Intervertebral Disc Structure, Composition, and Mechanical Function
Samuel A. Joseph Jr.
Patrick Boland
The spine can be considered a column of relatively rigid vertebrae connected by flexible intervertebral discs. Because of their flexibility, the intervertebral discs allow the spine to twist and bend throughout a wide range of postures. In addition to allowing flexibility, the intervertebral discs function in both absorbing energy and distributing loads applied to the spine. The unique structure and composition of the intervertebral disc allow for a wide array of mechanical functions to be performed. It is the disruption of this relationship that leads to intervertebral disc pathology.
Anatomy, Structure, and Composition
Anatomy
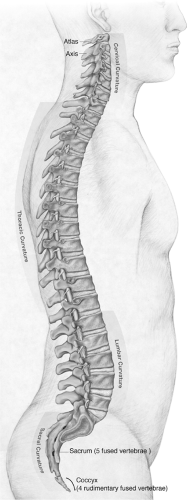
There are 23 discs in the human spine, which account for 20% to 30% of its length. Apart from the fused vertebrae of the sacrum and coccyx, the only vertebrae not connected by discs are the atlas and axis, which pivot at the specialized atlanto-axial joint, and the articulation between the atlas and the base of the skull, which articulate at the occipitoatlantal joint; this articulation also does not contain a disc (Fig. 23-1).
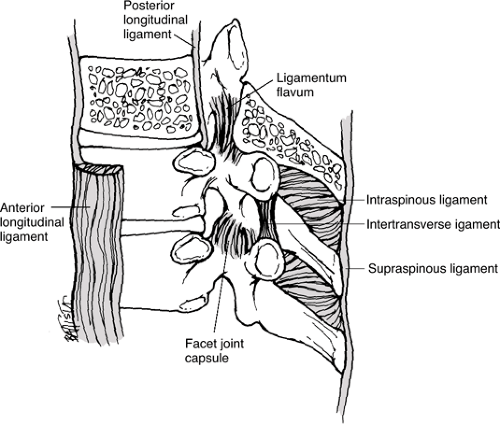
Non-disc structures also connecting the vertebral bodies (Fig. 23-2)
Anterior and posterior longitudinal ligaments
Ligamenta flava
Interspinous ligaments
Supraspinous ligaments
Structure
Shape
Roughly cylindrical
Most discs appear wedge-shaped because the anterior height is greater than posterior.
Cross-sectional area increases almost linearly from the cervical to lumbar segments.
Unlike cross-sectional area, disc height does not vary regularly along the length of the spine.
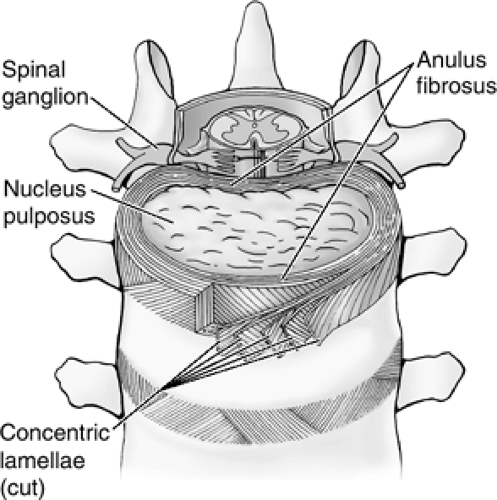
Components
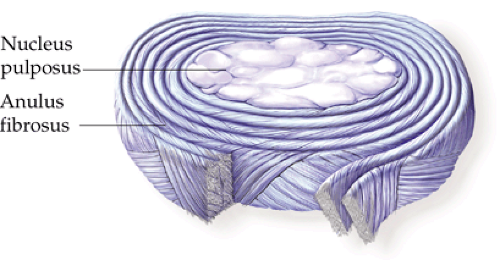
Nucleus pulposus: soft inner region
Anulus fibrosus: surrounding tough outer lamellae
Consists of 12 concentric coaxial lamellae that form a tube-like structure enclosing the nucleus
Arranged into a densely packed outer ring and an inner, larger fibrocartilaginous layer (Fig. 23-3)
Vascularity: largest avascular organ in the body
Small blood vessels found on the surface of the outer anulus penetrate 1 to 2 mm at most.
Simple diffusion is the most important mechanism for small-molecule transport into the disc and appears to be the factor most responsible for limiting cell viability.
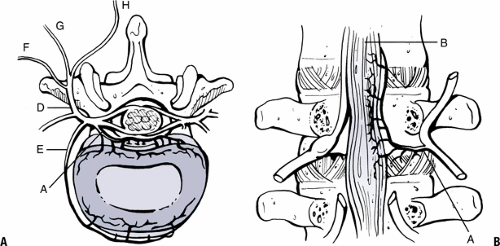
Innervation: poorly innervated
Sensory nerves do not penetrate deeper than the outer third of the anulus.
Main afferent pathway involves the nerve to the vertebral body: sinuvertebral nerve (recurrent nerve of Luschka) (Fig. 23-4).
Composition
Even though the discs may vary in size, they share the same basic structure and composition.
Two main structural components of the intervertebral disc
Collagen
Accounts for 70% of the dry weight of the anulus and <20% of the nucleus
Provides tensile strength
Proteoglycans
Account for a minimal percentage of the anulus but as much as 50% of the nucleus in the pediatric population
Provide stiffness, compressive strength, viscoelasticity
Collagen arrangement
Types I and II collagen fibrils
Distributed radially in opposing concentration gradients, with type II mostly in the nucleus pulposus and type I most concentrated in the exterior of the anulus
Anulus: I, II, III, V, VI, IX, X
Nucleus pulposus: II, VI, IX, X
Type I collagen provides strength to the tough lamellar sheets that are anchored into the bone of the adjacent vertebral bodies (Fig. 23-5).
Water: contained in the matrix of the disc and contributes approximately 65% to 80% of its total weight
Aggrecan is the main proteoglycan in the disc.
High density of negatively charged sulfate and carboxyl groups (cations) on the glycosaminoglycan chains that attract mainly Na+ (anions), which results in a cumulatively increased osmotic pressure of 1 to 3 atmospheres in the nucleus
Pressure gradient enables the disc to continually absorb water.
Hydration and swelling continue until it is restricted by the collagen network of the disc.
Equilibrium between the aggrecan and collagen provides the load-bearing, compression-resisting tissue that holds the other units of the spine in correct position while allowing movement of the spinal column.
Mechanical Function
Withstands the significant forces of an upright posture
Forces up to 17,000 Newtons estimated in lumbar discs
Functions within a specialized unit called the motion segment (Fig. 23-6), where the basic motions of axial compression, torsional loading, and sagittal and transverse bending or axial torsion occur (Fig. 23-7).
Biphasic viscoelastic behavior during loading (Table 23-1)
Mechanical loading causes fluid movement within the discs, which gives rise to time-dependent mechanical properties.
The less dense inner anulus and nucleus pulposus undergo larger volumetric changes in response to loads. This creates flow within the disc that dissipates the energy and causes viscoelastic creep.
The stiffer outer anulus converts this compressive load into hoop stresses while the inner layers act as a “shock absorber.”
The high tensile modulus of the outer anulus helps to prevent any bulging of the disc from the loads applied.
Torques on the motion segment distort the shape of the anulus without altering the volume, while bending and compression cause disc bulging, volumetric changes, and endplate deformation.
Function of the cartilage endplate
The hydraulic permeability causes rapid fluid transport and less pressurization in response to loading.
This permeability provides a conduit for water to flow from and into the disc and thereby helps transfer loads in a uniform manner across the inner anulus and nucleus pulposus.
Disc Aging
Age-related deterioration of the intervertebral disc leads to two of the most common clinical disorders of the spine:
degenerative disc disease and disc herniation. Changes in volume and shape are accompanied by gross morphologic and microstructural alterations (Table 23-2). The most extensive changes occur after the age of 20 in the nucleus pulposus, where the number of viable cells and the concentration of proteoglycans and water decline.
degenerative disc disease and disc herniation. Changes in volume and shape are accompanied by gross morphologic and microstructural alterations (Table 23-2). The most extensive changes occur after the age of 20 in the nucleus pulposus, where the number of viable cells and the concentration of proteoglycans and water decline.
Degenerative Disc Disease
Disc degeneration is a multifactorial process that is complex and poorly understood. It is the result of an intricate relationship between cellular biology, mechanical factors, and genetics. Aging and degeneration of discs are separate processes: although all discs undergo aging, not all of them degenerate. The end stage of degeneration can be identified by imaging studies and gross examination, but accepted criteria for the diagnosis and the distinguishing factors between degeneration and aging have not been established. It is also unclear as to what degree the degenerative process contributes to pain. Currently disc degeneration is believed to be a source of chronic pain, and over 90% of surgical
spine procedures are performed because of consequences of the degenerative process.
spine procedures are performed because of consequences of the degenerative process.
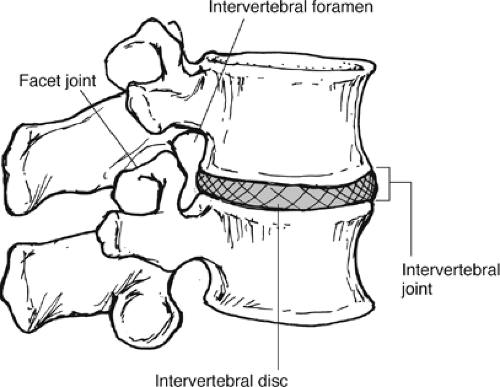 Figure 23-6 A motion segment consists of an intervertebral disc and the two adjacent vertebral bodies. (From Oatis CA. Kinesiology: The Mechanics and Pathomechanics of Human Movement. Baltimore: Lippincott Williams & Wilkins, 2004.)
Stay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree
 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access

|