Fibrous Lesions of Bone
Sung Wook Seo
Young Lae Moon
Francis Young-In Lee
Considerable controversy exists with respect to the terminology for fibrous lesions of bone. Although nonossifying fibromas (NOFs) and metaphyseal fibrous cortical defects (FCDs) are the most common lesions of bone, the current World Health Organization does not even include them in their classification, as they are not neoplastic (Box 5.5-1). Avulsive cortical irregularity has identical histology but is distinguished by a very specific location, the posteromedial distal femoral metaphysis. Benign fibrous histiocytoma, for which there are several synonyms, also has the same histology as NOF/FCD but is distinguished by its occurrence in older ages, in an atypical non–long bone location, with atypical radiographic appearance, or with unusual clinical presentation. Fibrous dysplasia and osteofibrous dysplasia have typical clinical presentations and radiographic appearances. Desmoplastic fibroma is a rare tumor that occurs most commonly in the mandible.
Box 5.5-1 Current Terminology for Fibrous Lesions of Bone
|
Nonossifying Fibroma, Metaphyseal Fibrous Cortical Defect, and Avulsive Cortical Irregularity
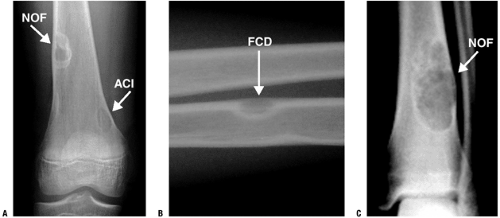
NOFs and their smaller counterparts, metaphyseal FCDs, are among the most common lesions of bones, particularly in children. Avulsive cortical irregularity (ACI) is a clinically distinct entity that shares the same histology but occurs only at the distal femoral posteromedial metaphysis. Each of these is most often discovered incidentally on radiographs obtained for other purposes, such as the evaluation of injuries about the knee. Their clinical presentations as incidental findings and their radiographic appearance of geographic, eccentric, radiolucent, partially intracortical lesions with a soap-bubble appearance are so characteristic that biopsy is usually unnecessary to establish the diagnosis. Their natural history of resolution over time strongly favors nonoperative treatment in most cases.
Pathogenesis
Etiology
NOF/FCD: focally defective periosteal cortical bone development leads to failure of ossification (developmental defect)
ACI: traumatic stress of avulsive microfracture, healing, and repeat avulsive fracture related to origin of medial head of gastrocnemius muscle and/or distal adductor magnus insertion on posteromedial cortical surface of distal femur only
Epidemiology
Incidence: true incidence unknown
NOF/FCD
NOF/FCD most common bone lesion(s) overall
Up to 40% of children with knee radiographs have one or more.
ACI
On x-ray, 10% to 40%, but on MRI up to 60%
Age: 3 to 20 for all three lesions (peak 10 to 15), with some NOFs and ACIs persisting into adulthood
Male:female 2 to 3:1 (both NOF/FCD and ACI)
Location
NOF/FCD
Long bone metaphyses predominate.
55% around knee
Distal femur > proximal tibia > distal tibia
Diaphyseal lesions and flat bones less common
ACI: By definition, these occur only in the posteromedial distal femoral metaphysis and are frequently bilateral.
Pathophysiology
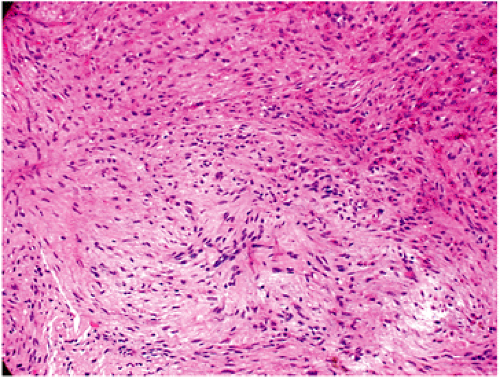
Pathology (Fig. 5.5-1)
Fibrous tissues arranged in storiform or cartwheel pattern with foamy histiocytes (30% to 50%, more frequent in adults), hemosiderin (variable), occasional multinucleated giant cells
Natural History
All of these lesions usually regress after skeletal maturity at the latest, sometimes sooner.
Most FCDs resolve without residual radiographic evidence, but some progress to NOF size.
Some lesions persisting into adulthood become latent or eventually ossify.
Assessing fracture risk
>50% of diameter of bone on both anteroposterior and lateral radiographs
>33 mm vertical dimension in nonfibular lesions
Distal tibial lesions most common site with associated fracture
Classification
NOF vs. FCD
FCD: typically small (<0.5 cm) radiolucency completely within the cortical bone
NOF: involves cortex but also extends into medullary bone
Some authors use a 3-cm size delineation.
ACI: posteromedial distal femoral metaphyseal lesion
Jaffe-Campanacci syndrome
Forme fruste of type I peripheral neurofibromatosis
Key components: multiple NOFs and café-au-lait spots
Variably associated: mental retardation, hypogonadism or cryptorchidism, ocular abnormality, cardiovascular malformations
NOF in neurofibromatosis type I (NF-1)
Most common bone lesion of NF-1
Diagnosis
Physical Examination and History
Most common clinical presentation: incidental asymptomatic finding
Other scenarios
Pathologic fracture with larger NOF
Usually not preceded by pain
Pain associated with lesions
Uncommon in FCD/NOF
Occurs more frequently with ACI but dissipates over time
Search for another source of pain.
Consider chondromyxoid fibroma, periosteal chondroma, and osteomyelitis in differential diagnosis for symptomatic lesions.
Radiographic Features
Plain Radiographs (Fig. 5.5-2)
Usually diagnostic in vast majority of cases
Well-marginated (geographic), eccentric, partially intracortical, multiloculated, soap-bubble radiolucent lesion with a sclerotic rim
May be central within smaller bones such as fibula but still partially intracortical
Occasional cortical thinning and expansion
ACI best visualized on oblique radiographs; often bilateral
Magnetic Resonance Imaging
Indicated for atypical plain film features, symptoms, or older patients
FCD: fibrous signal void within cortex, dark on T1-weighted but brighter on T2-weighted
NOF
Low-signal (dark) central region on both T1- and T2-weighted sequences due to hemosiderin and/or dense collagen
Typically no surrounding edema in absence of pathologic fracture
ACI: variable manifestations, including discrete lesions and simple irregularity of the posteromedial cortex
Bone Scan
Minimal to no uptake seen; bone scan usually not needed
Treatment
Observation: treatment of choice for essentially all FCDs and ACIs and the vast majority of NOFs
Open biopsy: atypical radiographic appearance, symptomatic lesions, and lesions in adults for which the diagnosis cannot be established by clinical and radiographic presentation (unusual)
Curettage and grafting with or without internal fixation: usually reserved for larger lesions after fracture (see fracture risk above) or in very active patients
Results and Outcomes
Local recurrence is nearly nonexistent for completely curetted NOF.
Peripheral radiolucencies may indicate residual NOF tissue.
Benign Fibrous Histiocytoma of Bone
This rare neoplasm is the prototypical fibrohistiocytic benign tumor within the World Health Organization classification schema. Its importance lies in its distinction from the more common NOF, so this section will contrast the features of this lesion with NOF.
Pathogenesis
Etiology
Unknown
Epidemiology
Incidence: rare
Age: 6 to 74 years (60% are above typical upper age limit for NOF)
Unlike NOF, female > male preponderance (slight)
Location
Any bone may be affected.
Like NOF, femur and tibia are most common, BUT diaphyseal or epiphyseal regions predominate in long bones (unlike metaphysis for NOF).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree