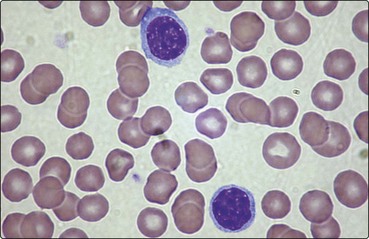
4 Most mature lymphocytes appear under the light microscope as cells with round nuclei and a thin rim of agranular cytoplasm (Fig 4.1). Although B- and T-cells are not distinguishable by their morphology, there are major differences in their mode of maturation and function. T-cells make up 75% of the lymphocytes of the blood and form the basis of cell-mediated immunity. They are less autonomous than their B-cell companions, needing the cooperation of antigen-presenting cells expressing self-histocompatibility molecules (human leucocyte antigens (HLA)) for the recognition of the antigen by the T-cell receptor (TCR) (Fig 4.2). Fig 4.2 Interaction of T-lymphocyte and antigen-presenting cells. T-cells originate in the marrow but many are destroyed in subsequent processing by the thymus, the objective being to select the minority of cells which will recognise self-HLA but not react with self-tissue antigens. The maturation sequence is characterised by changing patterns of cell surface molecules (Fig 4.3). Mature T-cells are divisible into two basic types. About two-thirds of blood T-cells are ‘helper’ cells expressing the surface marker CD4, while the remainder express CD8 and are mostly of ‘cytotoxic’ type. Fig 4.3 Maturation of B- and T-lymphocytes. It appears that helper cells recognise the combination of antigen and self-HLA class II molecules on the antigen-presenting cell, and cytotoxic cells bind with antigen in conjunction with HLA class I molecules on the target cell (Fig 4.2
Lymphocytes
T-lymphocytes
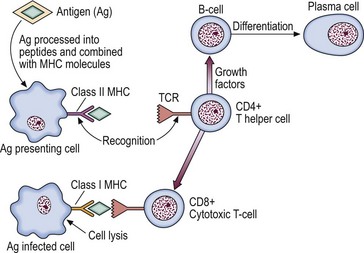
The T-cell receptor complex (TCR) recognises the combination of processed antigen and major histocompatibility complex (MHC) molecule and the immune response is initiated.
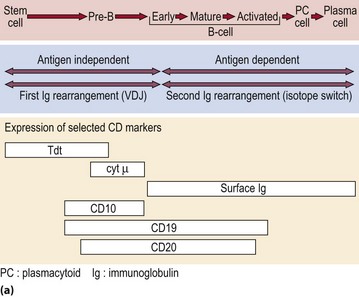
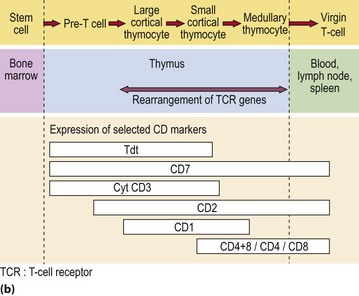
(a) B-lymphocyte maturation in the bone marrow. (b) T-lymphocyte development in the bone marrow and thymus.
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Oncohema Key
Fastest Oncology & Hematology Insight Engine