and Christian Waldherr1
(1)
Bern, Switzerland
3.1 Recall Rate
3.1.1 Case 1
General Information/Clinical Issues
Patient was a 49-year-old female, she presented with significant palpable laterocranial mastopathy on both sides.
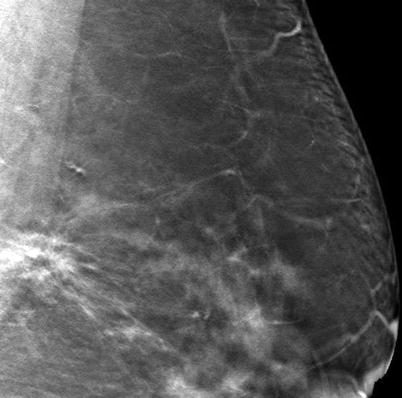
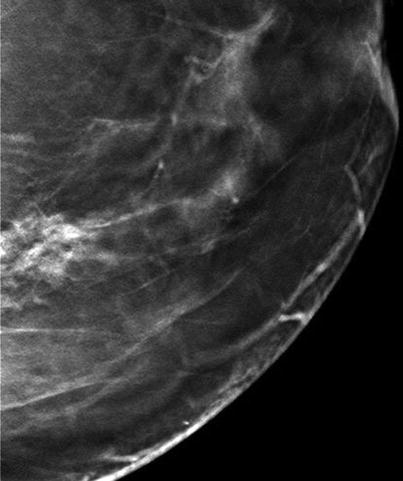
Mammographic Analysis—two-dimensional (2D) and 3D
Breast density American College of Radiology (ACR) III, on 2D in left oblique (Lobl) projection (Fig. 3.1a, b); increase in density/developing asymmetry on follow-up 2D in the posterior portion of the left breast cranial, not visible in left cranio-caudal (Lcc) view on 2D (Fig. 3.2a, b); Breast Imaging Reporting and Data System (BI-RADS) 0. On 3D in both views there was no visible mass or architectural distortion (Figs. 3.3a–c and 3.4); BI-RADS 1.
Fig. 3.1
(a, b) Two-dimensional (2D) (a) oblique (obl) in 2009 and (b) obl in 2011
Fig. 3.2
(a, b) 2D (a) cranio-caudal (cc) in 2009 and (b) in 2011
Fig. 3.3
(a–c) 3D slices (a–c) Lobl
Fig. 3.4
3D slice (cc)
Differential Diagnosis on 2D
Summation artifact (resulting from superimposed normal breast structures on 2D image mimicking a possible lesion), ductal carcinoma in situ (DCIS), invasive breast cancer (BI-RADS 0).
Conclusion/Diagnosis with 3D
Allows precise localization of a breast change and significantly improves diagnostic accuracy of non-calcified lesions compared with 2D, due to reducing overlapping breast tissue; 3D slices in both views show normal breast tissue that is superimposed, forming the summation artifact on 2D; no suspicious lesion on 3D (BI-RADS 1).
Recommendation for 2D
Additional spot view or 3D and US; BI-RADS 0
Recommendation for 3D
No recommendation, BI-RADS 1
US
No internal US.
Histology
−
Further Imaging/Further Diagnostic
−
3.1.2 Case 2
General Information/Clinical Issues
Patient was a 54-year-old female; screening; no prior images.
Mammographic Analysis—2D and 3D
Breast density ACR III. On 2D in Lcc projection (Fig. 3.5a, b) in side-to-side comparison at least one nonspecific convex ill-defined 11 mm density was medially located in the retroglandular clear space. In Lobl view on 2D the density was centrally located (Fig. 3.6a, b); BI-RADS 0. On 3D in Lcc views, there were two oval-shaped sharply defined 9- and 11 mm masses without calcifications (Fig. 3.7); BI-RADS 2.
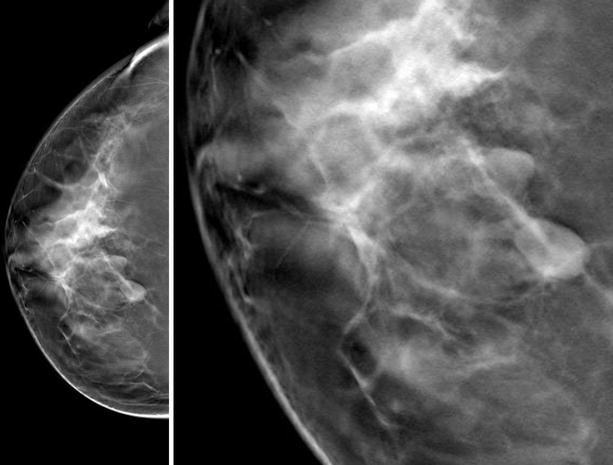
Fig. 3.5
(a, b) 2D (a) and (b) in cc
Fig. 3.6
(a, b) 2D (a) and (b) in obl
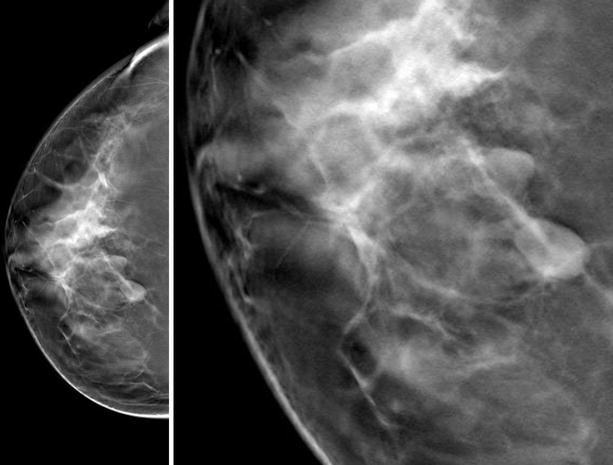
Fig. 3.7
3D cc and magnification cc
Differential Diagnosis on 2D
Normal fat-containing breast tissue, lymph node, fibroadenoma, DCIS, invasive breast cancer (BI-RADS 0).
Conclusion/Diagnosis with 3D
Allows precise localization of a breast lesion and significantly improves diagnostic accuracy of non-calcified lesions due to reduced superimposed breast tissue, compatible with a benign lesion (BI-RADS 2).
Recommendation for 2D
Spot view or 3D, US.
Recommendation for 3D,
US optional.
US
No internal US.
Histology
−
Further Imaging/Further Diagnostic
−
See Sect. 3.9 diagnostic work-up spot vs. DBT (digital breast tomosynthesis) Case 1
Comment
The apparent lack of sensitivity on 2D is caused by fibroglandular breast tissue overlapping the cancer or by architectural distortion, and misinterpretation of asymmetrical density on 2D-detected abnormalities. On 3D there is a reduction of the pseudo-lesions seen on 2D (caused by superposition of breast tissue on 2D).
Image Interpretation Pearls
To compensate for the limitations on 2D imaging we compare images with prior mammograms, if available. Especially in dense breast tissue, the margins of a lesion can be obscured due to the superposition of normal breast tissue, or a summation artifact can simulate a true lesion. On 2D the margins of the detected abnormalities in these cases are not clearly seen, illustrating the challenge of confirming or excluding a breast cancer in heterogeneously dense breast tissue. On the other hand, some malignant tumors also have sharp boundaries (see Chap. 7, Papillary cancer).
3.2 Higher Cancer Detection Rate
3.2.1 Case 1
General Information/Clinical Issues
Patient was a 60-year-old female; screening mammograms every 2 years (double reading); no signs or symptoms.
Mammographic Analysis on 2D, 2D (synthetic), and 3D
Breast density ACR II. On 2D in 2007 inhomogeneous breast tissue with a focus on a nonspecific density in Lcc view lateral and ‘iffy’ radial distortion right retromammillary, most probably due to summation artifact (Figs. 3.8a, b and 3.9a, b); BI-RADS 0. On 2D (synthetic) in 2013 there is a spiculated isodense mass laterocranial on the right side (Fig. 3.10a, b); BI-RADS 5, identified retrospectively in knowledge of the location already identified in Lcc views on 2D in 2007 and 2009 and detectable in 2011 (Fig. 3.11a–c), and somewhat less obvious in the Lobl view on 2D (Fig. 3.12a–c); on 3D the spiculated mass is clearly visible in both views (Fig. 3.13a, b and Fig. 3.14 [3D magnification, same figure as 3.13a]); BI-RADS 5.
Fig. 3.8
(a, b) 2D obl in 2007
Fig. 3.9
(a, b) 2D cc in 2007
Fig. 3.10
(a, b) 2D synthetic (a) obl and (b) cc in 2013
Fig. 3.11
(a–d) 2D (a–c) cc in 2007, 2009, and 2011 and 2D (synthetic); d (same figure as Fig. 3.10b) cc in 2013
Fig. 3.12
Fig. 3.13
(a, b) 3D (a) obl and (b) cc in 2013
Fig. 3.14
3D magnification (cc)
Differential Diagnosis on 2D
Questionable radial distortion right retromammillary on 2D in 2011 in one-view Robl (described by one reader), stable and pre-existing on follow-up, most probably due to summation artifact.
Conclusion/Diagnosis with 2D (Synthetic) and 3D
Lesion missed over years with 2D, easy to identify with 2D (synthetic) and 3D, highly suggestive of malignancy (BI-RADS 5).
Recommendation
Ultrasound (US) biopsy recommended.
US
No internal US.
Histology
Invasive ductal carcinoma.
Further Imaging/Further Diagnostic
No magnetic resonance imaging (MRI) recommended, optional
3.2.2 Case 2
General Information/Clinical Issues
Patient was a 60-year-old female; family history of breast cancer.
Mammographic Analysis on 2D, 2D (synthetic), and 3D
Breast density ACR III, no obvious changes on 2D follow-up mammograms (Fig. 3.15a–c Lobl and Fig. 3.16a–c Lcc); BI-RADS 2. In 2014, 2D (synthetic) and 3D showed a spiculated mass (5 mm in size) craniomedially in the forbidden area close to the chest wall on the left side (Figs. 3.15d, 3.16d, 3.17 3.18a, b, and 3.19 [3D magnification, same figure as Fig. 3.18a]); BI-RADS 5.
Fig. 3.15
(a–d) 2D (a–c) obl in 2008, 2010, and 2012; 2D synthetic obl (d) in 2014
Fig. 3.16
(a–d) 2D (a–c) cc in 2008, 2010, and 2012; 2D synthetic (d) in 2014
Fig. 3.18
(a, b) 3D (a) obl and (b) cc in 2014
Differential Diagnosis on 2D
Lymph node, small cyst, fibroadenoma.
Conclusion/Diagnosis with 2D (synthetic) and 3D
The small spiculated lesion was missed or misinterpreted over years with 2D; this lesion was easy to identify with 2D (synthetic) and 3D, and was highly suggestive of malignancy (BI-RADS 5).
Recommendation
US biopsy recommended.
US
No internal US.
Histology
Invasive ductal carcinoma.
Further Imaging/Further Diagnostic
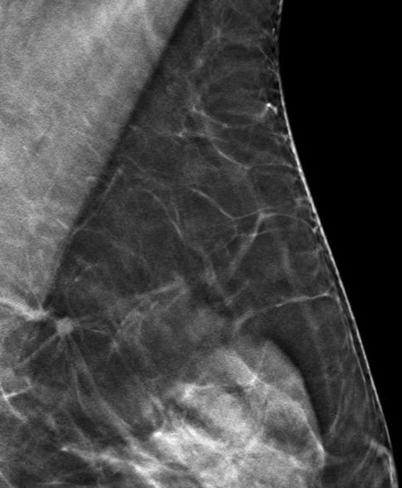
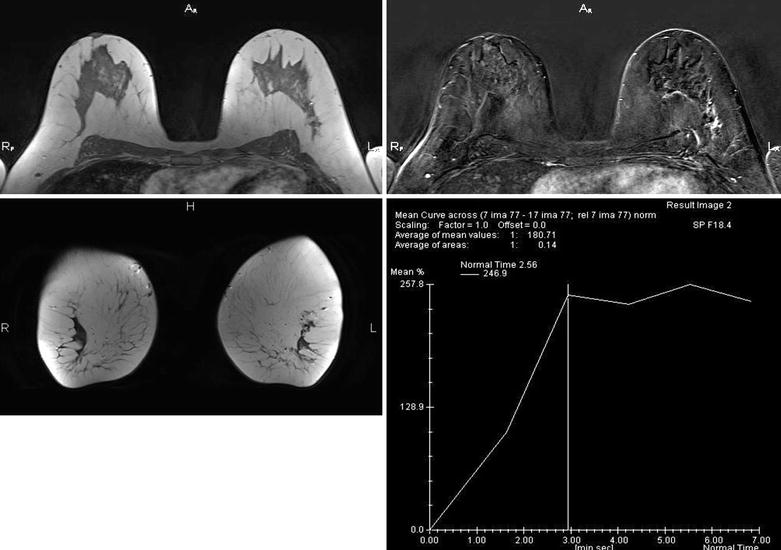
MRI recommended; on MRI (Fig. 3.20), there was an additional 16 mm breast cancer, missed with mammography.
Fig. 3.20
MRI
Comment
This case demonstrates malignant breast lesions not discovered over years with 2D. Discovered retrospectively with other imaging.
Image Interpretation Pearls
3D highlights masses and areas of architectural distortion.
3.3 Higher Accuracy of Diagnosis
3.3.1 Case 1
General Information/Clinical Issues
Patient was a 73-year-old female; noticed lump in the left breast.
Mammographic Analysis on 2D (Synthetic) and 3D
Breast density ACR II. On 2D in 2010 diffuse asymmetric density on the right side (Figs. 3.21a, b and 3.22a, b); BI-RADS 0. On 3D in Lcc irregular mass lateral in the left breast, findings not seen on 2D (Figs. 3.23 and 3.24 [3D magnification in cc, same figure as Fig. 3.23]); BI-RADS 5.
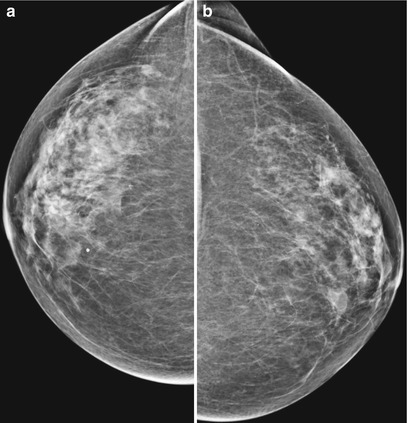
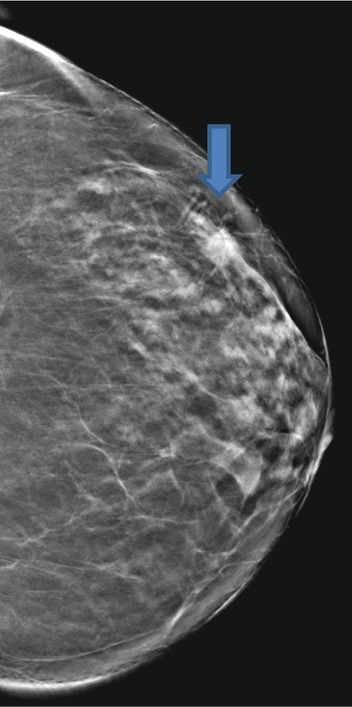
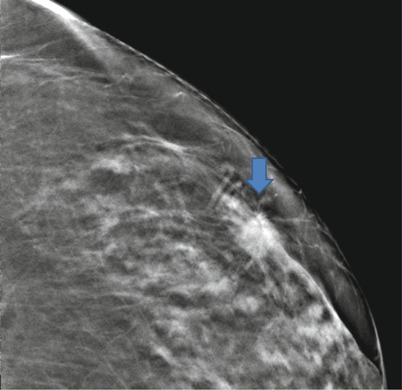
Fig. 3.21
(a, b) 2D and obl
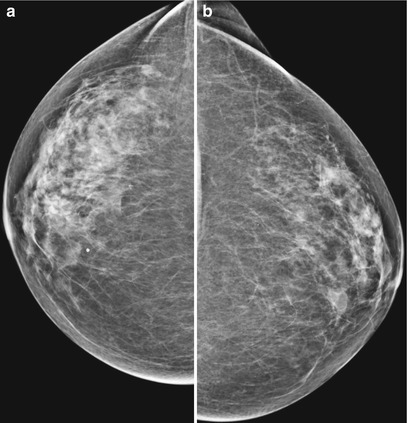
Fig. 3.22
(a, b) 2D and cc
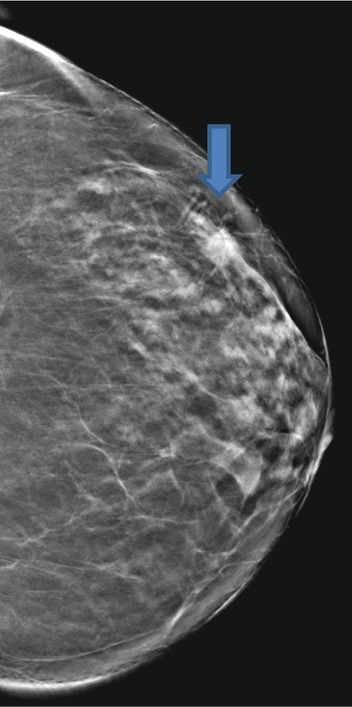
Fig. 3.23
3D cc
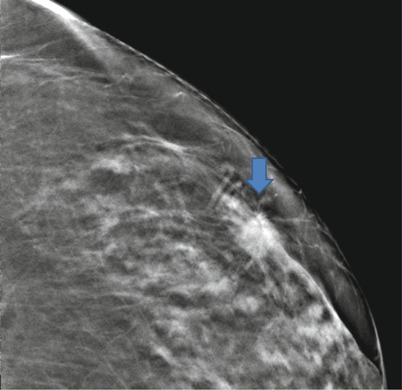
Fig. 3.24
Zoom 3D
Differential Diagnosis on 2D
Normal variation due to asymmetric involution (BI-RADS 0).
Conclusion/Diagnosis with 3D
2D findings were initially interpreted as negative, BI-RADS upgrade, highly suggestive of malignancy (BI-RADS 5).
Recommendation
US biopsy recommended.
US
External US (BI-RADS 5).
Histology
Invasive ductal carcinoma, pT1cpN1a (1/24)R0G2.
Further Imaging/Further Diagnostic
No preoperative MRI recommended in this case.
3.3.2 Case 2
General Information/Clinical Issues
Patient was a 51-year-old female, risk patient (grandmother with breast cancer); in 2011, there was a newly developed hemato-galactorrhea; on US in 2011 retromammillary duct ectasia was detected on the left side, and a papilloma may have been the underlying cause; on MRI in 2011 small cystic breast disease and a possible papilloma were detected at 3 o’clock on the left side; in February 2012, status after excision of a milk duct papilloma.
Mammographic Analysis on 2D, 2D (synthetic), and 3D
Breast density ACR III. On 2D in 2011, retrospective radial distortion in left breast latero-cranial with slightly higher density was seen in only one view (Lcc) (Figs. 3.25a, b and 3.26a, b); the initially recognized radial lesion is shown with 2D (synthetic) and 3D in 2013 (Figs. 3.27a, b, 3.28a, b, and 3.29 [3D magnification, same figure as 3.28a obl)]); BI-RADS 4.
Fig. 3.25
(a, b) 2D obl in 2011
Fig. 3.26
(a, b) 2D cc in 2011
Fig. 3.27
(a, b) 2D (synthetic) obl and cc in 2013
Fig. 3.28
(a, b) 3D in 2013 obl and cc
Differential Diagnosis on 2D
Complex sclerosing lesion, breast cancer.
Conclusion/Diagnosis with 3D;
BI-RADS upgrade, suggestive of malignancy (BI-RADS 4).
Recommendation
US biopsy recommended.
US
Histology
T-VAB invasive ductal carcinoma, Her2+.
Comment
3D is a powerful imaging modality for early breast cancer detection and increases the radiologist’s accuracy because there is reduced tissue overlap and structure noise on 3D. This leads to more confident readings and allows the more accurate evaluation of lesions. Accurate diagnosis is essential for optimal treatment.
Image Interpretation Pearls
On 2D the margins of the lesion in this case were not clearly seen and illustrate the challenge of cancer detection in heterogeneously dense breast tissue, especially in lesions with the same or lower density compared with the original breast tissue; 3D allows us to detect abnormalities that would have been very difficult to visualize on 2D.
3.4 Earlier Detection Rate
3.4.1 Case 1
General Information/Clinical Issues
Patient was a 62-year-old female; nodular findings retromamillary right side in 2013, follow-up mammograms from 2011 to 2013.
Mammographic Analysis on 2D, 2D (Synthetic), and 3D
Breast density ACR III; on 2D in 2011 (Fig. 3.33a, b) there was a retromamillary possible architectural distortion or radiating structure on the right side due to summation of breast tissue (BI-RADS 0); no suspicious lesion was found on additional US performed at this time. In 2013 2D (synthetic) and 3D showed a large spiculated retromamillary mass with associated grouped pleomorphic calcifications (Figs. 3.34a, b and 3.35a, b); BI-RADS 5. On 3D there was clear visibility of the indistinct, slightly radiating margins of the large mass (at least 4 cm in size; Fig. 3.35a); BI-RADS 5.
Fig. 3.33
(a, b) 2D (a) cc and (b) obl
Fig. 3.34
(a, b) 2D (synthetic) (a) cc and (b) obl
Fig. 3.35
(a, b) 3D (a) and (b) obl
Differential Diagnosis on 2D
With this modality, only a summation artifact (due to superimposed glandular breast tissue), radial scar, DCIS, lobular carcinoma in situ (LCIS), and breast cancer (BI-RADS 0) are identified.
Conclusion/Diagnosis with 3D
On 2D, seen in Fig. 3.33a, b, the existing pathology, shown with blue arrows, is nearly obscured by the overlapping tissues (with consequent delayed diagnosis); on 2D (synthetic) and 3D, findings are highly suggestive of malignancy (BI-RADS 5).
Recommendation
US biopsy recommended.
US
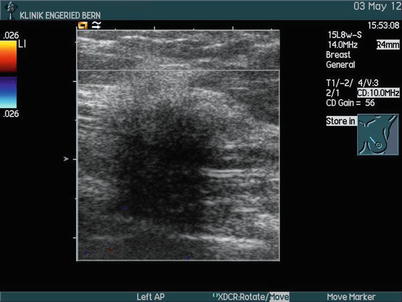
Large diffuse inhomogeneous hypoechoic infiltrative lesion (Fig. 3.36) retromammillary (BI-RADS 5).


Fig. 3.36
US
Histology
Invasive ductal carcinoma, moderately differentiated G2.
Further Imaging/Further Diagnostic
Preoperative MRI in this case. In cases of breast density ACR III or IV, MRI is recommended; look for common satellite lesions and axillary lymphadenopathy (Fig. 3.37).
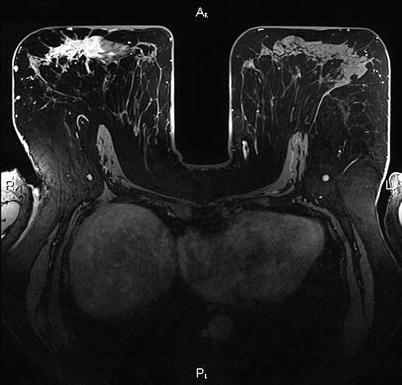
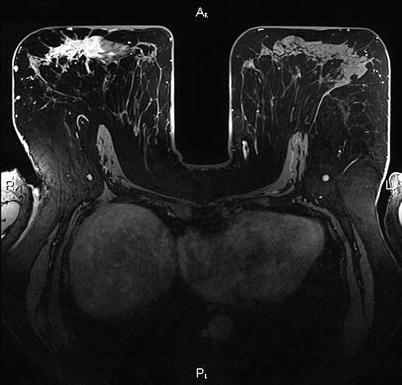
Fig. 3.37
MRI
3.4.2 Case 2
General Information/Clinical Issues
Patient was a 75-year-old female, on hormone replacement therapy, no signs or symptoms.
Mammographic Analysis on 2D (Synthetic) and 3D
Breast density ACR III. On 2D (Figs. 3.38a, b and 3.39) inhomogeneous glandular breast tissue, BI-RADS 0; on 3D clear visibility of a small (6 –7 mm) spiculated mass on the right side cranial close to the chest wall (Figs. 3.40 and 3.41 [3D magnification, same figure as 3.40 obl]); BI-RADS 5.
Fig. 3.38
(a, b) 2D obl
Fig. 3.39
(a, b) 2D cc
Fig. 3.40
3D obl
Fig. 3.41
3D magnification obl
Differential Diagnosis on 2D
Normal glandular breast tissue.
Conclusion/Diagnosis with 3D
The appropriate cross-sectional 3D slice allows clear visualization of the spiculated lesion, with BI-RADS upgrade, highly suggestive of malignancy (BI-RADS 5).
Recommendation
US biopsy recommended.
US
No internal US.
Histology
Invasive lobular carcinoma, moderately differentiated G2.
Further Imaging/Further Diagnostic
Preoperative MRI in this case shows a second even greater lesion (Fig. 3.42). MRI is recommended in lobular breast cancer or in cases of breast density ACR III or IV; look for common satellite lesions and axillary lymphadenopathy.
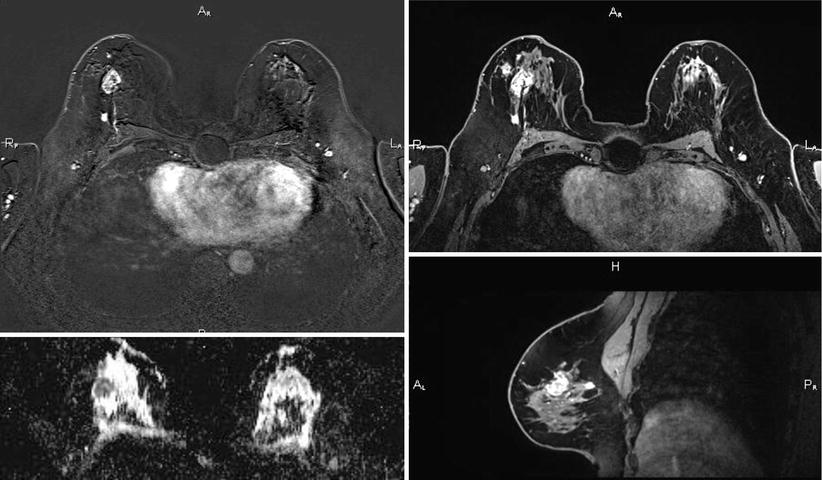
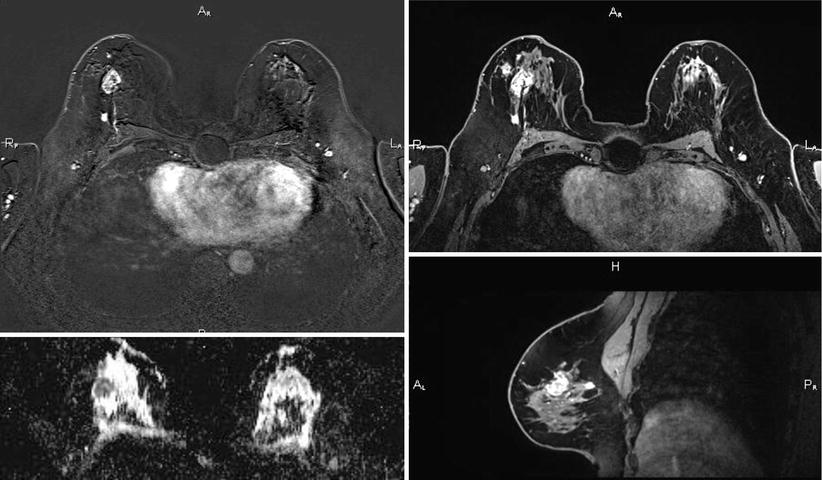
Fig. 3.42
MRI
Comment
These cases demonstrate why we expect earlier and improved cancer detection rates and higher positive predictive values for a biopsy recommendation with the use of this technology. The earlier detection of small cancers leads to lower treatment costs (less chemotherapy) and better chance of recovery.
Image Interpretation Pearls
On 3D the thin slices provide good visibility of lesions because of the reduction of structure noise.
See also Case 8.1.7: in Chap. 8 Tomoguided interventions/indications and advantages.
3.5 Better Delination of Tumor Size and Margins
3.5.1 Case 1
General Information/Clinical Issues
Patient was a 55-year-old female, screening, no signs or symptoms
Mammographic Analysis on 2D and 3D
Breast density ACR III. On 2D architectural distortion (15 mm) cranial right side without calcifications (Fig. 3.43a, b); BI-RADS 4. 3D demonstrates the spiculated margins of a clear mass that is now sharper (Figs. 3.43a, b and 3.44a, b). 3D magnification is shown in Fig. 3.45a, b (same figure as 3.43a, b); BI-RADS 5.
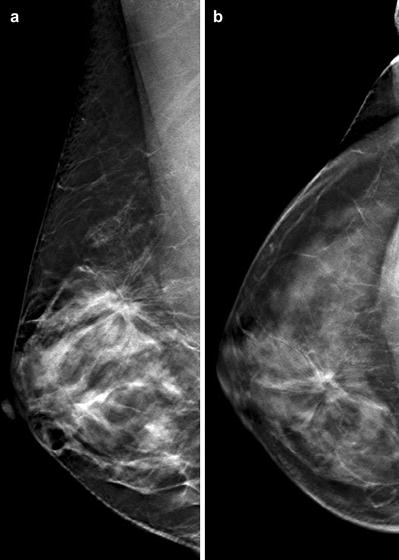
Fig. 3.43
(a, b) 2D (a) obl and (b) cc
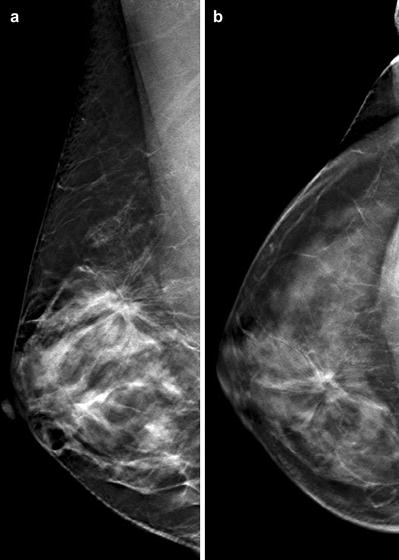
Fig. 3.44
(a, b) 3D (a) obl and (b) cc
Differential Diagnosis on 2D
Radial scar, complex sclerosing lesion, breast cancer.
Conclusion/Diagnosis with 3D
BI-RADS upgrade, highly suggestive of malignancy (BI-RADS 5).
Recommendation
US biopsy recommended.
US
No internal US.
Histology
Invasive ductal carcinoma pT1b, pN0, pMX, R0, G2.
Further Imaging/Further Diagnostic
No preoperative MRI in this case; in cases of breast density ACR III or IV, MRI is recommended; look for common satellite lesions and axillary lymphadenopathy.
3.5.2 Case 2
General Information/Clinical Issues
Age 45 years, left retromammillary 5 cm large palpable tumor and palpable axillary lymph nodes.
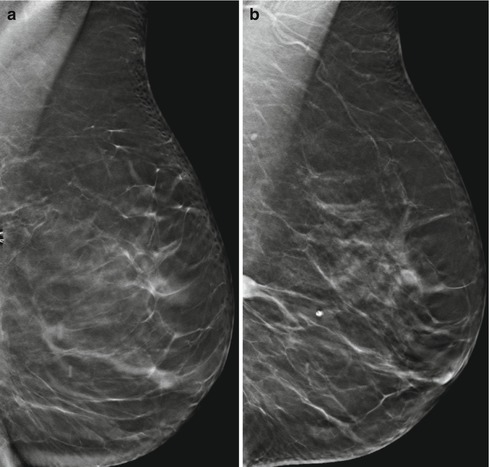
Mammographic Analysis on 2D and 3D
Breast density ACR III. On 2D diffuse asymmetric density retromamillary and latero-cranial left side with associated grouped pleomorphic calcifications and suspicious 3 cm large axillary lymph node (Fig. 3.46a, b); BI-RADS 4. On 3D clear visibility of the indistinct, slightly radiating margins of the large mass of at least 4 cm (Figs. 3.47a, b and 3.48 [2D magnification] and Fig. 3.46 [3D magnification,same figures as Figs 3.46a and 3.47a])); BI-RADS 5.
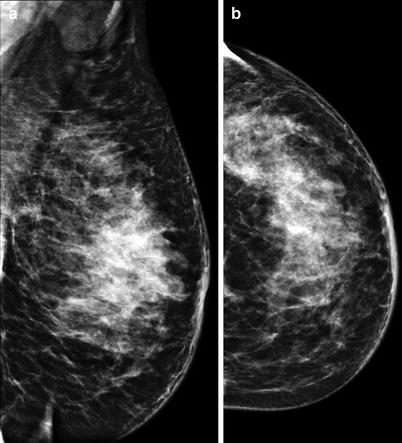
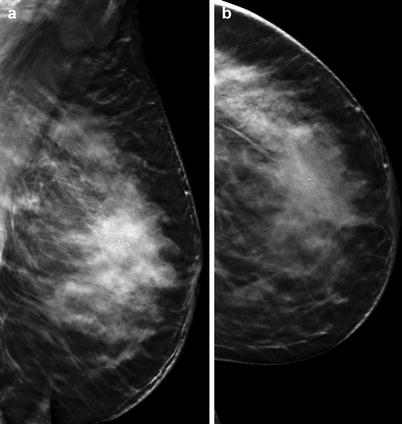
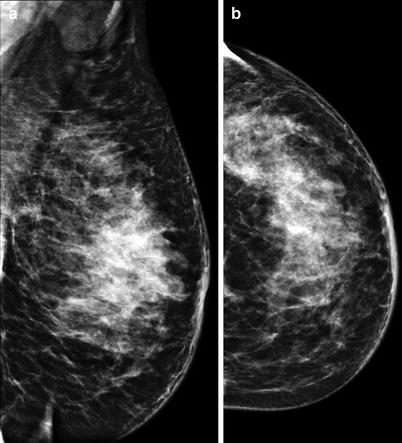
Fig. 3.46
(a, b) 2D (a) obl and (b) cc
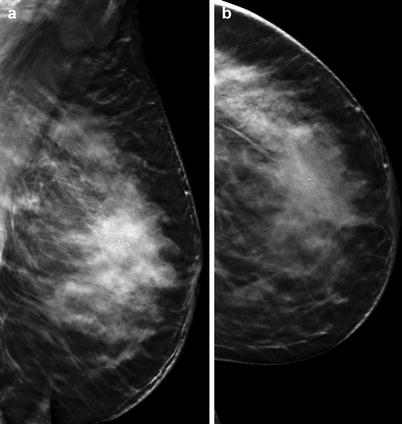
Fig. 3.47
(a, b) 3D (a) obl and (b) cc
Differential Diagnosis on 2D
Complex sclerosing lesion, breast cancer.
Conclusion/Diagnosis with 3D
BI-RADS upgrade, highly suggestive of malignancy (BI-RADS 5).
Recommendation
US biopsy recommended.
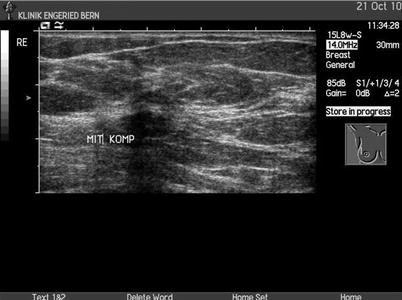
US
Large diffuse inhomogeneous hypoechoic infiltrative lesion (Fig. 3.50) retromammillary (BI-RADS 5).
Fig. 3.50
US
Histology
Invasive ductal carcinoma, moderately differentiated G2.
Further Imaging/Further Diagnostic
No preoperative MRI in this case; in cases of breast density ACR III or IV, MRI is recommended; look for common satellite lesions and axillary lymphadenopathy.
Comment
Because of the reduced tissue overlap and structure noise on 3D, objects are better visualized, with improved clarity. 3D facilitates the marginal analysis of mass lesions. This leads to more confident readings and allows the more accurate evaluation of lesions.
Image Interpretation Pearls
On 2D breasts are compressed to reduce tissue overlap, with known limitations especially in dense glandular tissue. On 3D the thin slices provide good visibility of lesions because of the reduction of structure noise. 3D is better for the delineation/demarcation of the margins of breast tumors because it reduces overlapping normal breast tissue.
3.6 Upgrade of BI-RADS
3.6.1 Case 1
General Information/Clinical Issues
Patient was a 76-year-old female; she had a 1.5 cm palpable lump medial left side.
Mammographic Analysis 2D (synthetic) and 3D
Breast density ACR II. On 2D (synthetic) in side-to-side comparison, there was an asymmetric density craniomedial at the 10 o’clock position close to the chest wall, with associated monomorphic microcalcifications (Fig. 3.51a–d); BI-RADS 0. On 3D in both views there was a 2 cm large fat-containing mass with desmoplastic reaction (Figs. 3.52a, b, 3.53 and 3.54 [3D magnification, same figure as 3.52a, b]); BI-RADS 4.
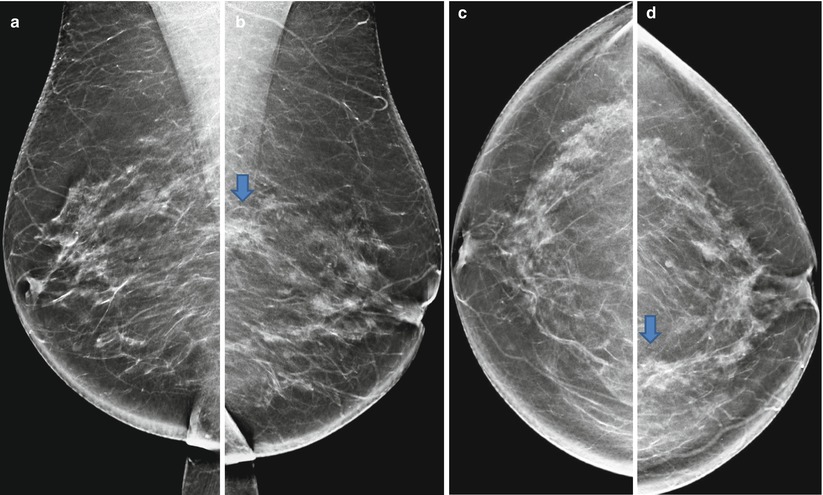
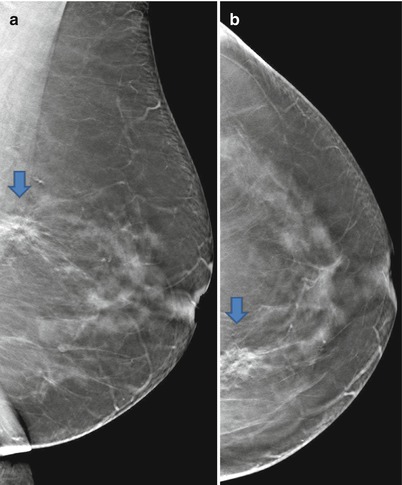
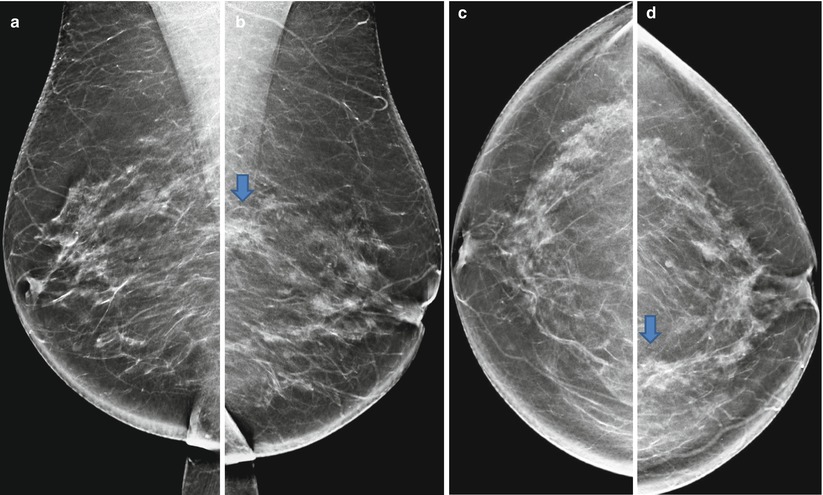
Fig. 3.51
(a, b) 2D synthetic (a) obl and (b) obl. (c, d) 2D synthetic (c) cc and (d) cc
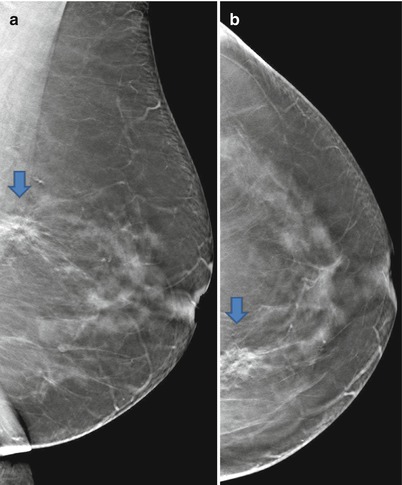
Fig. 3.52
(a, b) 3D (a) obl and (b) cc
Differential Diagnosis on 2D
Normal fat-containing breast tissue, lymph node, fibroadenoma, DCIS, invasive breast cancer (BI-RADS 0).
Conclusion/Diagnosis with 3D
An abnormality was detected on 2D, but the malignant characteristics of the lesion were clearly defined with 3D, suggestive of malignancy (BI-RADS 4). Cave: lobular carcinoma can also contain fat.
Recommendation on 2D
Spot view or 3D, US with biopsy or T-VAB.
Recommendation on 3D,
US with biopsy or T-VAB.
Histology
Invasive lobular carcinoma, pT1c pN0 G2 R0.
Further Imaging/Further Diagnostic
No preoperative MRI.
3.6.2 Case 2
General Information/Clinical Issues
Patient was a 62-year-old female; no signs or symptoms, external fine needle biopsy FNA or FNAC in November 2009 revealed cystic mastopathy with epithelial atypia.
Mammographic Analysis 2D and 3D
Breast density ACR I. On 2D nonspecific convex ill-defined 10 mm density craniolateral on right side (Figs. 3.56a, b and 3.57a, b); BI-RADS 0; on 3D in Lcc, there was a visible 10 mm lobulated mass with desmoplastic reaction (Fig. 3.58a, b [3D magnification, same figure as 3.58a]); BI-RADS 4.
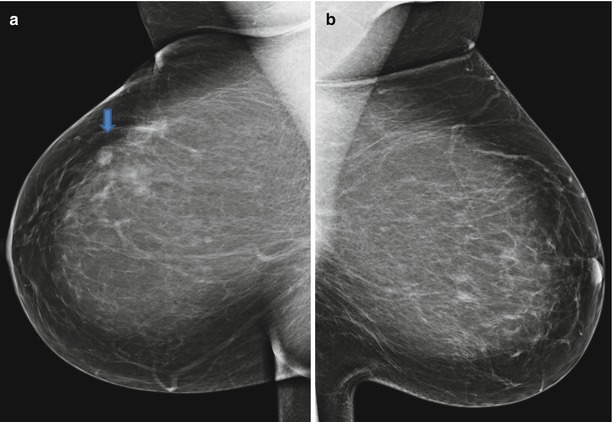
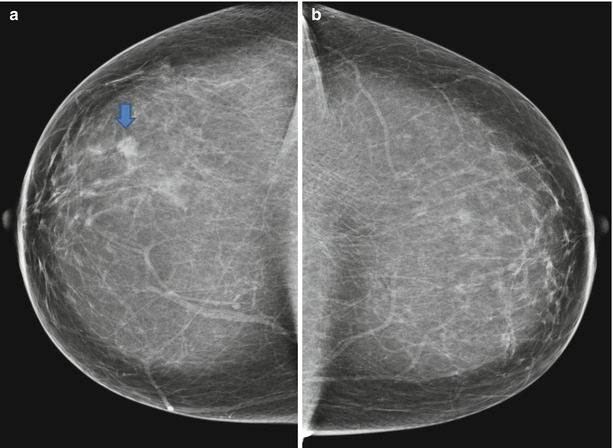
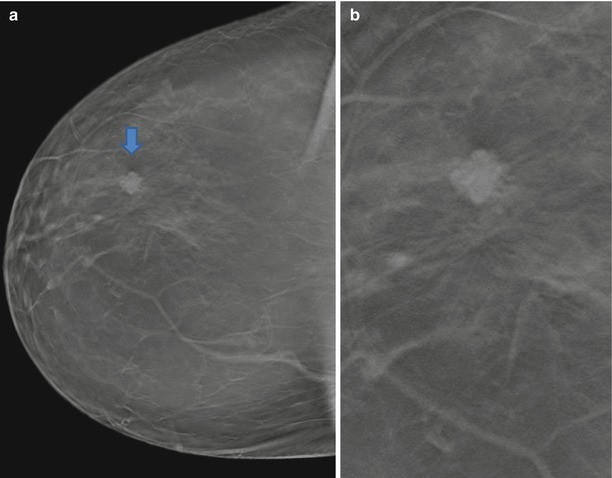
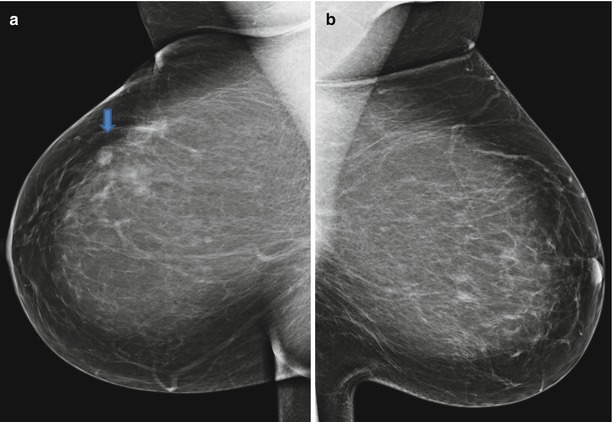
Fig. 3.56
(a, b) 2D (a) and and (b) in obl
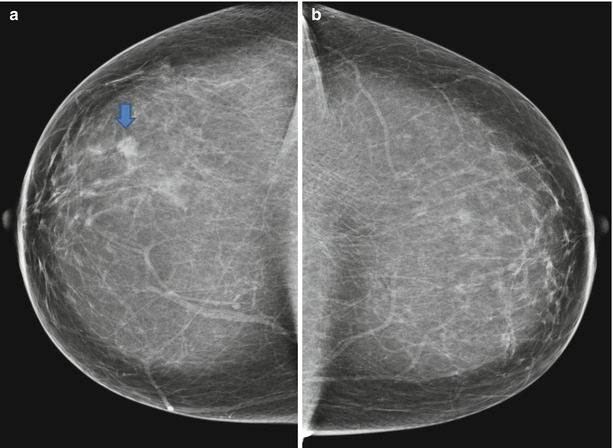
Fig. 3.57
(a, b) 2D (a) and (b) in cc
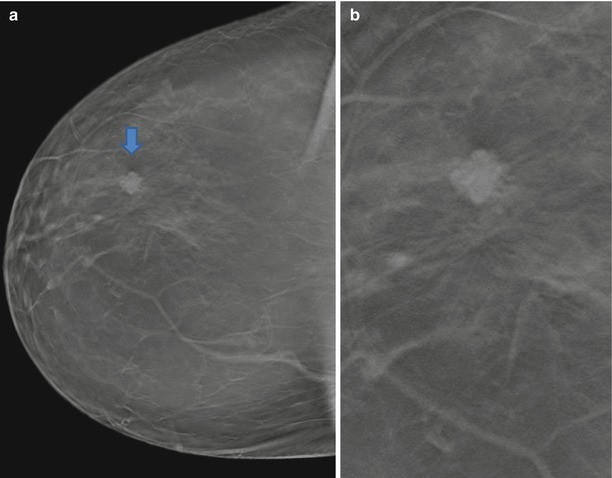
Fig. 3.58
(a, b) 3D cc and magnification cc
Differential Diagnosis on 2D
Cyst, lymph node, fibroadenoma, DCIS, invasive breast cancer (BI-RADS 0).
Conclusion/Diagnosis with 3D
Allows precise localization of a breast change and significantly improves diagnostic accuracy of non-calcified lesions compared with 2D, suggestive of malignancy (BI-RADS 4).
Recommendation on 2D
Spot view or 3D: US.
Recommendation on 3D
US biopsy or T-VAB.
US
Vertically orientated 15 × 10 mm hypoechoic lesion (Fig. 3.59) with hyperechoic rim and discrete sound attenuation dorsally at 10 o’o’clock (BI-RADS 5).
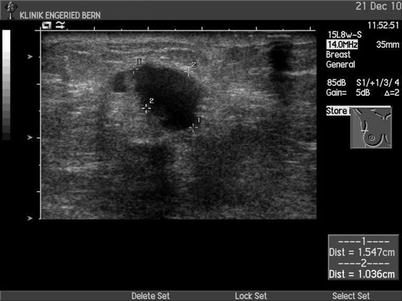
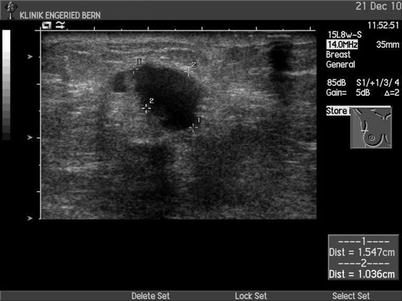
Fig. 3.59
US
Histology
pT1cN1a(1/2)(sn) R0 G2.
Further Imaging/Further Diagnostic
No preoperative MRI recommended.
Comment
3D, compared with 2D, allows better differentiation between benign and malignant lesions; BI-RADS upgrade and downgrade is possible on 3D. If an only-one-view finding is detected on 3D, this finding has to be biopsied.
Image Interpretation Pearls
2D imaging has limitations, especially in heterogeneously dense breast tissue. True lesions can be obscured due to the superposition of normal breast tissue; a summation artifact can simulate a true lesion, and asymmetric density can be caused by lobular carcinomas or by a normal variation. 3D is very helpful in the work-up of 2D-detected abnormalities. Look for desmoplastic reactions, architectural distortions, mass, and associated calcifications on 3D.
3.7 Exact Localization and Exact Depth of the Lesion
3.7.1 Case 1
General Information/Clinical Issues
Patient was a 71-year-old female; screening mammography detected a suspicious lesion on the left side; an externally performed US-guided core biopsy did not confirm a malignant lesion.
Mammographic Analysis on 2D (Synthetic) and 3D
Breast density ACR II. On 2D there was an ill-defined centrally located lesion (Fig. 3.60a, b); BI-RADS 4. On 3D there was a centrally located spiculated 15 mm mass with different densities without associated grouped calcifications (Fig. 3.61a, b); BI-RADS 5.
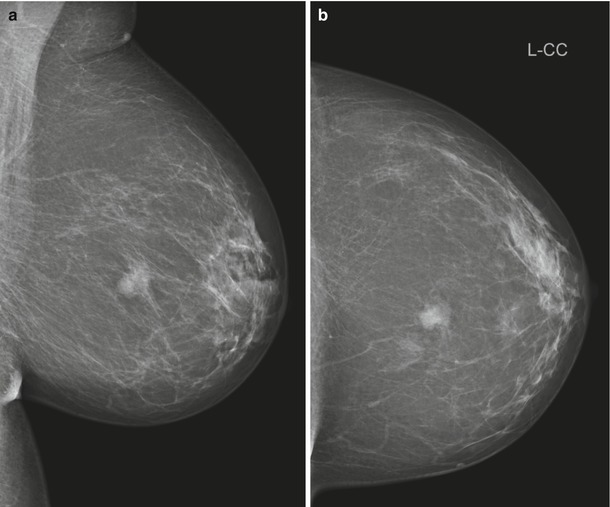
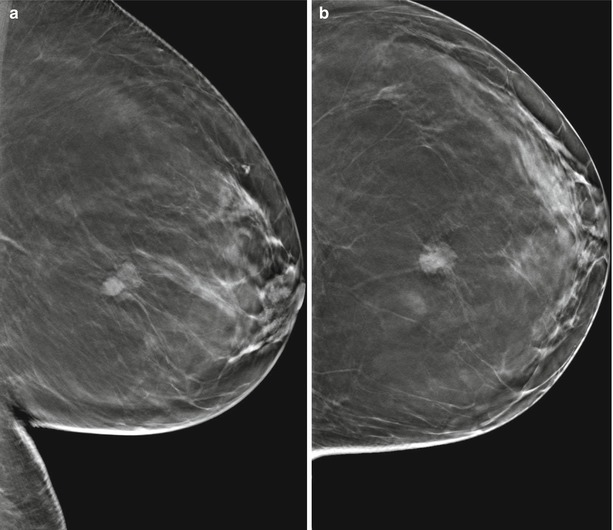
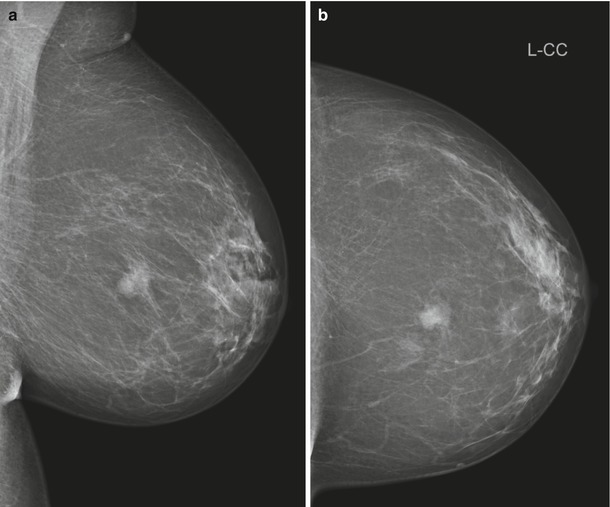
Fig. 3.60
(a, b) 2D cc
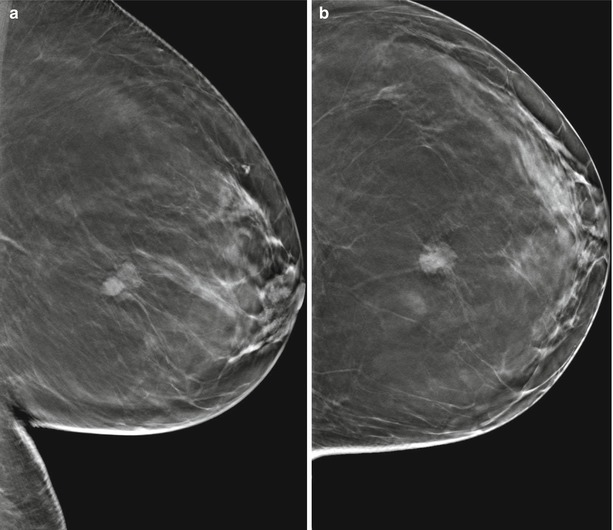
Fig. 3.61
(a, b) 3D (a) obl and (b) cc
Differential Diagnosis on 2D
Complex sclerosing lesion, breast cancer (BI-RADS 4).
Conclusion/Diagnosis with 3D
Highly suggestive of malignancy (BI-RADS 5).
Recommendation
US biopsy recommended.
US
Lesion is occult on US; US was carried out at different times by a total of three experienced sonographers (BI-RADS 0)., Finally T-VAB (Fig. 3.62a–c) was performed.
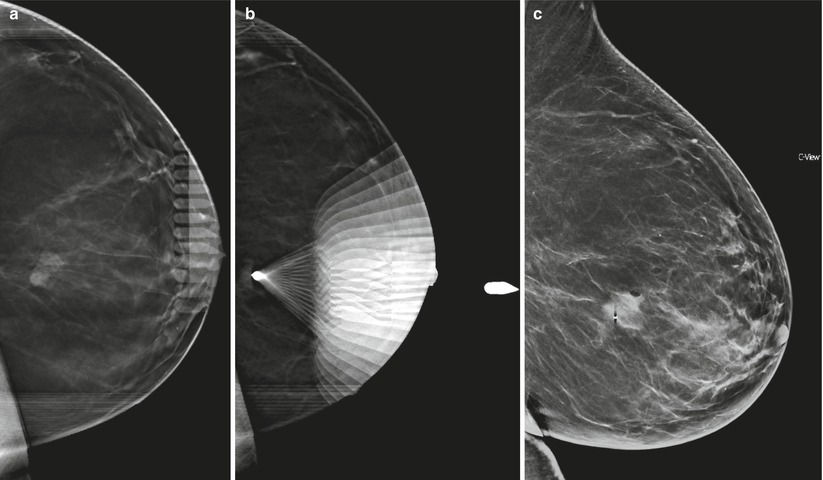
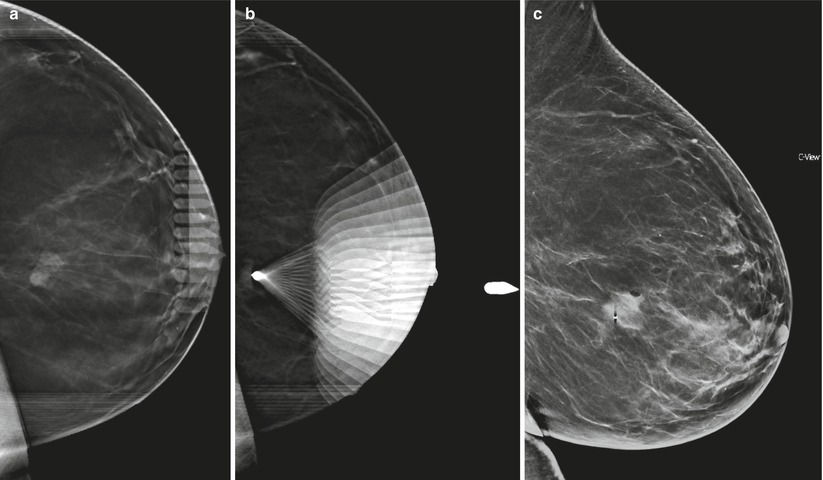
Fig. 3.62
(a, b) 3D T-VAB. (c) 2D (synthetic) ml
Histology After T-VAB
Poorly differentiated adenocarcinoma of ductal type with lobular cancerization.
Further Imaging/Further Diagnostic
No preoperative MRI in this case; in cases of breast density ACR III or IV, MRI is recommended.
3.7.2 Case 2
General Information/Clinical Issues
Patient was a 61-year-old female; mother and grandmother with breast cancer.
Mammographic Analysis 2D and 3D
Breast density ACR II. On 2D in Lcc projection in side-to-side comparison, there was a nonspecific convex ill-defined 6 mm density in the retroglandular clear space lateral; in Lobl view on 2D this was not visible, and there were no prior images (Fig. 3.63a, b); BI-RADS 0. On 3D in both views there was a visible 6 mm stellate mass without calcifications (Figs. 3.64a, b and 3.65[3D magnification, same figure as Fig. 3.64a]); BI-RADS 5.
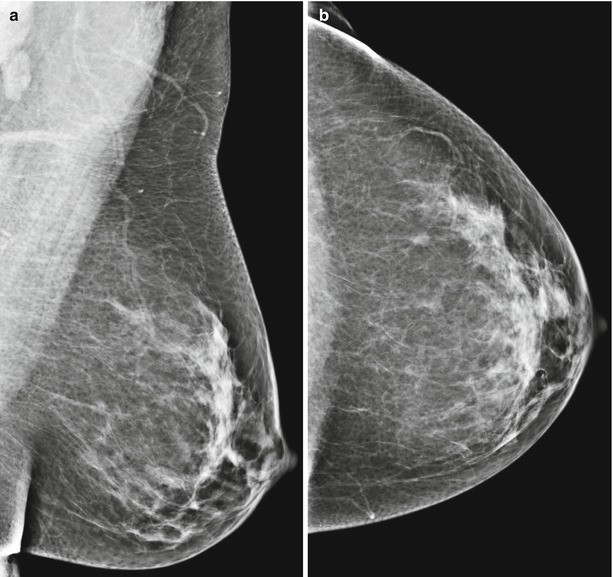
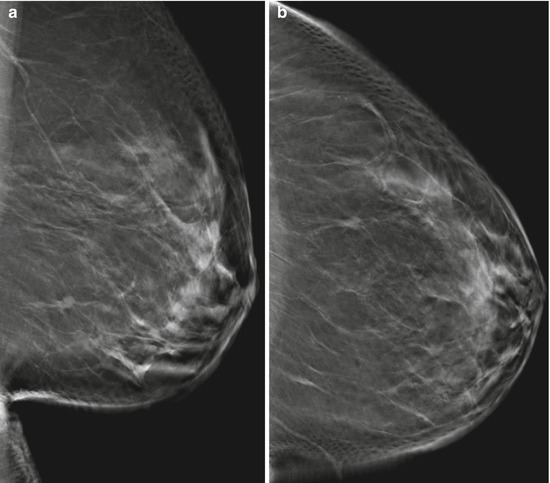
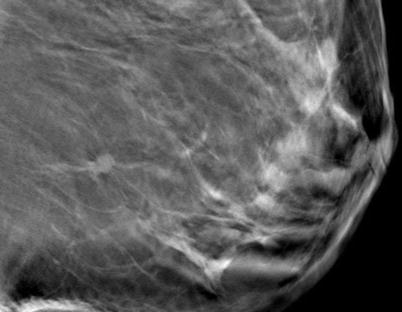
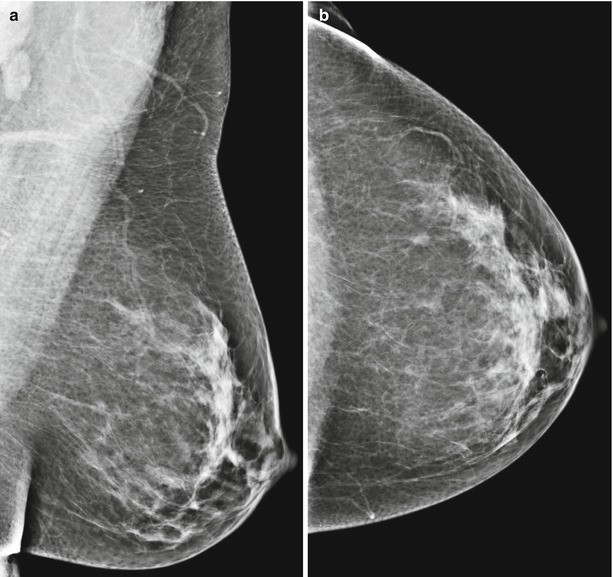
Fig. 3.63
(a, b) 2D (a) Lobl and (b) Lcc
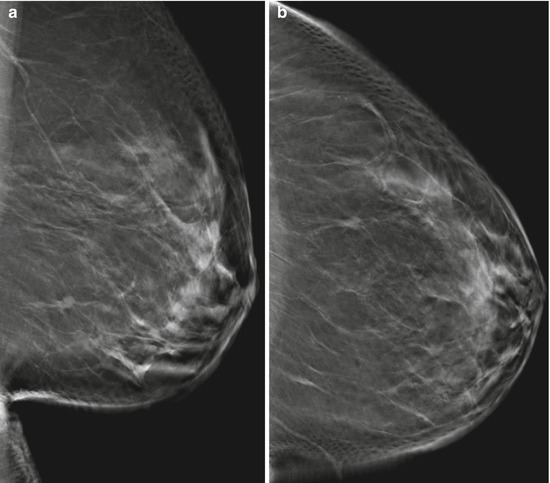
Fig. 3.64
(a, b) 3D (a) Lobl and (b) Lcc
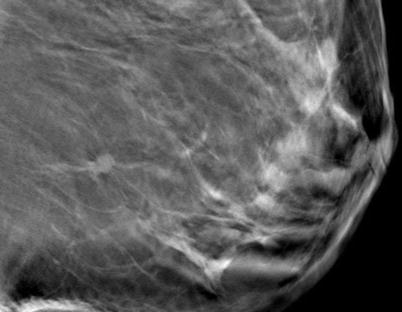
Fig. 3.65
3D magnification Lobl
Differential Diagnosis on 2D
Normal fat-containing breast tissue, lymph node, fibroadenoma, DCIS, invasive breast cancer (BI-RADS 0).
Conclusion/Diagnosis with 3D
Allows precise localization of a breast change and significantly improves diagnostic accuracy of non-calcified lesions compared with supplemental 2D diagnostic views, highly suggestive of malignancy (BI-RADS 5).
Recommendation
On 2D spot view or 3D, US with or without biopsy or T-VAB.
Recommendation
On 3D,US biopsy or T-VAB.
US
Occult, T-VAB recommended.
Histology
Invasive ductal carcinoma, G2.
Further Imaging/Further Diagnostic
No preoperative MRI recommended.
3.7.3 Case 3
(See Chap. 6: Malignant changes: location lesion Case 7)
General Information/Clinical Issues
Patient was a 68-year-old female; no signs or symptoms.
Mammographic Analysis on 2D and 2D (Synthetic) and 3D
Breast density ACR II. On 2D no suspicious lesion in 2012 (Fig. 3.66a, b); BI-RADS 1; new ill-defined asymmetrical density close to the chest wall on follow-up 2D (synthetic) in 2014 (Fig. 3.67a, b); BI-RADS 4. The expected location of the lesion is medial on 2D.
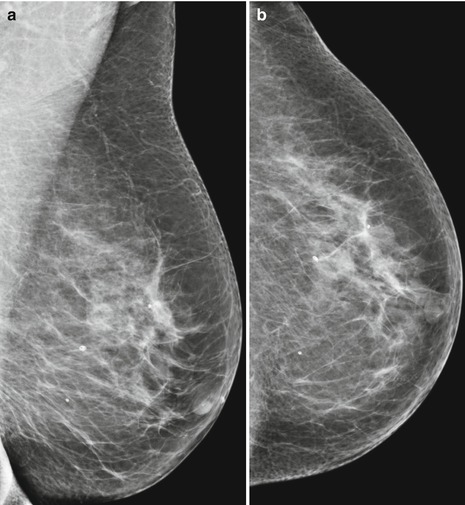
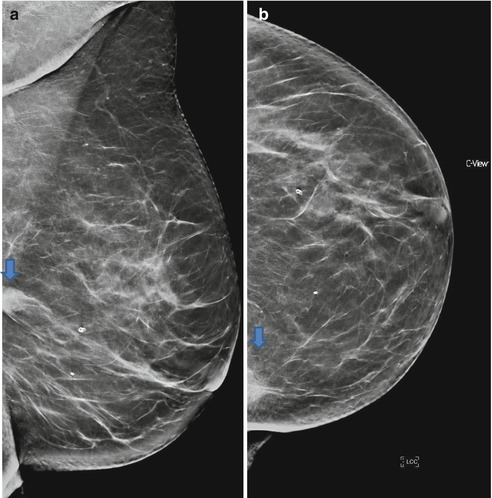
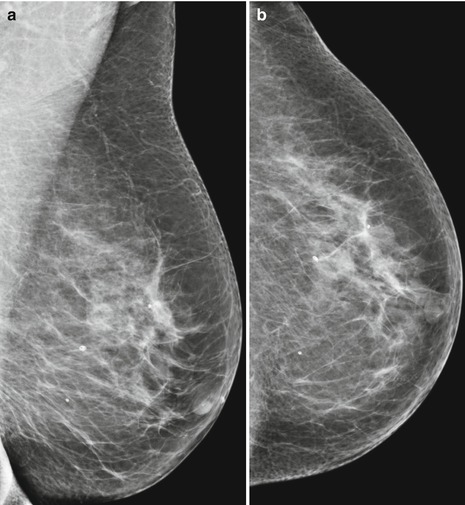
Fig. 3.66
(a, b) 2D (a) obl and (b) cc
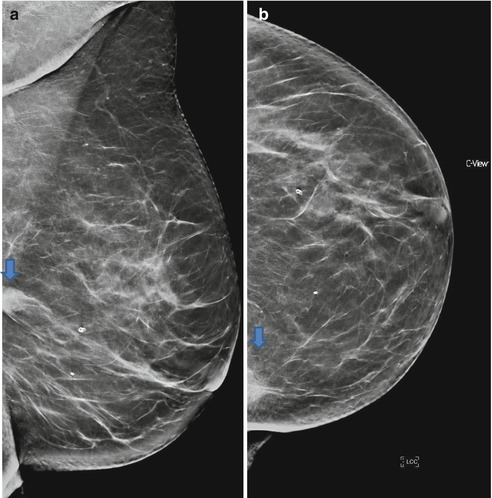
Fig. 3.67
(a, b) 2D (synthetic) (a) obl and (b) cc
Differential Diagnosis on 2D (Synthetic)
Nodular fasciitis, DCIS, invasive breast cancer (BI-RADS 4).
Conclusion/Diagnosis with 3D
The assignment/location of the lesion was performed incorrectly in the mammographic report on 2D, the asymmetric medial density was caused by the musculus pectoralis (Fig. 3.68). 3D control of the inserted clip after US-guided biopsy (Fig. 3.70) shows that the lesion is located laterally (Fig. 3.71a, b); lesion is suggestive of malignancy (BI-RADS 4).
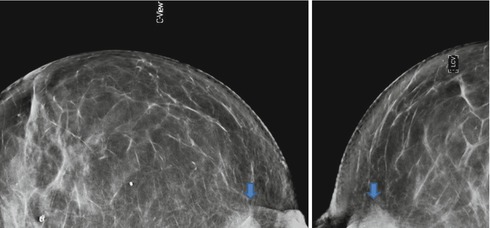
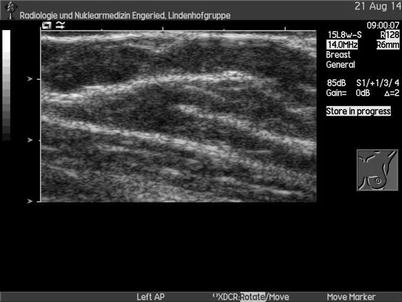

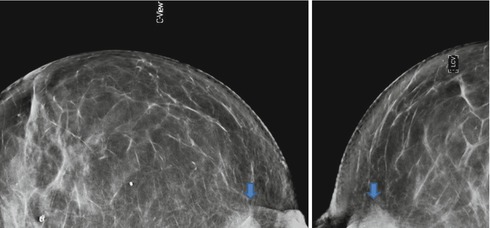
Fig. 3.68
2D cleavage view
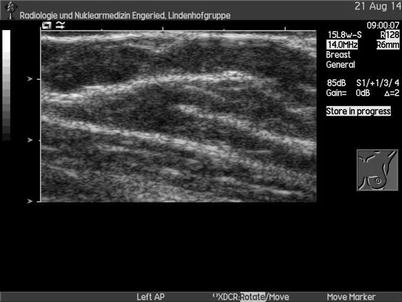
Fig. 3.69
US

Fig. 3.70
US
Recommendation
US biopsy recommended.
US
Subsequent targeted US was performed, which showed no obvious suspicious medial lesion (Fig. 3.69); US-guided biopsy of a questionable hypoechoic area medially in the breast was performed with additional clip marking (Fig. 3.70); second-look US shows an ill-defined hypoechoic lateral lesion (Fig. 3.72) after 3D control of the inserted clip.
Histology
Invasive lobular carcinoma, moderately differentiated G2.
Further Imaging/Further Diagnostic
No preoperative MRI in this case; in cases of breast density ACR III or IV, MRI is recommended; look for common satellite lesions and axillary lymphadenopathy.
Comment
3D provides more precise lesion localization compared with 2D. Subsequent targeted US was performed in the first two cases, but the detected lesions in 3D were sonographically not depictable. These cases illustrate the role of 3D and T–VAB in the diagnostic work-up of recalled patients.
Image Interpretation Pearls
3D determines (similarly to MRI) the exact localization of lesions in the breast; therefore, a second-look US is, in many cases, helpful in the diagnostic work-up of suspicious lesions.
3.8 One-View-Only Findings
3.8.1 Case 1
General Information/Clinical Issues
Patient was a 61-year-old female; mother and grandmother with breast cancer.
Mammographic Analysis 2D and 3D
Breast density ACR II. On 2D in Lcc projection (Fig. 3.73a, b) in side-to-side comparison, there was a nonspecific convex ill-defined 6 mm density in the retroglandular clear space lateral. 2D Lobl shows no abnormality, and there were no prior images (Fig. 3.74a, b); BI-RADS 0. On 3D, there was enhanced visibility of a 6 mm stellate mass without calcifications in both views (Figs. 3.75a, b and 3.76 [3D magnification, same figure as 3.75b]); BI-RADS 5.

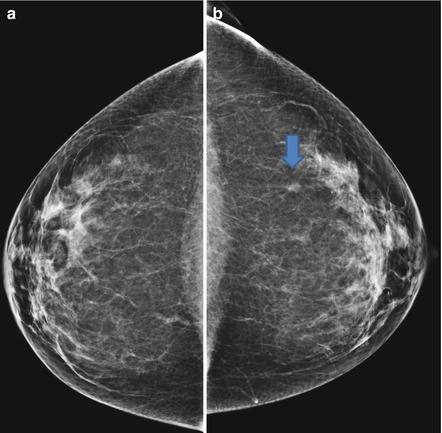
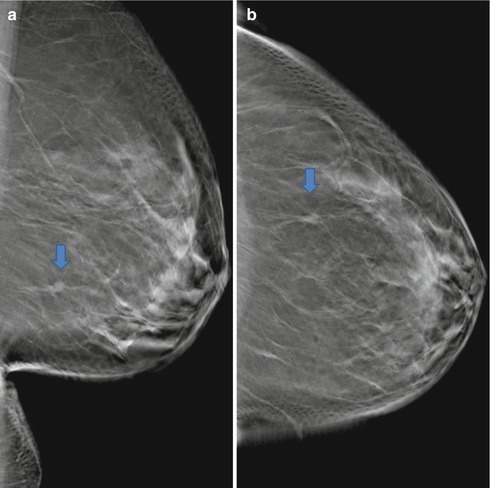
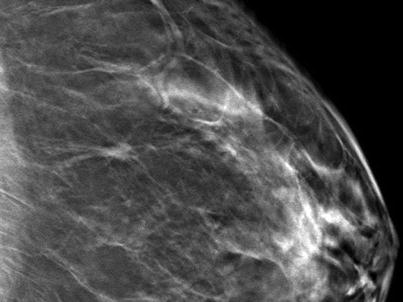

Fig. 3.73
(a, b) 2D (a) and (b) in obl
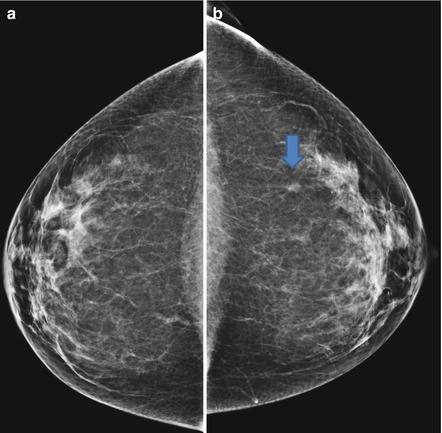
Fig. 3.74
(a, b) 2D (a) and (b) in cc
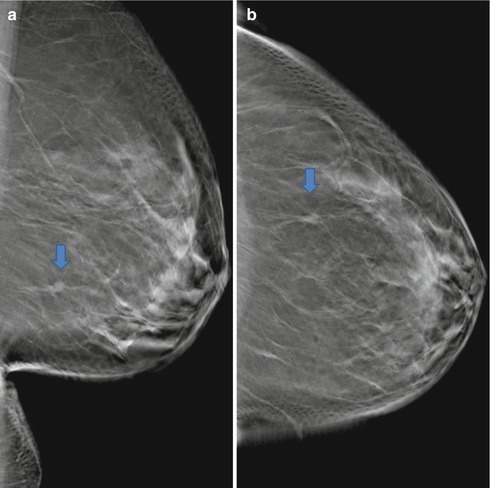
Fig. 3.75
(a, b) 3D (a) obl and (b) cc
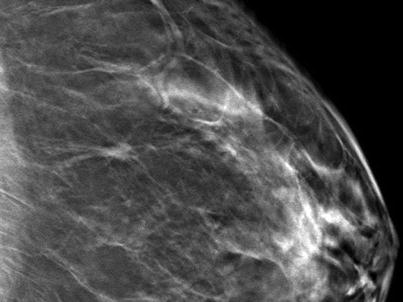
Fig. 3.76
3D magnification Lcc
Differential Diagnosis on 2D
Normal fat-containing breast tissue, lymph node, fibroadenoma, DCIS, invasive breast cancer (BI-RADS 0).
Conclusion/Diagnosis with 3D
Allows precise localization of a breast change and significantly improves diagnostic accuracy of non-calcified lesions, due to clear visible margins of the lesion, compared with 2D; highly suggestive of malignancy (BI-RADS 5).
Recommendation
On 2D spot view or 3D, US with or without biopsy or stereotactic guided vacuum assisted biopsy (S-VAB).
Recommendation
On 3D,US biopsy or T-VAB.
Histology
Invasive ductal carcinoma, G2.
Further Imaging/Further Diagnostic
S-VAB biopsy, no preoperative MRI.
Comment
3D is very helpful in the work-up of density asymmetries; look for architectural distortions, mass, and associated calcifications; 3D reduces false positives. When an only-one-view finding is detected on 3D, this finding has to be biopsied.
Image Interpretation Pearls
Compare images with prior mammograms if available; consider a normal variation as a cause of focal asymmetry (such as fat-containing lesions; cave: lobular carcinoma can also contain fat); especially in dense breast tissue the lesion can be obscured due to the superposition of normal breast tissue; a summation artifact can simulate a true lesion; consider that the anatomical location of a lesion can exclude detection in the second view.
See Chap. 6. Malignant changes: one-view-only findings.
3.9 Diagnostic Work-up Spot View vs. Digital Breast Tomosynthesis
3.9.1 Case 1
General Information/Clinical Issues
Patient was a 69-year-old female; screening; no signs or symptoms; no previous mammography (MG).
Mammographic Analysis on 2D and 2D (Synthetic) and 3D
Breast density ACR III. On 2D radial distortion retromamillary right side in obl view (Fig. 3.78a) with possible not obvious correlate in cc view central retromamillary (Fig. 3.78b); BI-RADS 4. On 2D (synthetic) and 3D the radial distortion was caused by a summation effect (Figs. 3.79a, b and 3.80a, b); this result also shows the spot view (Fig. 3.81a, b); BI-RADS 1.
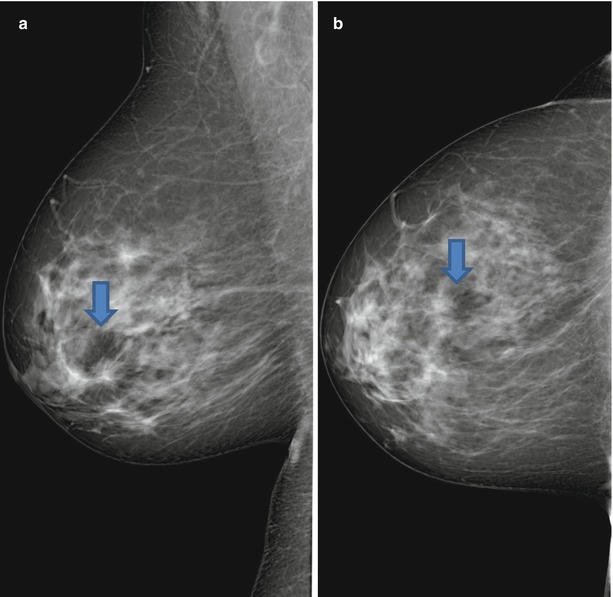
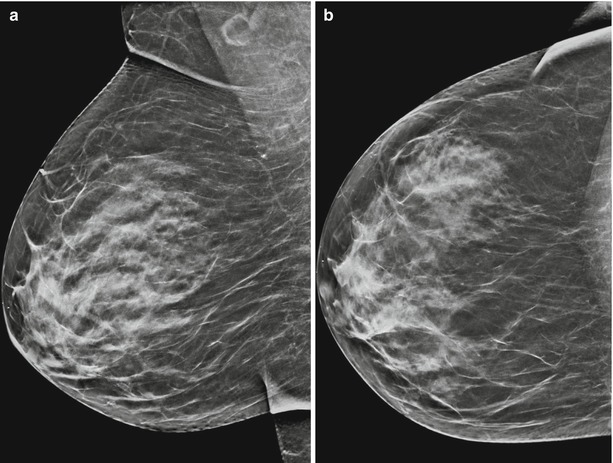
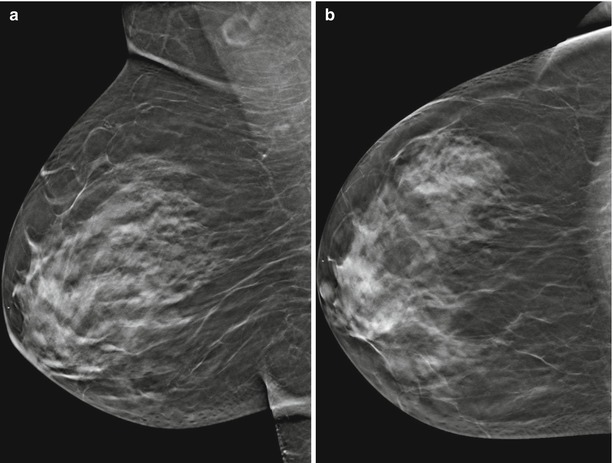
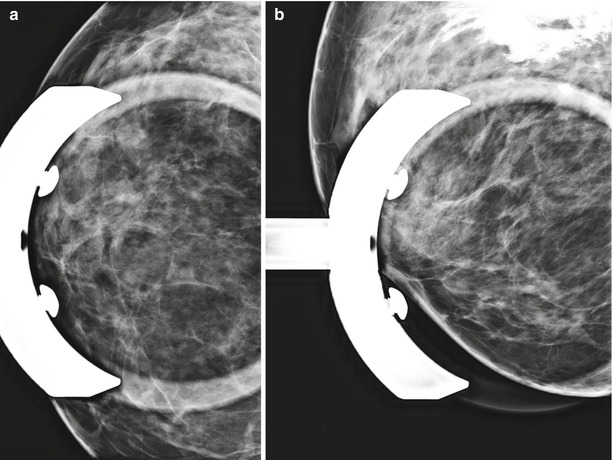
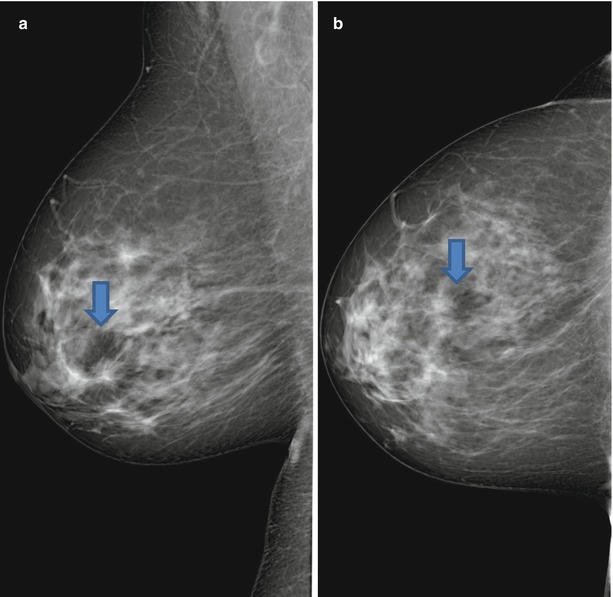
Fig. 3.78
(a, b) 2D (a) obl and (b) cc
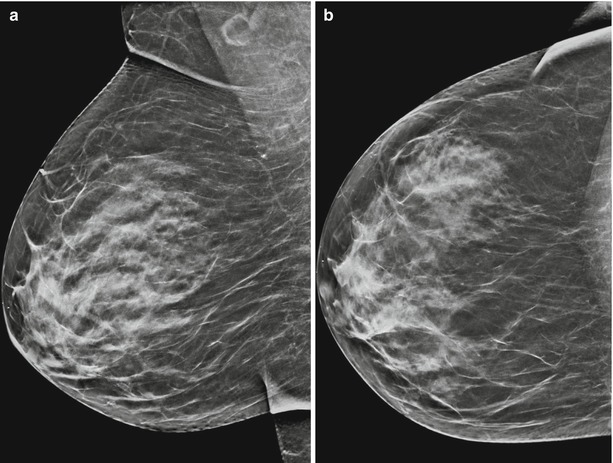
Fig. 3.79
(a, b) 2D (synthetic) (a) obl and (b) cc
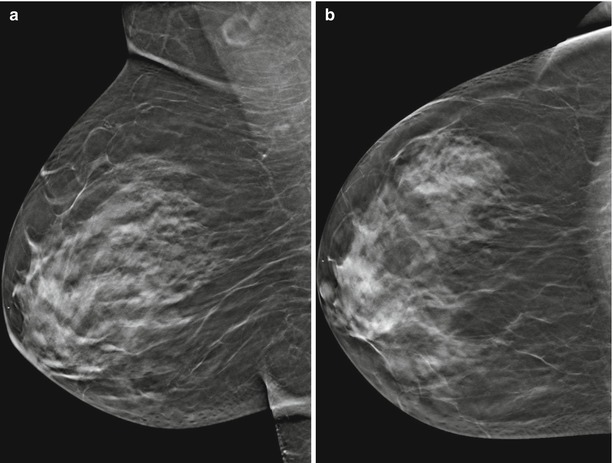
Fig. 3.80
(a, b) 3D (a) obl and (b) cc
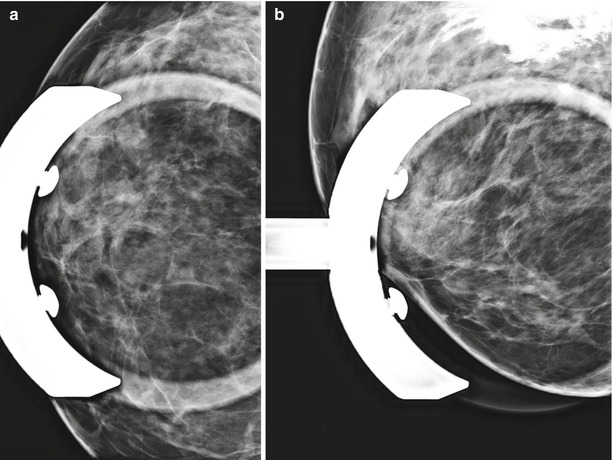
Fig. 3.81
(a, b) Spot view
Differential Diagnosis on 2D
Complex sclerosing lesion, breast cancer (BI-RADS 4).
Conclusion/Diagnosis with 2D (Synthetic) and 3D
BI-RADS downgrade, normal breast tissue (BI-RADS 1).
Recommendation
Spot views or 3D; previously, for the diagnostic work-up of a suspicious lesion a spot view was conducted, today 3D is at least equivalent.
US
No internal.
Histology
−
Further Imaging/Further Diagnostic
In case of doubt a follow-up is optional.
3.9.2 Case 2
General Information/Clinical Issues
Patient was a 66-year-old female; screening; clinically no signs or symptoms, no previous MG.
Mammographic Analysis on 2D (Synthetic) and 3D
Breast density ACR I. On 2D (synthetic) 6 mm-wide nonspecific irregular density (lesion I) on the right side lateral, and grouped amorphic calcifications (lesion II) medial (Fig. 3.82a, b); BI-RADS 0. On 3D grouped amorphic calcifications medial and more clearly distinguishable indistinct margins of the lateral irregular density (Figs. 3.83a, b and 3.84 [3D magnification, same figures as 3.83b]); BI-RADS 4. Spot view was not helpful in this case; the irregular density (lesion I) has almost disappeared (Fig. 3.85a), the morphology of microcalcifications is better assessed on 3D compared with spot view (Fig. 3.85b).
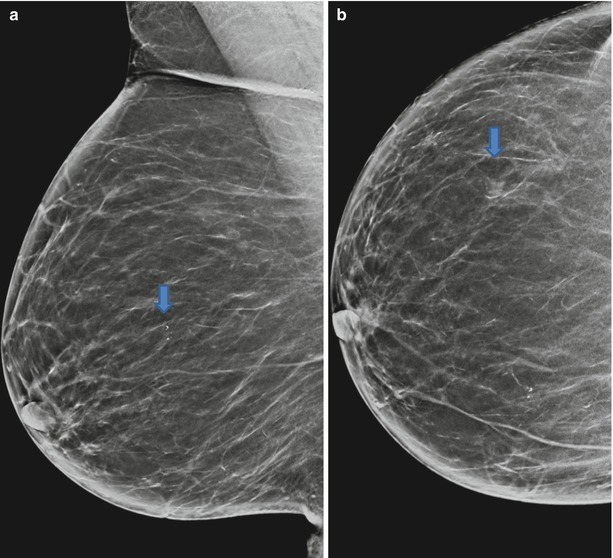
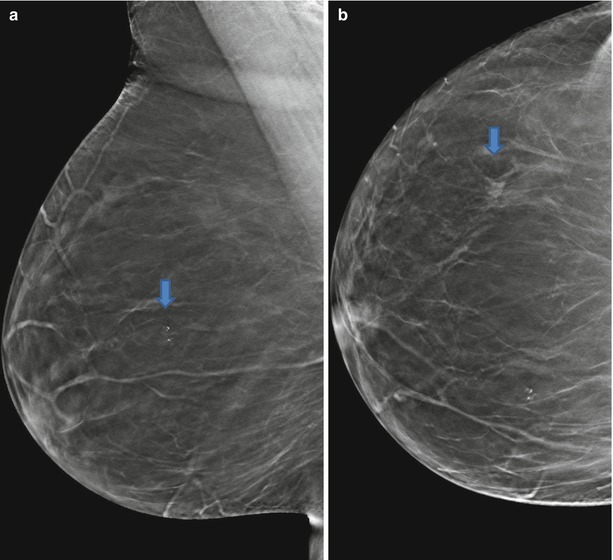
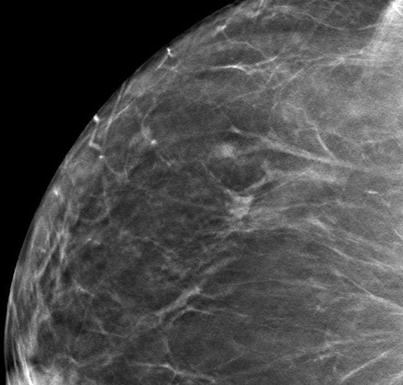
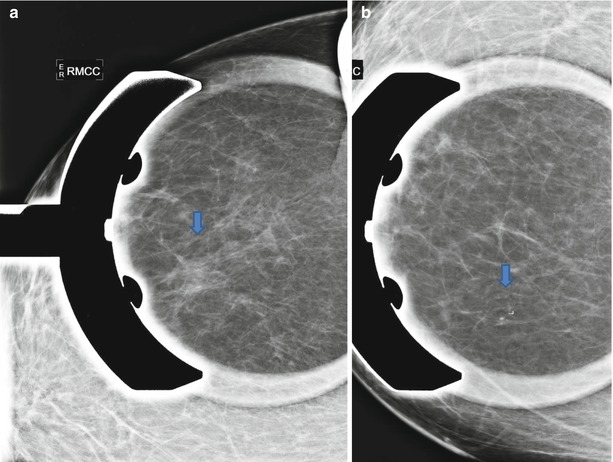
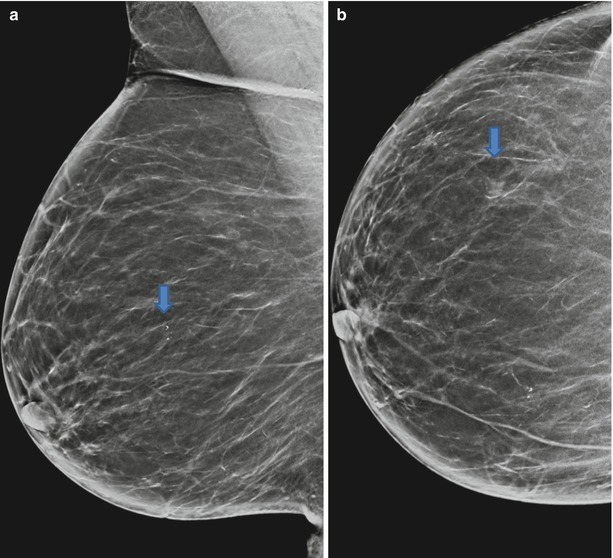
Fig. 3.82
(a, b) 2D (synthetic) (a) obl and (b) cc
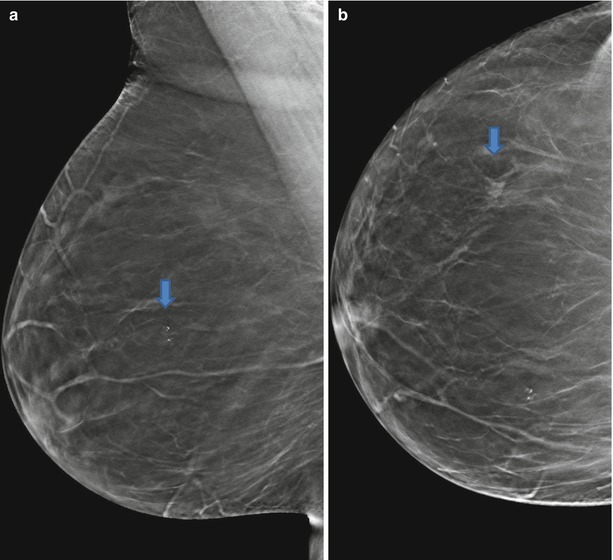
Fig. 3.83
(a, b) 3D (a) obl and (b) cc
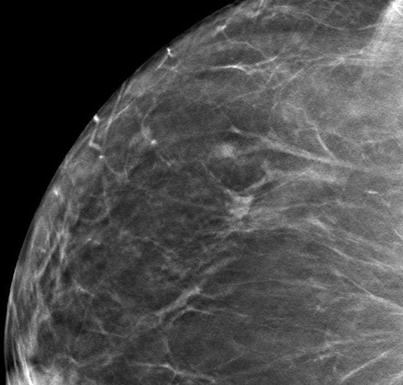
Fig. 3.84
3D magnification cc
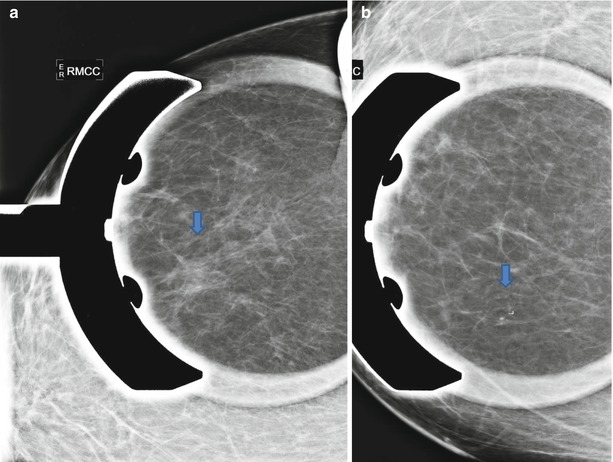
Fig. 3.85




(a, b) Spot views (a) and (b)
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree