IODINE METABOLISM
Iodine is essential for the synthesis of thyroid hormones. With four iodines per molecule of T4, iodine comprises 66% of T4 by weight; with three iodines, T3 is 58% iodine (Fig. 30-1). Normally, ˜90 μg (˜120 nmol) of T4 and 6.5 μg (˜10 nmol) of T3 are secreted daily by the thyroid gland. Thus, 60 to 80 μg (˜550 nmol) of iodine must be transported into the gland daily to maintain normal daily hormone production.1 Iodine is not always present in sufficient quantities from dietary sources in the environment. Surprisingly, even in the United States, the daily iodine intake has been declining.2 Accumulation of the absolute iodine requirement for thyroid hormone synthesis is facilitated by an efficient system for concentrating and conserving iodine in the thyroid gland. Between 5000 and 10,000 μg of hormonal iodine is stored within the gland.1 This pool constitutes a protective reserve against periods of dietary iodine deficiency.
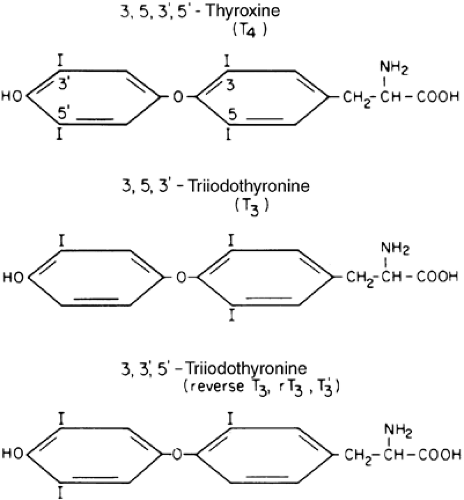 FIGURE 30-1. Chemical structures of L-thyroxine (T4), L-triiodothyronine (T3), and reverse T3 (rT3). (From Hershman JM. Endocrine pathophysiology. Philadelphia: Lea & Febiger, 1980.) |
IODIDE CLEARANCE
Within a certain range, the thyroid gland can adjust to variation in dietary iodine with changes in its clearance of iodide from plasma. However, either chronic dietary deficiency of iodine or conditions of severe iodine excess often exceed the capacity for regulation, resulting in disease states (see Chap. 37 and Chap. 38).
Virtually all of dietary iodine is reduced to iodide and absorbed in the small intestine. Circulating iodide is cleared from the blood principally by the kidney (80%) and by the thyroid (20%).1 Renal excretion, measured with a 24-hour collection, varies with filtered load and reflects 97% of dietary intake; only ˜3% is lost in the stool.1 Renal iodide is passively reabsorbed; thus, the renal clearance depends on glomerular filtration rate and is apparently unaffected by serum iodide concentration. Patients with end-stage renal disease (ESRD) have decreased renal iodide clearance and elevated serum iodide concentrations.3 Iodide excess is a proposed mechanism for the increased incidence of hypothyroidism, thyroid nodules, and goiter, whereas the mechanisms for increased thyroid cancer with ESRD are unknown.3 In contrast, thyroidal iodide clearance changes inversely with dietary intake and intrathyroidal iodine stores, increasing as much as fivefold under conditions of iodine deficiency.1
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree






