Lobectomy
CRITICAL ELEMENTS
Patient Selection for Lobectomy
Patient Selection for Bilobectomy or Other Advanced Lung Resection
1. PATIENT SELECTION FOR LOBECTOMY
Recommendation: Lobectomy is the preferred treatment for patients with resectable lung cancer.
Type of Data: Prospective.
Strength of Recommendation: Strong.
Rationale
Lobectomy remains the preferred surgery for the resection of lung cancer with curative intent, despite the fact that segmentectomy is increasingly being considered for such resection. Although its findings are being challenged in an ongoing major clinical trial, the original Lung Cancer Study Group trial demonstrated that the local recurrence rate of patients who underwent sublobar resection was three times that of patients who underwent lobectomy and that sublobar resection patients had a 50% higher rate of death with cancer compared with lobectomy patients.1,2
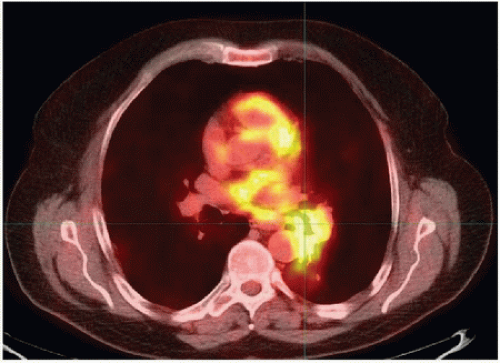
The primary contraindications to simple lobectomy are tumor and/or hilar nodal invasion at the origin of the lobar bronchus (Fig. 11-1), which precludes obtaining a negative surgical margin with bronchial division, and tumor and/or hilar nodal invasion of the lobar or main pulmonary arteries.
Bronchoscopy and careful review of contrast-enhanced chest computed tomography (CT) findings are imperative to identify central tumors that may involve major airway or vascular structures within the hilum and thus preclude lobectomy.
Intraoperative Technical Suggestions
Anatomic lobectomy is based on the individual dissection, ligation, and division of the lobar pulmonary arteries and venous branches to the lobe. The order in which these structures are divided often depends on the lobe being resected and/or the surgeon’s preferred technique.
The branch points of the pulmonary artery offer an opportunity to meticulously dissect intra- and interlobar N1 nodal stations. Although published guidelines recommend that level 10 nodes be dissected, we believe that it is good practice to identify and separately dissect other N1 stations to more accurately stage the disease.1,3 One recent study indicated that the presence of extralobar N1 disease (stations 10 and 11) predicts worse prognosis than does the presence of intralobar N1 disease (stations 12 to 14).4 Dissecting the hilar lymph nodes (levels 10, 11, and 12), which exposes the hilar structures prior to their division, is extremely helpful during lobectomy. Following vascular division, the lobar bronchus or bronchi should be discreetly dissected, divided, and closed grossly free of tumor.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree