Infection Risks Due to Athletes’ Personal and Social Behaviors
Daniel J. Sexton
Christopher J. Hostler
Introduction
This chapter focuses on explaining how personal and social behaviors affect an athlete’s risk of infection. Several best practices and recommendations have been included to help team medical personnel mitigate these risks and behaviors. Simple interventions and player education can substantially and effectively reduce these risks for athletes.
Basic Premises
Consistent use of best practices related to personal hygiene is the primary method of infection prevention among athletes. Such practices are simple and effective. For example, direct contact between athletes (hand-to-skin, skin-to-skin, and mucous membranes-to-skin) is how most bacterial and many viral pathogens are transmitted in athletic facilities. Bacterial pathogens such as methicillin-resistant Staphylococcus aureus (MRSA) are frequently present on the hands of players and athletic trainers and, if personal hygiene is not scrupulously practiced, these microbes can be transmitted to other players and staff. This sequence of transmission can in turn lead to clinical infection, especially if other players have abraded or damaged skin. Athletes train and interact with one another in facilities that allow unusually close contact. If personal hygiene is ignored, these interactions and close contact in turn facilitate and increase the risk of transmission of pathogens such as MRSA, respiratory viruses, and numerous other potential pathogens.
Basic personal hygiene practices such as hand hygiene, prompt showering after practice, and avoidance of sharing personal equipment such as towels and razors can prevent transmission of infectious agents in team settings. Other measures such as keeping cut or abraded skin clean, dry, and covered are also important. All the personal hygiene practices discussed below should be ingrained and regularly practiced by all team members and staff even when all individuals seem to be and feel perfectly healthy.
Basic personal hygiene practices such as hand hygiene, prompt showering after practice, and avoidance of sharing personal equipment such as towels and razors can prevent transmission of infectious agents in team settings.
As discussed elsewhere, asymptomatic colonization of staff and players is common, and transmission of pathogens such as MRSA can occur from a healthy team member to a team mate. Such transmission from asymptomatic staff or patients occurs regularly in healthcare facilities throughout the world when lapses in personal hygiene occur.
Finally, personal and social behaviors of individual athletes may have direct or indirect adverse effect on the health of their teammates. For example, athletes with skin, gastrointestinal, or respiratory infections who fail to report and seek immediate treatment from athletic trainers or team physicians before participating in practices or competition can expose their teammates, opponents, and other staff members to transmissible pathogenic viruses or bacteria.
Hand Hygiene
Tips and Advice
Athletes should be educated about basic hygienic practices that reduce their and fellow team members’ risk of becoming ill.
Hand hygiene and access to hand cleaning agents should be facilitated and promoted in all athletic training facilities.
Signage and other types of reminders can be helpful in promoting basic knowledge about and adherence to basic personal hygienic practices such as hand hygiene, prompt showering after practices, and other strategies that reduce the risk of transmission of common pathogens.
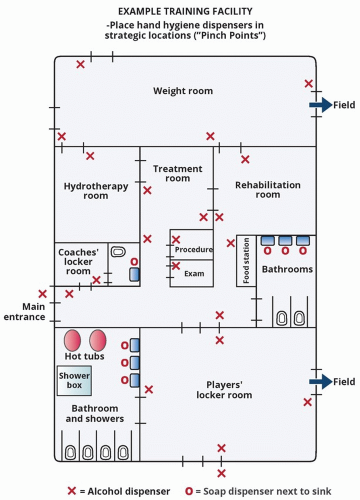
Identify strategic locations for hand hygiene stations, including all entry and exit points in the training room, treatment room, locker room, exercise rooms, weight rooms, meeting rooms, and the cafeteria (see Figure 3.1).
Encourage athletes to perform hand hygiene any time they pass a dispenser.
 Best Practice Educate athletes to routinely perform hand hygiene with alcohol-based hand hygiene cleaning agents before eating, when players and staff enter the training facility and treatment areas and when hands are visibly soiled or contaminated.
Best Practice Educate athletes to routinely perform hand hygiene with alcohol-based hand hygiene cleaning agents before eating, when players and staff enter the training facility and treatment areas and when hands are visibly soiled or contaminated.Rationale: Direct (skin-to-skin) transmission is the primary method by which most bacterial pathogens (such as MRSA) are transmitted in athletic facilities. Similar direct transmission is also important in the spread of viruses causing influenza and the common cold. Pathogens such as MRSA are often temporarily present on the hands of team players and team medical personnel; these agents can be transmitted to others if hand hygiene is not performed correctly. Alcohol-based hand hygiene products are highly effective in reducing person-to-person transmission of almost all pathogens including MRSA.1,2 Alcohol-based
hand hygiene products are as effective as traditional handwashing with soap and water in most situations. Use of alcohol-containing hand cleaning agents takes less time and causes less skin irritation than soap and water. Adherence to hand hygiene protocols and best practices should be expected of all players. Team leadership should reinforce and correct players and staff who have lapses in following this important best practice. Promoting adherence to this best practice is a cornerstone of developing a culture of safety and excellence among all team players and staff.
hand hygiene products are as effective as traditional handwashing with soap and water in most situations. Use of alcohol-containing hand cleaning agents takes less time and causes less skin irritation than soap and water. Adherence to hand hygiene protocols and best practices should be expected of all players. Team leadership should reinforce and correct players and staff who have lapses in following this important best practice. Promoting adherence to this best practice is a cornerstone of developing a culture of safety and excellence among all team players and staff.
Tips and Advice
Alcohol-based hand hygiene products can be delivered as foams, gels, or liquids. All of these formulations have similar efficacy.
Dispensers should be located in easily accessible and visible locations.
 Recommendation 2 Clean hands with soap and water instead of alcohol-based products after toileting and when they are visibly soiled or heavily contaminated with dirt, debris, or body fluids such as mucus or blood.
Recommendation 2 Clean hands with soap and water instead of alcohol-based products after toileting and when they are visibly soiled or heavily contaminated with dirt, debris, or body fluids such as mucus or blood. Recommendation 3 Remind athletes to clean hands with soap and water instead of alcohol-based products when anyone in the facility has a diarrheal illness.
Recommendation 3 Remind athletes to clean hands with soap and water instead of alcohol-based products when anyone in the facility has a diarrheal illness.Rationale: Alcohol-based hand hygiene products are not effective when hands are heavily soiled with dirt, feces, or other material such as oils or blood. Alcohol does not kill two important pathogens that cause highly transmissible diarrheal illness—norovirus and Clostridioides difficile (also known as “C. diff”).
 Recommendation 4 Signage that informs and prompts all visitors and players to clean their hands should be placed at strategic locations throughout the facility.
Recommendation 4 Signage that informs and prompts all visitors and players to clean their hands should be placed at strategic locations throughout the facility.Rationale: Placement of signage promoting hand hygiene underscores a team-wide commitment to the routine and frequent use of hand hygiene agents. Similar to the placement of hand hygiene stations, these signs should be located at strategic location throughout the facility, such as at entry points to the facility, treatment areas, locker rooms, and weight rooms.
 Recommendation 5 Use moisturizing hand lotions or emollients if the skin on hands is dry or cracked.
Recommendation 5 Use moisturizing hand lotions or emollients if the skin on hands is dry or cracked.Rationale: Frequent use of alcohol-containing hand hygiene products may lead to dry and cracked skin. While most hand hygiene products also contain emollients to prevent drying of skin, frequent use of these agents may still result in drying and cracking of skin. Dry, cracked, or irritated skin is more likely to harbor pathogens such as MRSA. Thus, ensuring that lotion is available for use can help overcome this potential side effect of increased hand hygiene. Lotion is best distributed via pumps from nonrefillable containers.
Tips and Advice
When possible, lotion should be dispensed via pumps from nonrefillable containers. Refillable containers can become contaminated with bacteria.
 Recommendation 6 Use hospital-grade soap from prefilled/prepackaged dispensers in the training, treatment, and examination/procedure rooms.
Recommendation 6 Use hospital-grade soap from prefilled/prepackaged dispensers in the training, treatment, and examination/procedure rooms.Rationale: Handwashing with soap and water rather than alcohol-based products is necessary in selected situations as discussed above. There is no compelling evidence that antibacterial soaps prevent infection in the community better than plain soap and water.3 Antibacterial soaps are recommended for use in medical facilities. However, we currently do not recommend the use of soaps containing triclosan. Instead, we recommend using hospital-grade liquid soaps containing chloroxylenol, benzalkonium, or chlorhexidine in prefilled dispensers. Triclosan, the active ingredient of most commercially available household antibacterial liquid soaps, may disrupt reproductive or thyroid function in aquatic life and laboratory animals.4,5 In fact, the Food and Drug Administration (FDA) recently concluded that the majority of chemicals used in the over-the-counter antiseptic soap, including triclosan, were “not generally recognized as safe and effective.”6
Finally, refillable soap dispensers have a small but known risk of becoming contaminated with potential pathogens such as Pseudomonas and Serratia. Thus, prefilled/prepackaged dispensers that can be replaced when the soap content becomes empty or low are recommended.
Skin Hygiene
 Best Practice Shower after practice to decrease the risk of bacterial transmission from player to player and player to environment.
Best Practice Shower after practice to decrease the risk of bacterial transmission from player to player and player to environment.Rationale: MRSA exposure in the setting of skin abrasions and cuts acquired through routine team activities such as practice or workouts substantially increases the risk of subsequent infection. The highest risk of transmission of important pathogens such as MRSA from one player to another likely occurs during and immediately after practice. Approximately 1% to 3% of the general American population is colonized with MRSA,7,8 but as many as 10% to 20% of competitive athletes are colonized either transiently or for longer time periods.9,10 Thus, periodic contact with MRSA is inevitable in team settings. Such exposures occur “silently,” and players and staff have no way to know when such exposures occur.
In other words, there is no amount of infection prevention interventions that will eliminate all exposures during athletic endeavors. As a result, players must assume they have been and will be exposed to MRSA and other potential pathogens during practices and games. Showering immediately after practice or games is a critical step to prevent long-term skin colonization with MRSA particularly if there are minor skin cuts or abrasions (Figure 3.2). Showering also reduces the density and number of MRSA bacteria on the skin of colonized players which further reduces the risk of a true skin infection if minor cuts or skin abrasions are present. Finally, showering also reduces the density and amount of MRSA bacteria in the environment of the team training facility and locker room.
There is no amount of infection prevention interventions that will eliminate all exposures during athletic endeavors.
Educate players—“you will be exposed to MRSA during routine athletic activities.”
Showering immediately after practice will decrease the risk of MRSA infections in three specific ways:
Prevents long-term colonization. Showering removes bacteria before long-term colonization occurs and before low-grade colonization (following an exposure) results in infection in skin transiently damaged by minor cuts or abrasions. Prompt showering after games or practice is also an effective way to prevent long-term colonization in players who had direct skin-to-skin contact with other players who have long-term colonization with MRSA.
Reduces the density and number of MRSA bacteria in colonized players. Players who are colonized with MRSA are at increased risk of subsequent MRSA infection.11 Showering immediately after practice reduces the amount of MRSA on the skin in patients previously colonized with MRSA, thereby also decreasing the risk that any cuts or skin abrasions sustained during practice become infected.
Reduces the amount of MRSA in the environment. Players who are heavily or transiently colonized with MRSA on the skin are more likely to contaminate the environment. Postpractice showers reduce the amount of MRSA on the skin and, thus, secondarily reduce contamination of the training facility and its equipment.
Tips and Advice
Use of bar soap in showers is not recommended. Bar soap has been implicated as a potential source of MRSA transmission in athletes and in prisons.12
Soap dispensers that utilize prefilled/prepackaged liquid soap are preferable.
 Recommendation 3 If hair is removed with clippers, dispose of the clipper head after each use or ensure that each player has a dedicated clipper head.
Recommendation 3 If hair is removed with clippers, dispose of the clipper head after each use or ensure that each player has a dedicated clipper head. Recommendation 4 If body hair is electively removed by shaving, shave clean skin with a fresh razor using soap and lubricants at locations separate from the athletic training facility.
Recommendation 4 If body hair is electively removed by shaving, shave clean skin with a fresh razor using soap and lubricants at locations separate from the athletic training facility.Rationale: Shaving causes small, frequently invisible abrasions and cuts in the skin.13 Pathogenic microorganisms such as MRSA and group A streptococci can access these tiny skin defects. This sequence, in turn, often leads to long-term skin colonization and/or an increased risk of subsequent skin and soft-tissue infections.14 This phenomenon is directly responsible for the well-known fact that preoperative skin shaving of the operative site significantly increases the risk of wound infections after surgery. As a result, shaving of hair prior to a surgical procedure is strongly discouraged.15
Cosmetic shaving has been implicated in outbreaks of MRSA infections in athletes. For example, 10 players on a college football team developed MRSA cellulitis or skin abscesses
during a 2-month period; body shaving was strongly and significantly associated with increased MRSA infection risk in this outbreak.16 If hair removal below the neck is required for medical reasons or for personal preferences of a player, hair should be removed using clippers that have a disposable rather than reusable head.
during a 2-month period; body shaving was strongly and significantly associated with increased MRSA infection risk in this outbreak.16 If hair removal below the neck is required for medical reasons or for personal preferences of a player, hair should be removed using clippers that have a disposable rather than reusable head.
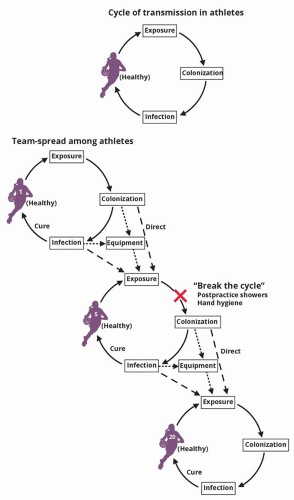 Figure 3.2 Break the transmission cycle—shower after practice to prevent exposure leading to colonization. |
Intact skin is the most important defense against skin infections
We acknowledge that certain athletes (such as swimmers, cyclists) may practice body shaving for aerodynamic improvement. Similarly, athletes may shave legs and armpits for social reasons. If shaving for these reasons is required, athletes must be educated to NEVER share a razor. Ideally, shaving for these purposes should be performed at home with a skin lubricant after the skin has been cleaned with soap. Ultimately, the decision to use cosmetic body shaving is largely a personal matter beyond the control of team physicians and athletic trainers. Thus, bans on such practices are, in most instances, neither practical nor absolutely necessary in healthy players. Temporary bans on cosmetic body shaving, however, can be reasonably used by teams as secondary control measure when clusters of two or more MRSA infections occur over a short time period.
Signage may be useful in educating players about the risks associated with cosmetic body shaving and may reduce the number of players who use body shaving or the frequency of such shaving. Similarly, these risks should be part of the team’s annual or new-player educational programs on infection prevention. Players should be reminded that the consequences of a skin infection on their career or on their performance during an individual season should be weighed against the benefits of cosmetic body shaving.
Tips and Advice
Place signage in the team training facility to educate and remind players about the risk of cosmetic body shaving.
Educate players about the risks of body shaving below the neck during the team’s annual or new-player educational sessions.
 Recommendation 1 Body piercings of the tongue, lips, nose, eyebrows, nipples and “high piercing” of the cartilage portion of the ear in athletes should be avoided due to risk of infection.
Recommendation 1 Body piercings of the tongue, lips, nose, eyebrows, nipples and “high piercing” of the cartilage portion of the ear in athletes should be avoided due to risk of infection.Rationale: Complications of body piercing can be severe. These complications include local and systemic infections and allergic (contact) reactions; keloid formation; and secondary risks of traumatic tearing during play as well as permanent scarring and disfigurement. Such complications are particularly common when piercing occurs in unregulated and often unsafe locations such as piercing studios, shopping mall kiosks that lack appropriate sterility and infection control practices, and/or when performed by personnel who lack education and understanding about basic sterility, disinfection of equipment, and sterile technique. Outbreaks of serious infections after body piercings have been linked to use of contaminated “after-piercing” solutions and inadequate disinfection of equipment used in the piercing process.17 Piercings performed by inadequately trained personnel or in locations lacking appropriate equipment and sterility can also lead to hepatitis B or C infections or, rarely, secondary infections of the heart valves or brain abscesses.
Tips and Advice
Athletes who have piercings should remove all jewelry from pierced body parts while competing or training.
Athletes who decide to have piercings should visit the studio or facility prior to the procedure to examine and understand the availability of sterile equipment and to be certain that the personnel performing the piercing have a full understanding of sterile technique, proper disinfection, and proper storage of equipment.
Rationale: Permanent tattoos can occasionally result in serious complications including keloid formation, localized infections with bacteria such as MRSA, and various mycobacteria that can be difficult to treat, hepatitis B and C infections, and both major and minor hypersensitivity reactions related to the various metallic salts used in tattoo pigments.
Tips and Advice
We acknowledge “discouraging” body piercing and tattoos is an uphill battle for medical personnel, as both are increasingly a part of sports culture and society in general. Nevertheless, we recommend providing important information about infection risks related to these practices to athletes before they elect to participate in them.
Athletes should be educated about the potential risks of tattoos and provided basic information about how to avoid or minimize these risks.
Athletes who are contemplating getting a new tattoo should be counseled to avoid tattoo parlors or tattoo artists that fail to properly use sterile and aseptic techniques or work in studios that lack appropriate infection control products, supplies, and processes (eg, gloves, hand hygiene sterile materials, and storage facilities).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree