|
Disease: Leukemias, MDS, or lymphoma: Leukopenia 2° to marrow dysfunction or leukemic infiltration; MM: Functional hypogammaglobulinemia- predisposes to infxn w/encapsulated organisms. CLL: Hypogammaglobulinemia; heavily pretreated w/lymphotoxic purine analogs such as Fludarabine or Pentostatin causes defects in cell-mediated immunity against pathogens like Listeria, Pneumocystis jiroveci, mycobacteria, opportunistic viral & bacterial pathogens (Cancer 2002;94:2033; Clin Exp Immunol 1992;89:374; Oncology (Huntingt) 2000;14:41). Refractory CA: ↑ risk due to marrow infiltration or poor marrow function due to previous toxic therapies.
Chemotherapy: Monoclonal Ab: Anti CD52- Alemtuzumab causes sev. & prolonged T cell depletion; Anti CD20- rituximab & Ofatumumab cause reactivation of viral diseases such as Hepatitis B and PML (Ann Hematol 2011;90:1219; Blood 2009;113:4834). Bortezomib, Temozolomide: Lymphocyte-depleting agents; can cause disseminated VZV, Pneumocystis jiroveci infxn. Corticosteroids: Dose & duration dependent- Pneumocystis jiroveci & Nocardiosis can occur.
Tumor size: Bulky tumors overgrow their blood supply & necrose, serving as nidus for infxn. Anatomical disruption: Hepatobiliary, urinary or GI tract tumors cause stasis due to obstruction w/infxn; culprit organisms are usually commensal bacteria.
Transplantation: Allogeneic transplant: ↑ predisposition for infxn compared to autologous. Splenic radiation; sev. GVHD: Functional asplenia- can cause overwhelming infxn w/ encapsulated organisms such as Streptococcus pneumoniae, Haemophilus influenzae, & Neisseria meningitidis (J Natl Compr Canc Netw 2012;10:1412).
|
Definitions: ANC < 500 cells/mm3 or if expected to ↓ in next 48 h; profound neutropenia: ANC < 100 cells/mm3; functional neutropenia: Counts are nl or ↑, but do not function appropriately
hematologic tumors (Clin Infect Dis 2004;39:32). Infxn occur in 20-30% of febrile episodes; common sites are intestinal tract, lung, & skin. Bacteremia occurs in 10-25% of all pts, particularly in profound & prolonged neutropenia (Ann Intern Med 1966;64:328; Blood 2006;107:4628; Clin Infect Dis 2004;39:25).
|
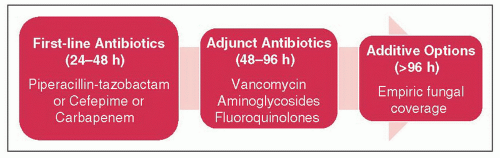
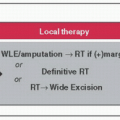
First-line Rx: Should be w/antipseudomonal abx. Vancomycin & aztreonam can be used in case of allergy (hives/bronchospasm) to first-line abx.
Adjunct abx: Should not be started first line, unless there are specific indications, like suspected catheter-related infxn, skin or soft tissue infxn, PNA, hemodynamic instability, or multidrug-resistant organisms (such as MRSA, resistant gram-negative organisms) (Clin Infect Dis 2011;52:56). Must use local antibiogram & institution-specific guidelines to make choices.
Empiric fungal coverage: Choices are echinocandins, liposomal Amphotericin B, or Voriconazole
|
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree