DEFINING ENDEMIC OR EPIDEMIC HAIS
Endemic HAIs are defined as sporadic infections that constitute the background rate of HAIs at the healthcare facility; the rate of such HAIs usually fluctuates from month to month, but overall it is not statistically significantly different from the background rate of these infections (see
Chapters 6,
30). Of all HAIs, endemic HAIs account for the majority of infections, and are the focus of most IC activities. The predominant pathogens and sites of endemic infection are somewhat similar at different types of healthcare facilities, but do differ on the basis of the case-mix of patients (including underlying diseases and severity of illness) and types of procedures performed and devices used (see
Chapter 30) (
Tables 8.1,
8.2A,
8.2B) (
4,
5). (http://www.cdc.gov/nhsn/PDFs/dataStat/NHSN-Report_2010-Data-Summary.pdf). Endemic infections can change in type (pathogen, site, or both) and/or rate as the result of a variety of factors, including opening or moving to a new facility, introducing a new or expanding existing clinical services or specialties (e.g., bone marrow or organ transplant, neonatal intensive care unit (ICU), surgical or medical subspecialty), introducing new diagnostic methods (e.g., laboratory or radiology), and so on.
Most endemic HAIs result from breaks in aseptic technique, most commonly from person-to-person transmission via transient HCW hand carriage of the colonizing or infecting pathogen. Numerous studies have documented that HCWs often fail to perform hand hygiene before and between contacts with patients or their contaminated environment (
6). Nevertheless, investigating endemic HAIs transmitted in this way focuses the attention on the importance of general IC recommendations (including identifying and isolating infectious patients, HCW hand hygiene, environmental cleaning and disinfection, and existing guidelines to prevent these infections) and can be associated with a reduction in the rate of these infections. Because many endemic infections are preventable, investigation of such problems by the infection preventionist (IP) or hospital epidemiologist may be warranted if the rate of endemic HAI is gradually increasing at the institution or the rate of these infections is higher than the institutional goal, that which is expected, than reported in the literature, or than reported from other similar institutions.
Epidemic HAIs are defined as the occurrence of infection at a rate statistically significantly higher than the background rate of such infections; recognized infection clusters often are unexpected, and involve either an unusual pathogen or a pathogen with an unusual antimicrobial susceptibility pattern (see
Chapters 9,
15). The recognition of clusters of common organisms with common antimicrobial susceptibility patterns may be difficult because they merge with the existing endemic infections. Often, IC personnel attempt to determine whether a cluster represents an outbreak on the basis of numerator data only. In such a situation, it is difficult, if not impossible, to determine whether a detected cluster represents an outbreak unless it involves either a very rare organism (e.g.,
Vibrio cholerae diarrhea) or a common organism with an unusual antimicrobial susceptibility pattern (e.g., vancomycin-resistant
Staphylococcus aureus).
The determination of an outbreak should not be based on numerator data alone. Although one episode of healthcare-associated malaria or cholera in a U.S. hospital represents an epidemic, one cannot determine whether a cluster of healthcare-associated S. aureus bloodstream infections (BSIs) represents an outbreak unless one can calculate and compare the S. aureus BSI rates in the time periods during and before the cluster. Because of the abrupt nature of epidemics and the feeling that most such outbreaks are preventable, in most situations epidemics warrant investigation.
RECOGNIZING ENDEMIC OR EPIDEMIC HAIS
Surveillance is the cornerstone for the rapid recognition of endemic or epidemic HAIs (see
Chapter 5). In order to detect either endemic or epidemic HAIs, one must have a surveillance program in place to detect such infections. Because the majority of HAIs arise in severely ill patients exposed to invasive devices (e.g., patients in ICUs or those with invasive devices) or those undergoing surgical invasive procedures, surveillance for infections in these populations is most important. If no systematic surveillance system is in place, many clusters may not be recognized, and if they are recognized, it is impossible to determine whether the cluster identified is endemic or epidemic unless appropriate denominator data are obtained and rates are calculated and compared.
If active prospective surveillance using standardized definitions and methodologies, such as those published by the CDC’s National Healthcare Safety Network (NHSN) (http://www.cdc.gov/nhsn/TOC_manual.html), is not conducted, it may be necessary to carry out a specific retrospective study to determine the background rate of infection before one can determine whether the HAI problem detected or recognized is endemic or epidemic (
7,
8,
9,
10,
11,
12,
13,
14,
15,
16,
17). In institutions in which active prospective surveillance is not being conducted in the area, when a cluster is detected, a retrospective study must be undertaken to attempt to reconstruct the current and past rates of such infections in the area. Only then can one differentiate between an endemic and epidemic problem. A simple definition of epidemic is a rate of HAI significantly higher than the background rate.
The early detection of infection clusters and the determination of whether the cluster identified is endemic or epidemic are most readily done if active surveillance for such infections and calculation of infection rates in the area are part of an ongoing, validated process. Once the cluster is identified, the investigator next determines whether the problem is endemic or epidemic in nature.
Differentiating endemic from epidemic HAIs requires review of how the numerator and denominator are collected, validation of the accuracy of these data, and assessment of whether factors exist that might influence either the numerator or denominator data (i.e., surveillance artifact, change in definitions, introduction of new diagnostic technologies or patient populations or procedures, etc.) (
Table 8.3). Care must be taken to ensure that surveillance artifact is not leading to an erroneous conclusion that either the number of HAIs or the HAI rate is increasing. A wide variety of factors that can inflate or deflate the numerator or denominator data can lead to surveillance artifact; they include changes in the definitions used to ascertain HAIs, HAI detection methods—including surveillance or laboratory methods—changes in the populations of patients served, devices used, or procedures performed.
Because surveillance artifact influencing either the numerator or the denominator data can prejudice HAI rate comparisons, it is important that the accuracy of these data be determined before rate comparisons are made. Although it is tempting to quickly begin comparative epidemiologic studies to ascertain the source and risk factors for infection, it is imperative that sufficient time be taken before embarking on such analyses to ensure the accuracy of the numerator and denominator data used to demonstrate that the HAI rate is increasing. Otherwise, one will be misled and devote precious personnel resources to conducting an investigation of a less urgent, non-emerging, or nonimportant problem.
Often, numerator data are the first finding that leads to a belief that there is an epidemic. Thus, confirmation of the validity and accuracy of the numerator data is an important first step. To be consistent, the numerator data should be obtained using the same standardized definition over the time periods being compared. For instance, if the IP has changed the HAI definitions used, it may appear that the HAI rate also has changed when it did not; case ascertainment has altered, and reclassification of the HAIs using the “old” surveillance definitions may show no change in the number of HAIs or the HAI rate. Even if the same surveillance definitions are used, for some sites of infection, it may still be necessary to validate the accuracy of the surveillance data.
For instance, if BSIs are being classified by the IP as primary or secondary on the basis of microbiology data, but data concerning the presence of a catheter in patients with BSIs are not being collected, there may be misclassification of BSIs. If a review of the surveillance definitions used for case ascertainment suggests that the sensitivity and/or specificity of the definitions used is low or allows for considerable subjectivity, it may be necessary to validate the accuracy of the case-ascertainment method by having several members of the IC team review each “case” independently and ensure its accuracy.
Because the existence of an outbreak usually cannot be determined by the evaluation of the numerator data alone, one needs to be equally precise in ensuring the validity and accuracy of the denominator data that will be used to calculate the HAI rates in the epidemic and preepidemic periods. The selection of the denominator to use in calculating HAI rates is critically important. Previous studies have shown that for ICU patients, the duration of a patient’s ICU stay, device (e.g., central line or urinary catheters or mechanical ventilation) exposure and the duration of that exposure, and severity of illness all contribute to the patient’s HAI risk (
10,
11,
12,
13).
Thus, these important confounding variables must be controlled for by using ICU-specific, device-specific denominator data (e.g., the number of urinary catheter days for the surgical ICU) rather than using either patients or patient-days as the denominator if valid HAI rate comparisons are to be made (
8). Similarly, the use of a surgical patient risk index that attempts to control for some of the most important factors determining a surgical patient’s infection risk, such as the type and duration of the surgical procedure, severity of illness, and wound class, is essential if valid HAI rate comparisons are to be made in surgical patients (
14,
15). In addition, other important factors such as body mass index, diabetes mellitus, reoperation, and history of smoking all of which have repeatedly been shown to increase the surgical site infection (SSI) risk should be controlled for.
In most instances, one can determine whether a perceived problem is endemic or epidemic only by the comparison of
HAI rates during the suspected epidemic and preepidemic periods. Care should be taken when comparing the HAI rate at one’s own institution with that reported either in the literature or from other institutions. Unless the surveillance methods used (including HAI definitions and case-ascertainment methods), the populations served, the types and number of invasive device used, and the types and number of surgical procedures performed are similar and the type of denominator data used for rate calculations are the same, it may be misleading to compare one institution’s HAI rate with that of another institution. Benchmarking, such as comparing to state-reported HAI rates or CDC NHSN rates, may give one a general sense of the overall HAI rate. However, because of the large number of confounding variables that can influence the numerator, denominator, or HAI rate, one often is safest comparing HAI rates over time at one’s own institution. However, even then, one must be cautious in making such comparisons, ensuring that the comparisons include both similar numerator and similar denominator data.
For example, comparison of healthcare-associated central line-associated BSI (CLA-BSI) rates in an ICU to which only medical patients are admitted with rates in another unit at that same institution to which both medical and surgical patients are admitted or comparison of healthcare-associated CLA-BSI, catheter-associated urinary tract infections (CA-UTI), SSI, or ventilator-associated pneumonia (VAP) or event (VAE) rates among patients in a medical ICU to the rates in patients in surgical ICUs maybe misleading. Because both the mix of patients and the devices used can influence HAI rates, controlling for these factors by making comparisons with similar populations and controlling for the duration of patients’ stays and devices used is necessary if valid rate comparisons are to be made. These factors are most easily controlled for by making HAI rate comparisons in a particular unit or population within an institution over time.
DIFFERENTIATING ENDEMIC FROM EPIDEMIC INFECTIONS
No one definition can be used in all situations to differentiate endemic from epidemic infections or define epidemic infections. Depending on the severity of the problem and the administrative and other pressures present, one may be able to precisely and accurately define the numerator and denominator data or need to perform a “quick and dirty” analysis to determine whether an epidemic is present and an investigation must be initiated. Once one is confident of the validity and accuracy of these data, one is in a position to compare the rate of the HAIs or other adverse events recognized in the cluster to the background rate of such events and determine whether the cluster is an epidemic or endemic occurrence. If one can confirm the accuracy of the numerator data but not the denominator data, one may be forced to use a less accurate denominator (e.g., the number of patients or the number of patient-days) to calculate the “rate.”
It must be realized that depending on the variation in the possible confounding variables, the findings of the comparison of the “epidemic” to “preepidemic” rates (i.e., statistically significantly higher, lower, or unchanged) may be misleading. Furthermore, it may sometimes be difficult, even given the appropriate numerator and denominator data, to determine whether a cluster of infections is endemic or epidemic. For
instance, if an endemic rate of infection continues to rise, at some point it may be considered epidemic in nature if recent experience is compared with suitable remote baseline data. In other situations, the lack of background rate data (e.g., no surveillance conducted, new patient population or new diagnostic test introduced at the facility) may preclude the possibility of making rate comparisons. However, in most situations, it is possible to either determine or estimate the background rate and to decide whether the detected cluster of HAIs represents an epidemic or endemic problem. The recent development of a variety of computer statistical software packages has simplified the calculation and comparison of HAI rates; however, the ease with which it is possible to make such comparisons has further highlighted the importance of ensuring the accuracy and validity of the numerator and denominator data used (see
Chapter 10).
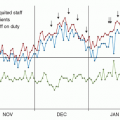
Some researchers have suggested conducting prospective surveillance and using threshold programs to determine when the HAI rate increases above a certain level that warrants further investigation. Such programs were used in the 1970s in the CDC’s National Nosocomial Infections Surveillance (NNIS) system and were found to be unreliable because of normal variations in the HAI rate at most institutions. Although it may be easy to establish a high HAI rate above which further investigation is indicated, the sensitivity of such a system would be low. To date, it has been impossible to design a sensitive and specific threshold program that would not only identify all epidemics when they occur, but also highlight other nonoutbreaks as clusters requiring investigation. It has been equally difficult to develop a sufficiently sensitive and specific threshold program for the detection of clusters requiring further investigation.