Introduction
Atherosclerosis is a disease of ageing. Cardiovascular event rates increase in a curvilinear fashion after age 65 years in men and 75 years in women.1, 2 The decline in age-standardized cardiovascular disease (CVD)-associated death rates has shifted mortality to increasingly advanced age, with the number of cardiovascular events in those aged >80 years having increased by 60% since 1970.3 Numerous epidemiological studies have shown that age is the principal unmodifiable risk factor for events.4–6 Both diabetes and hypertension are strongly age-related risk factors.7 In parallel with these risk factors levels of total cholesterol rise with age especially after middle age or the menopause. The increasing incidence of metabolic syndrome and obesity with age means that high density lipoprotein cholesterol (HDL-C) levels tend to fall and triglyceride levels rise.8 Thus hyperlipidaemia is an increasing risk factor for coronary events, aortic valve disease, stroke, peripheral vascular disease including abdominal aortic aneurysm and possibly dementia (multi-infarct type). As many elderly patients have suffered one cardiovascular event they are at high risk of another, often in a different vascular bed. Thus patients with strokes more often have coronary events than second strokes.
As life expectancy increases, preventive efforts will become increasingly important for preventing morbidity, improving quality of life (QOL), and reducing healthcare expenditures for older persons. Clinicians need to consider additional factors in the elderly which most often are not applicable in younger individuals when faced with treatment decisions. These include co-morbid conditions, polypharmacy, drug–drug interactions and differential safety and tolerability profiles; all of which could lead to alterations in the benefit-harm balance. This highlights the importance of considering both the treatment options and the evidence for their use in the elderly population.
Cholesterol in the Elderly
Ageing is associated with a progressive increase in cholesterol levels in men and in many women profound changes in lipids follow the menopause with substantial increases in low density lipoprotein cholesterol (LDL-C) secondary to possibly changes in proprotein convertase subtilisin kexin-9 (PCSK-9) levels which are under the control of sex steroids and a reduction in HDL-C most probably caused by changes in sex steroids.9 However, most hyperlipidaemia in the elderly is still caused by dietary and lifestyle choices. The slowly declining metabolic rate of the elderly, associated with reduced levels of activity due to concurrent ageing or osteological problems means that many show features of the metabolic syndrome. Dietary conservatism also tends to mean that currently the elderly are less likely to consume a diet rich in fruit and vegetables and are more likely to eat a diet rich in saturated fat.
Secondary causes of hyperlipidaemia are more common in the elderly. The most common cause of mixed hyperlipidaemia is insulin resistance and/or type 2 diabetes. Rates of chronic renal disease also increase in the elderly, which allied to greater arterial stiffness, result in increases in pulse pressure, isolated systolic hypertension and secondary cardiovascular risk. Other causes that tend to be associated with ageing include alcohol-induced hyperlipidaemia which is more commonly due to a reduction in liver-related detoxification in the elderly and its frequent association with depression, especially in single men. Alcohol-induced hyperlipidaemia may show a profile varying between mixed hyperlipidaemia to pure hypercholesterolaemia depending on the frequency of alcohol intake. Non-alcoholic steatitic hepatitis, which is often associated with a mixed hyperlipidaemia, is more common in the centrally obese elderly.
The most common cause of pure secondary hypercholesterolaemia is hypothyroidism. The significance of this is that prescription of a lipid-lowering drug to a grossly hypothyroid patient massively increases their risk of drug-associated rhabdomyolysis.
However, despite these factors the positive association between total and LDL-C and cardiovascular risk attenuates with advancing age.10 In epidemiological studies a 1 mmol l−1 lower total cholesterol (TC) is associated with approximately 50% reduction in coronary heart disease (CHD) mortality in patients aged 40–49 years, 33% in those aged 50–69 and 15% in those aged 70–89 years.11 Yet, though the relative risk reduction associated with lower cholesterol decreases with age, the absolute effects of lower cholesterol on annual ischaemic heart disease mortality rates are greater in the elderly given the higher prevalence of atheroma. Also cholesterol levels decline in acute and chronic disease states, inflammation, malnutrition and cancer, all of which are more common in the elderly and thus this attenuated association may be partly due to confounding.12
Clinical Signs
Clinical signs present differently in the elderly. Arcus senilis is associated with familial hypercholesterolaemia in the young but not in the elderly. Xanthelasma are associated with mixed dyslipidaemia and reduced skin thickness and elasticity and thus are more common in older individuals. Tendon xanthomata may be confused with gout tophi or Heberden’s nodes which are common in the elderly but may be clinically distinguished by their movement with the underlying tendon.
Lipoproteins and Their Measurement
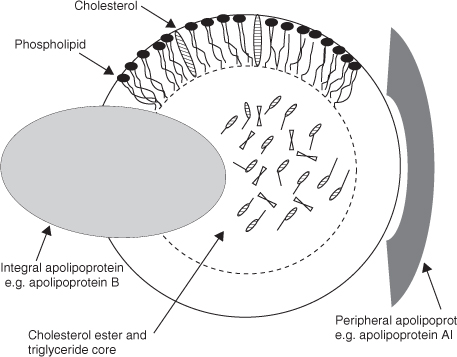
Blood lipids are transported in macromolecular complexes called lipoproteins. Figure 38.1 shows a schematic representation of these complex molecules. Their function is to transport triglycerides (energy) and fat soluble vitamins to sites of storage or metabolism, the principal function of the apolipoprotein B group (chylomicrons, very low density lipoprotein, low density lipoprotein (LDL)). They also function to detoxify lipopolysaccharide toxins and remove potentially toxic fatty acid metabolites—principally through reverse transport by apolipoprotein A-1 containing high density lipoproteins (HDLs). Blood lipids are most often measured either as TC, LDL, HDL as well as plasma total triglyceride (TG) components. Only the cholesterol fraction (-C) of the major lipoprotein fractions is measured routinely and the concentrations of the cholesterol subfractions do not necessarily reflect the activity of these dynamic pathways—as is most true of HDL. LDL-C is generally not measured by laboratories but calculated instead, using the Friedewald equation [LDL-C (mmol l−1) = TC—(HDL-C + TG/2.20)].13 This approximation becomes less reliable at higher triglyceride concentrations (TG > 4.5 mmol l−1) and cannot be used in non-fasting samples.14
Alternatively the concentrations of the principal proteins—apolipoproteins (apo) B and A1 can be measured and can be better measures of total CVD risk12 analogous to the use of non-HDL cholesterol and HDL-C.14
Diagnosis
Lipid screening in the elderly should comprise a full profile of TC, TG and HDL-C with a calculated LDL-C. At lower levels of TC, current recommendations from the UK National Institute of Health and Clinical Excellence15 and the Joint British Societies guidelines16 recommend risk assessment using the Framingham (1991) equation. Treatment is recommended for any cardiovascular risk factor at 20%/future decade risk of CVD (15%/future decade risk of CHD). This approach differs from European17 and US guidelines18 where risk is assessed at the chronological age and treatment instituted at 20% CHD risk. It should be noted that risk assessment is an imprecise art with any estimate having a wide confidence interval.19 The UK guidelines also adjust the risk assessment to age 70 to reduce prescribing in the otherwise fit elderly given the strong association of risk with age whereby almost any 75-year-old would require lipid-lowering. This statement is controversial and many would recommend direct assessment of plaque burdens using non-invasive techniques, for example carotid intima media thickness or coronary calcium scores.20, 21
The risk assessment biochemical profile should include measurement of transaminases (AST/ALT), thyroid function tests and a baseline creatine kinase (CK). Lipid-lowering therapy with a statin or fibrate is contraindicated if AST/ALT exceeds 3 × upper reference limit of normal (ULN) (usually >150 IU l−1). The actual contraindication is to persistent elevations in transaminases as many elevations turn out to be transient and caused by either infections or are secondary to other drug therapies (e.g. heavy paracetamol or opiate-containing analgesic use). If gamma-glutamyl transferase is measured its level is irrelevant to starting or continuing lipid-lowering therapies.
Thyroid function tests should be measured. Gross hypothyroidism (TSH > 20 mU l−1) is associated with a hypercholesterolaemia and this should be treated prior to re-measurement of the lipid profile due to the risk of lipid-lowering therapy-associated rhabdomyolysis. The risk factors for rhabdomyolysis are age, creatinine, reduced muscle mass, female sex and hypothyroidism. Mild hypothyroidism is common in the elderly and not a contraindication to lipid-lowering therapies though some reports suggest that reports of myalgia may be more common in patients with borderline hypothyroidism.
The significance of CK measurement in the elderly is debated. Lipid-lowering therapies are contraindicated in patients with CK > × 10 ULN though most clinicians are reluctant to prescribe if 5 × ULN. Some elevated CK measurements, for example in Africans or Afro-Caribbeans, represent normal variants. In other patients a mildly elevated CK allied with a mild adverse reaction to lipid-lowering therapies should prompt investigation for rheumatological causes of disease as the lipid-lowering therapy may have uncovered this predisposition.
LDL-C as a Target of Therapy with Statins
Epidemiological studies incriminate high levels of LDL-C as being atherogenic with the serum TC as a good correlate for LDL-C levels.18 However, the definitive proof has come from clinical trial work of lipid-lowering interventions which has been hailed as one of the major advances in clinical medicine. Whether cholesterol is lowered by diet, drugs, or other means, CVD risk decreases.22 Comparing earlier trials of statins, and other treatment modalities such as bile acid sequestrant resins and ileal bypass surgery with more recent statin trials, the benefit of absolute LDL-C reduction is present across a wide range of baseline concentrations.
Statins
Statins form the cornerstone of pharmaceutical CVD prevention. These agents have shown to reduce the risk of both CHD and stroke in clinical trials enrolling persons aged up to age 80 years (Table 38.1). A meta-analysis of 90 056 patients which included 14 randomized trials showed that those aged >65 years (n = 6446) had 19% reduction in the risk of major cardiovascular events, a benefit similar to the 22% reduction in risk experienced by those aged <65 years (n = 7902).23 Earlier secondary prevention statin trials, such as the Scandinavian Simvastatin Survival Study (4S),24 Cholesterol and Recurrent Events (CARE),25 and Long-term Intervention with Pravastatin in Ischemic Disease (LIPID),26 support a benefit of lipid lowering after MI. Although these trials excluded patients >75 years of age (4S upper age limit, 69 years), subgroup analysis demonstrated a benefit of statins among younger elderly.27, 28 More data on statin therapy in the elderly became available following the Heart Protection Study which randomized more than 20 000 participants with known CVD or diabetes to either simvastatin 40 mg or placebo in the age range 40–80 (85 by trial end).29 Simvastatin reduced the risk of cardiovascular events by 18% in those aged 70 to 80 years (n = 5806) compared with 24% in those aged <65 years. The apparent attenuated impact of simvastatin in the older age group was not statistically significant. As the elderly have a higher absolute risk of events the number of events prevented in those aged >70 years and in those aged <70 years were similar. More evidence on the benefits of statin intervention in the elderly accumulated following the Prospective Study of Pravastatin in the Elderly at Risk (PROSPER), which was specifically aimed at evaluating the efficacy of statin use in the elderly.30 In this study 5804 subjects between the ages 70–82 years with pre-existing CHD or at high risk for CHD were randomized to 40 mg of pravastatin or placebo. Over an average of more than three years follow-up, the pravastatin group had significantly fewer combined cardiovascular outcomes (CHD death or non-fatal or fatal myocardial infarction, fatal or non-fatal stroke). The question as to whether older individuals without evidence of CVD will benefit from statin treatment (i.e. in the primary prevention setting)31 was answered by the recent Justification for the Use of Statins in Prevention: an Intervention Trial Evaluating Rosuvastatin (JUPITER) trial.32 This study compared rosuvastatin 20 mg to placebo in 17 802 apparently healthy participants with relatively low LDL-C levels of <3.4 mmol l−1 and high sensitivity C-reactive greater than 2 mg l−1. The composite primary cardiovascular endpoint showed a relative risk reduction of 44% [hazard ratio 0.56 (95% CI, 0.46–0.69)]. 5644 (32%) of participants were older than 70 years making this by far the most representative primary prevention data of the benefits of statin treatment in the elderly.
Heart failure is common in the elderly secondary to ischaemia, hypertension and cardiomyopathy. A number of statin trials have been conducted in populations with grade 2–3 heart failure after post hoc analyses of general CHD prevention trials suggested benefits in grade 1–2 disease.33 The Controlled Rosuvastatin Multinational Study in Heart Failure CORONA34 and GISSI-Heart Failure (GISSI-HF)35 studies showed no benefits of adding statin therapy in advanced heart failure but also that these drugs were not toxic in these populations.
Specific Prescribing Points in the Elderly
Data from the large trials shows little difference in side-effect rates between statin and placebo arms.36, 37 However, many patients recruited to the trials have previous experience of statins and the designs of many trials incorporate an active run-in period in which those who suffer side effects are identified early. Thus side-effect rates may be underestimated especially in elderly populations. No specific dose reduction is advised or necessary for the elderly with statins though many general practitioners worldwide initiate therapy at low doses but unfortunately do not titrate the dose to efficacious levels resulting in a persistent under-treatment of lipids in the elderly. Drug interactions vary between compounds in the statin class. The most significant interaction is of cytochrome P450 3A4 metabolized statins (lovastatin, simvastatin, atorvastatin) with other drugs metabolized by this pathway—conazole antifungals, erythromycin, and in specialist practice, cyclosporine and HIV protease inhibitors (Table 38.2). Simvastatin interacts with amiodarone at doses >20 mg and other statins should be used if amiodarone therapy is necessary (e.g. for atrial fibrillation). A weaker interaction 3A4 can occur with diltiazem through this pathway but is not usually clinically significant. Drug interactions of this type are less significant for the other statins.
All statins frequently cause gastrointestinal disturbance by a transient dysregulation of bile acid metabolism through the farnesoid-X receptor pathway. This problem may be exacerbated in patients with diverticulosis or irritable bowel disease. Gastrointestinal side effects may be accompanied by a transient increase in bilirubin and transaminases. This problem is usually self-limiting within 2–3 weeks and on repeat measurement liver profiles have usually normalized.
Myalgia occurs in 5% of patients with statin therapy and is not associated with any change in CK.37 Again often it is self-limiting but if symptoms persist than the statin therapy should be changed to the weaker agents that show predictably better side-effect profiles (pravastatin, fluvastatin). Myositis (raised CK, muscle pain) and rhabdomyolysis (CK > 20 × ULN; muscle pain; myoglobinuria) are rare side effects of statin therapy. The risk factors for rhabdomyolysis are age, creatinine, muscle mass, female sex, hypothyroidism and concomitant therapy with drugs interacting through the relevant cytochrome pathway (usually 3A4); likely to displace statins from plasma proteins; or sharing a myopathic tendency (e.g. other lipid-lowering drugs).
Ezetimibe
The cholesterol absorption inhibitor, ezetimibe, works by reducing the upper intestinal cholesterol absorption to produce in monotherapy around 20% reduction in LDL-C. This drug has proven to be very successful in the market due to its low side-effect profile with its main benefit being add-on therapy to statins to achieve targets.38 Currently no CVD outcomes data is available on ezetimibe and the importance of this has recently been highlighted.39 The Simvastatin-Ezetimibe in Aortic Stenosis trial40
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree