specific sites of bone that are generally considered expendable, and therefore not in need of reconstruction, are those listed.
Fibula: usually no bony reconstruction required (lateral collateral ligament [LCL] stabilization proximally or augmentation distally is sometimes required)
Iliac wing: when acetabulum not involved (some surgeons advocate reconstruction to restore pelvic continuity)
Pubis: if hip joint maintained, no bone reconstruction of inferior pelvis usually necessary
Rib: no bone reconstruction necessary
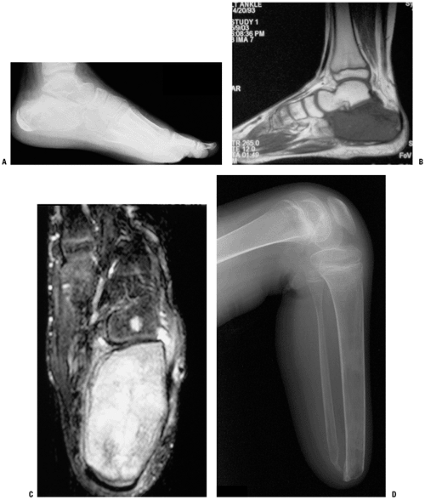
Distal ulna: no bone reconstruction is necessary, but soft tissue repair of the triangular fibrocartilage is recommended (Fig. 4.3-2)
Limb Reconstruction
Generalities of Available Options
There are several options for reconstructing skeletal defects after resection of malignant or aggressive benign bone tumors. Each has inherent advantages and disadvantages, and these should be considered when planning limb salvage surgery. The seven “A’s” of limb reconstruction are:
Amputation
Autograft
Arthrodesis
Allograft
Arthroplasty
Allograft-prosthetic composites (APC)
Alternative reconstructions
Amputation (see Fig. 4.3-1)
Advantages
Lowest complication rate
Least chance of requiring reoperation for failure of reconstruction
Disadvantages
Body image issues
Function of upper extremity or proximal lower extremity may be fair to poor.
Autograft (Fig. 4.3-3)
Vascularized (e.g., free fibula) or nonvascularized (iliac crest, rib, fibula)
Advantages
“Normal” bone
Durable reconstruction
No risk of disease transmission
Disadvantages
Limited by size of defect and amount of bone available
Additional morbidity from donor site
Risk of cross-contamination (small)
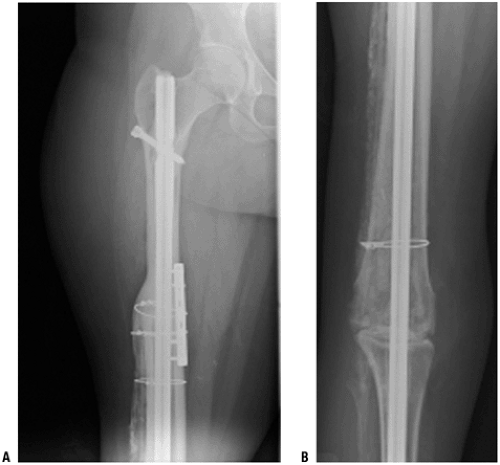
Arthrodesis: Fusion of Bone With Elimination of Joint (Fig. 4.3-4)
Advantages
Stable reconstruction after union
No need for revision/repeat surgery after union
Disadvantages: does not allow immediate function/weight bearing, may require additional bone graft (auto- or allograft), delayed union/nonunion rates can be high depending on site
Allograft
Supplied by “bone bank”: sterilization with or without radiation (weakens), processing required for storage and transplantation
“Rejection” of transplanted bone does not occur, but role of “histocompatibility” is currently being evaluated.
Intercalary: segment of bone between joints maintained; host joint surfaces maintained; cylinder versus hemi-cylinder (Fig. 4.3-5)
Osteoarticular: articular surface of allograft used to reconstruct at least part of the joint surface (Fig. 4.3-6)
Advantages
Stable reconstruction after union
Not limited by size of reconstruction required
No donor morbidity
Disadvantages
Infection up to 20%
Nonunion/delayed union of host–graft junctions up to 20%
Fracture of allograft up to 15% to 20%
Disease transmission possible
Size of allograft needs to be matched to host.
Arthroplasty
Usually by “megaprostheses”; modular endoprosthesis that can replace segments of bone and adjacent joint(s) (Fig. 4.3-7)
Advantages
Stable reconstruction that usually allows early weight bearing
Implant failure short term is low (less than fracture, nonunion of allograft)
No disease transmission
Size of reconstruction less of a problem (e.g., “total femur” and variable sizing of implant possible)
Disadvantages
Will likely require (several) revisions over lifetime
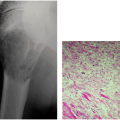
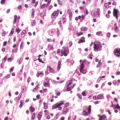
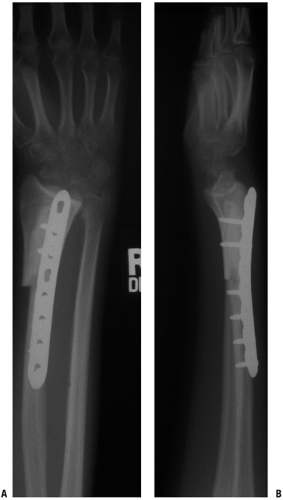 Figure 4.3-6 Following resection of a giant cell tumor of the distal radius, this patient underwent reconstruction using a distal radius osteoarticular allograft. |
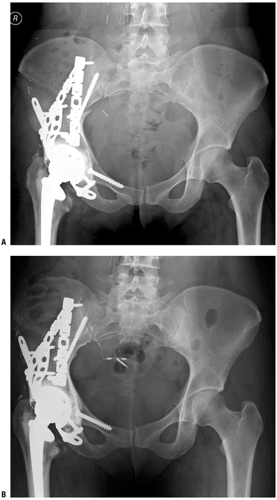
Allograft-Prosthetic Composite (APC)
Combines segmental reconstruction of bone with allograft and joint surface reconstruction with more standard arthroplasty (cemented) components (Fig. 4.3-8)
Advantages
May allow for better soft tissue (tendon) attachment about the joint and therefore more stability (e.g., host rotator cuff to proximal humeral APC or host patellar tendon to proximal tibial APC or host gluteus medius tendon to proximal femoral APC)
Some surgeons believe this allows better function of that joint (controversial).
Disadvantages
Technically more difficult
All the risks of allograft and arthroplasty combined, though stems of prosthesis should cross host allograft junction to make nonunion and fracture less of a clinical problem
Disease transmission
Alternative Reconstructions
Site-specific options may have advantages over other types of reconstructions.
Rotationplasty: for resections about the knee (Fig. 4.3-9)
Single-bone forearm after radial/ulnar tumor resection (Fig. 4.3-10)
Bone transport/limb lengthening
Physeal distraction in children
Reconstruction in the Growing Child
Since bone sarcomas can occur at ages where there is more bone growth left, resection of bone can result in significant leg length discrepancies. This needs to be considered in the treatment of these young patients. One indication for amputation is significant limb length inequality after treatment. However, options do exist for limb salvage surgery in growing children:
Expandable prostheses can be “lengthened” as the child grows (Fig. 4.3-11).
Rotationplasty requires preoperative planning to achieve both knees being at same level at skeletal maturity (see Fig. 4.3-9).
Limb lengthening after treatment (e.g., bone transport or Ilizarov technique)
Claviculo-pro-humero (autograft clavicle used to replace proximal humerus)
Proximal fibular autograft
Location-Specific Reconstructive Options
There are unique anatomic considerations to each site of bone tumor resection. Those, along with the reconstructive options, are discussed below.
Scapula (Fig. 4.3-12)
Many patients with scapular bone sarcomas undergo resection without reconstruction, but scapular endoprostheses are available; proponents cite improved functional outcome through lateralization of the shoulder joint.
Unique anatomic considerations
Soft tissue extent determines feasibility of scapular endoprosthetic reconstruction.
Reconstructive options
Flail shoulder reconstruction
Scapular endoprostheses (see Fig. 4.3-12)
Need rhomboids, trapezius, latissimus dorsi, serratus anterior, some of rotator cuff
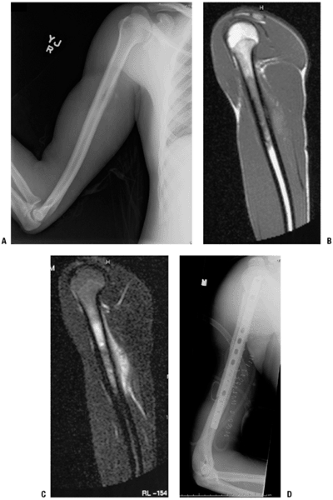
Proximal Humerus (Figs. 4.3-13 and 4.3-14)
Unique anatomic considerations
Intra-articular involvement
Some surgeons feel the shoulder joint should be routinely resected en bloc with the proximal humerus due to a purported high incidence of intra-articular tumor extension.
Many surgeons feel the resection should be based upon individual radiographic assessment.
Rotator cuff tendon insertion at tuberosities
Any resection of the proximal humerus entails sacrifice of the native rotator cuff attachments, and only osteoarticular allograft and allograft prosthetic composite reconstructions allow the potential for suturing of the host tendons to the reconstruction.
Axillary nerve and deltoid muscle insertion at deltoid tuberosity
Axillary nerve and/or deltoid muscle resection is sometimes needed for tumor resection based upon soft tissue extension.
Without the axillary nerve and/or deltoid function, the best reconstructive options are arthrodesis or proximal humeral spacer.
If axillary nerve and deltoid function can be preserved, mobile reconstructive options (osteoarticular allograft, allograft prosthetic composite, and megaprosthesis) are viable alternatives.
Glenohumeral joint stability
Reconstructive options (Table 4.3-2)
Osteoarticular allograft
Allograft prosthetic composite (see Fig. 4.3-13)
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree