Imaging manifestations of hematological diseases and their potential complications are broad, and there may be significant overlap in features of various disease processes. Knowledge of appropriate choice of imaging test, pertinent imaging patterns, and pathophysiology of disease can help the reader increase specificity in the diagnosis and treatment of the patient. Most importantly, we encourage readers of this review to engage their radiologists during the diagnostic, treatment, and management phases of care delivery.
Key points
- •
Imaging manifestations of hematological diseases and their potential complications are broad, and there may be significant overlap in features of various disease processes.
- •
Knowledge of appropriate choice of imaging test, pertinent imaging patterns, and pathophysiology of disease can help the reader increase specificity in the diagnosis and treatment of the patient.
- •
Most importantly, we encourage readers of this review to engage their radiologists during the diagnostic, treatment, and management phases of care delivery.
Introduction
The imaging of spinal manifestations of hematological disorders are best understood and appreciated by taking an anatomic compartment approach. In this review, we discuss such manifestations by focusing on the imaging appearance in the vertebral body/epidural, dural/leptomeningeal (meningeal), and spinal cord compartments. This review focuses on radiographic imaging, computed tomography (CT), and MRI, and will predominantly discuss vertebral and epidural disease. Where appropriate, details about meningeal and spinal cord involvement are included.
Introduction
The imaging of spinal manifestations of hematological disorders are best understood and appreciated by taking an anatomic compartment approach. In this review, we discuss such manifestations by focusing on the imaging appearance in the vertebral body/epidural, dural/leptomeningeal (meningeal), and spinal cord compartments. This review focuses on radiographic imaging, computed tomography (CT), and MRI, and will predominantly discuss vertebral and epidural disease. Where appropriate, details about meningeal and spinal cord involvement are included.
General imaging features
Vertebral/Epidural Disease
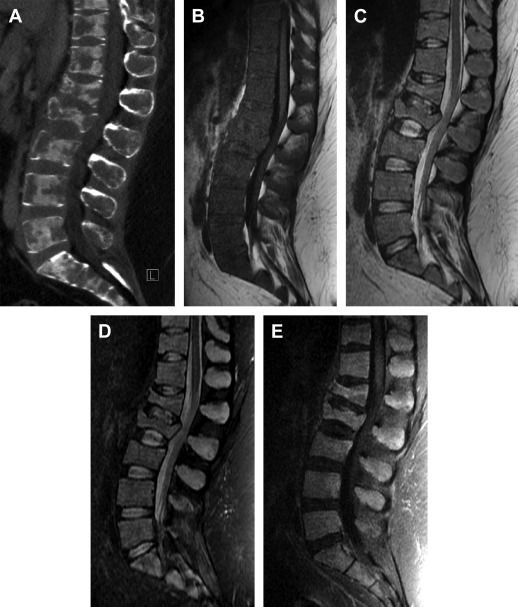
Compared with spinal metastatic disease, hematopoietic malignancies are more likely to be diffuse and less likely to have cortical destruction. As such, MRI is often superior to radiography and CT, particularly in visualizing bony lesions that are largely in bone marrow. It is worthwhile discussing a few imaging basics, particularly regarding MRI sequences as they apply to vertebral marrow disease.
T1 spin-echo weighted imaging (T1WI) is essential in bone marrow evaluation. Due to the size and tumbling frequency of fat molecules, yellow marrow normally has a hyperintense (bright) appearance on T1WI due to a short T1 relaxation time. In contradistinction, tumor and most other pathologic processes will have prolonged T1 relaxation times producing hypointense (low) signal that typically stands out sharply against the hyperintense background of fatty marrow.
Younger patients have more red hematopoietic marrow than yellow marrow, making visualization of lesions on T1WI more challenging. Fat suppression should not be used for noncontrast T1WI of the marrow, as this will remove the intrinsic contrast. The opposite is true when performing postcontrast T1WI; if fat suppression is not used, enhancing hyperintense lesions will lose their conspicuity against T1 hyperintense marrow. Therefore, fat suppression is essential for postcontrast T1WI when evaluating vertebral disease.
By the same token, routine T2 spin-echo weighted imaging (T2WI) is not ideal for vertebral and epidural evaluation. Pathologic processes are generally hyperintense on T2WI, and can be masked against background T2 signal of normal marrow. For this reason, fat suppression is also essential for T2WI in vertebral and epidural evaluation of the spine. Short tau inversion recovery (STIR) sequences are often used for this purpose, and provide relatively homogeneous fat saturation. Abnormalities on STIR often appear brighter than on routine T2WI, in part due to the change in dynamic range of the image. For this review, however, we use STIR and fat-saturated T2WI interchangeably.
Noncontrast T1WI, fat-suppressed T2WI (or STIR), and postcontrast fat-suppressed T1WI sequences are the bread and butter of vertebral marrow imaging. There are several additional advanced sequences that are touched on later, which can be useful adjuncts, including diffusion-weighted imaging (DWI), chemical shift imaging (CSI), and dynamic contrast-enhanced (DCE)-MRI techniques.
Detection and characterization of an epidural mass is critical in the imaging evaluation of the spine. MRI is generally preferable to CT for this assessment. As an epidural lesion grows larger, it first narrows the thecal sac and effaces the cerebrospinal fluid (CSF) around the cord, then eventually progresses to compress the cord itself, potentially causing cord edema and eventually myelomalacia. At the lumbosacral levels, epidural masses can compress the cauda equina. Epidural extension of vertebral tumor commonly has a bilobed appearance in the anterior epidural space, which has been called the “curtain sign,” due to limitation by the posterior longitudinal ligament and attached midline septum.
Posterior epidural masses are seen more commonly in hematologic malignancy compared with metastatic disease. Epidural masses can extend through intervertebral foramina and into the paraspinal regions. Contrast is useful not only in delineating extent of epidural tumor, but also in distinguishing tumor from disc herniation, which may mimic epidural tumor on noncontrast imaging but should not enhance with contrast.
Meningeal and Spinal Cord Disease
MRI is the standard for imaging meningeal and cord manifestations of hematological malignancy and any complications. Fat-saturated T2WI and postcontrast fat-saturated T1WI sequences are essential to evaluate the meninges, thecal sac CSF, spinal cord, and cauda equina. Precontrast T1WI is not vital by itself, but is useful when comparing with postcontrast T1WI if fat saturation was not used. Conventional T2WI (without fat saturation) can complement fat-saturated or STIR images.
Noncontrast CT or CT with intravenous contrast has minimal use in evaluating meningeal and cord disease. CT myelography can be useful in patients having contraindications to MRI. In this technique, iodinated contrast is injected in the thecal sac, usually via lumbar injection. The contrast fills the thecal sac and surrounds the cord and cauda equina, thereby producing an “outline” of these structures and any significant abnormality in their contour. Although CT myelography has some utility in differentiating intramedullary from intradural/extramedullary findings, further characterization of enhancement pattern, intramedullary characteristics, and extradural (outside the dura mater) is extremely limited to not possible.
Hematologic malignancies
Leukemia
Leukemia is the most common malignancy in children, as well as the ninth most common in adults. Acute lymphoblastic leukemia (ALL) and acute myeloid leukemia (AML) subtypes arise from immature leukocytes. Of childhood leukemia cases, approximately 80% are due to ALL and 10% are of the AML subtype. Chronic lymphocytic leukemia and chronic myeloid leukemia (CML) arise from mature cell lines.
Leukemia tends to infiltrate rather than focally replace the bone marrow. A caveat to this is that myeloid leukemias can have focal chloromas, also referred to as granulocytic sarcomas. These occur in 2.5% to 9.1% of patients with AML, and 5 times less commonly in patients with CML, with most younger than 15 years of age. Chloroma may occur before the onset of leukemia and can rarely be multifocal.
Computed tomography and radiography
Vertebral/epidural disease
Leukemic infiltration can appear as a permeative or mottled bone marrow appearance, which may be diffuse or regional. Lucent bands (“leukemic lines”), periosteal reactions, and subperiosteal erosions may be seen, although less commonly than in the appendicular skeleton. After treatment, lucent lines generally resolve quickly, whereas other CT and plain film findings may lag or persist.
Focal abnormality may not be evident on plain film or CT, and in many cases only diffuse osteopenia or a normal appearance is seen. Sclerotic foci are rare, and more likely to be encountered after treatment. Vertebral compression fractures are commonly seen ( Fig. 1 ). Vertebra plana, complete collapse of a vertebral body, is also occasionally encountered. Chloromas present as focal lytic lesions, with any extraosseous soft tissue components well depicted on CT.
Meningeal/spinal cord disease
CT is very poor for evaluation of meningeal and spinal cord disease. MRI is the study of choice and is discussed as follows.
MRI
Vertebral/epidural disease
On T1WI sequences, leukemic infiltration of bone marrow often manifests as diffuse homogeneous or speckled T1 hypointensity, and can sometimes be more regional. There is corresponding hyperintensity on STIR sequences, which can vary in intensity and conspicuity. Leukemic lesions enhance on postcontrast T1WI, albeit with high variability.
Approximately 10% of cases will have a normal MRI appearance. In pediatric patients in whom there is a greater fraction of hematopoietic cells, the normal marrow signal may be intermediate to low signal on T1WI. In these cases, detection of leukemic infiltrate can be challenging. Various quantitative MR techniques have been described for improving detection, including bulk T1 relaxation measurement and MR spectroscopy. CSI also has been used, demonstrating a lower fat fraction within tumor infiltrated marrow. Moore and colleagues demonstrated increased T1 relaxation times in those with active disease. These techniques have been used not only to improve detection, but also to evaluate response to therapy. Early work with DCE-MRI suggests it also may be useful in assessment of disease burden.
Chloromas appear as focal T1WI isointense and STIR hyperintense mass lesions. Enhancement is typically homogeneous, although necrotic foci have been reported. Chloromas can be predominantly epidural in location, sometimes without significant bony involvement. Epidural lesions may extend into neural foramina and the paravertebral region, may have multilevel involvement, and are at high risk for cord compression.
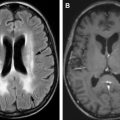
Meningeal/spinal cord disease
Although not as common, leukemic involvement of meninges can occur (neoplastic meningitis). The typical pattern on MRI is nodular or diffuse enhancement of the leptomeninges and cauda equina and/or diffuse enhancement of the CSF on fat-saturated postcontrast T1WI. Although this finding is not specific for leukemia, it is highly concerning if the patient has a history of the disease. Moreover, a normal MRI does not exclude neoplastic meningitis because MRI is less than 50% sensitive and specific. Therefore, CSF sampling is still highly specific (>95%) for neoplastic meningitis, but not as sensitive (∼50%). Last, leukemia rarely infiltrates the cord; however, a case report described intramedullary involvement by leukemia presenting as transverse myelopathy.
Polycythemia Vera
Vertebral/epidural disease
Polycythemia vera (PV) is a proliferative disorder of stem cells. The process is panhyperplastic, but typically causes pronounced erythrocytosis. PV typically demonstrates T1WI hypointense and STIR hyperintense signal abnormality diffusely involving the marrow. Some cases can have focal involvement. It is considered a low-grade malignant process, and 15% undergo transformation to AML. The imaging appearance is somewhat nonspecific among hematologic disorders, and cannot distinguish which cases have undergone myeloid metaplasia. Many cases eventually progress to myelofibrosis.
Lymphoma
Primary vertebral lymphoma is rare; however, lymphoma metastases to the spine are relatively common, found in 40% of patients with lymphoma in one autopsy series. Bony involvement usually occurs during the course of disease and is uncommon at presentation. Vertebral and epidural involvement is typically seen in advanced disseminated disease. Non-Hodgkin lymphoma (NHL) is 3 times as common as Hodgkin disease, and, accordingly, spinal involvement is more frequently encountered in NHL. In Hodgkin disease, vertebral involvement can occur with extranodal stage IV disease. Bony involvement can occur from local or hematogenous spread, and is typically only seen in late-stage widespread disease. When bony involvement does occur, it is commonly spinal.
Computed tomography and radiography
Vertebral/epidural disease
Commonly, a permeative, or “moth-eaten” pattern is seen. Focal lesions may be lytic, sclerotic, or mixed. Sclerotic lesions are somewhat more common in Hodgkin disease. An “ivory vertebra” appearance can be seen on radiographs or CT, a name given to diffuse, relatively homogeneous sclerosis of a vertebral body. A lamellated pattern of periosteal reaction can be seen, more commonly with HD. NHL can rarely have an appearance overlapping with that of multiple myeloma, with multiple focal lytic lesions.
Meningeal/spinal cord disease
CT is very poor for evaluation of meningeal and spinal cord disease. MRI is the study of choice and is discussed as follows.
MRI
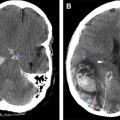
Vertebral/epidural disease
Lymphoma lesions demonstrate focal hypointense signal on T1WI. Lymphoma is more likely to focally replace rather than infiltrate the marrow, as opposed to leukemia. It is often not possible to distinguish the lesions from metastatic disease based solely on MRI features. The lesions enhance on postcontrast T1WI ( Fig. 2 ). The lesions may demonstrate isointense to mildly hypointense T2WI signal as well as restricted water diffusion on DWI, reflecting hypercellularity.
When involvement is relatively diffuse, there can be overlap in the appearance of neoplastic and non-neoplastic marrow processes. Some initial work with DCE imaging has demonstrated increased perfusion parameters in cases of diffuse tumor, with a potential to differentiate these from benign disorders.
The “wrap-around sign” of vertebral lymphoma describes the appearance of diffuse vertebral involvement, circumferential paravertebral involvement, and preserved depiction of the intervening vertebral cortex. This sign is useful in differentiating patients with lymphoma, from those with other metastatic disease and multiple myeloma.
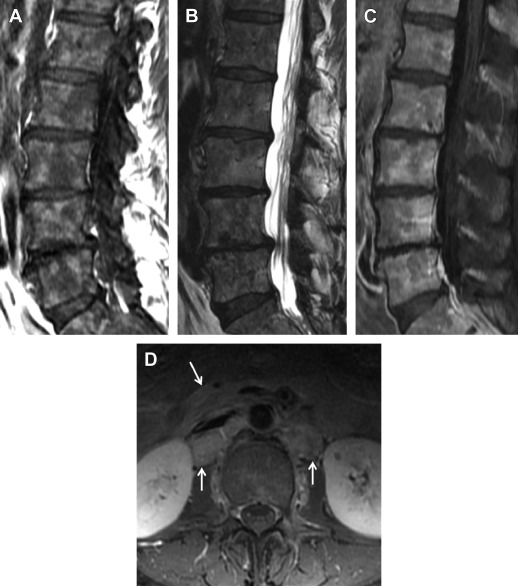
As with other vertebral tumors, epidural extension can occur with the potential for spinal canal compromise (see Fig. 2 ). Uncommonly, lymphoma may be predominantly epidural without significant vertebral involvement. This may occur by spread from lymph nodes through the intervertebral foramina, and can be seen with both Hodgkin disease and NHL.
Meningeal/spinal cord disease
Like leukemia, meningeal involvement of lymphoma can be leptomeningeal ( Fig. 3 ). However, dural infiltration can occur both diffusely or focally (masslike). As lymphoma is a great mimicker, its appearance can be heterogeneous and may raise concern for other diseases, such as tuberculosis, sarcoidosis, or metastases from other malignancy. Of note, epidural extramedullary hematopoiesis can be difficult to differentiate from lymphoma, regardless of compartment.

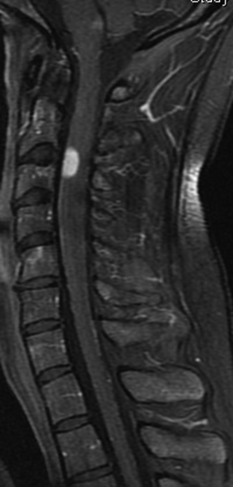
Although rare, intramedullary lymphoma deposits can occur; however, carry a differential diagnosis if a primary diagnosis of lymphoma is not known ( Fig. 4 ). This differential diagnosis includes dermoid tumor, astrocytoma, ependymoma, hemangioblastoma, ganglioneuroblastoma, and metastases.
Waldenstrom Macroglobulinemia
Waldenstrom macroglobulinemia (WM) is a type of NHL characterized by infiltration of bone marrow with lymphoplasmacytic cells. It is also considered a plasma cell dyscrasia, with monoclonal immunoglobulin M-protein found in serum. Patients also may have lymphadenopathy, organomegaly, and hyperviscosity syndrome among other systemic manifestations. WM is usually an indolent process typically presenting in older patients. Transformation to high-grade lymphoma can occur.
Vertebral/epidural disease
On radiography and CT, studies may appear normal or demonstrate generalized osteopenia. Focal lytic lesions are not typically seen, a differentiating factor from myeloma. MRI often demonstrates diffuse homogeneous or variegated marrow signal abnormality, with hypointensity on precontrast T1WI, hyperintensity on STIR, and enhancement on fat-saturated postcontrast T1WI, which may be patchy. On both CT and MRI, lymphadenopathy may be visualized in the included surrounding soft tissues, such as the retroperitoneum ( Fig. 5 ).
Meningeal/spinal cord disease
Leptomeningeal infiltration of WM is exceedingly rare; however, when it occurs is called Bing-Neel syndrome. MRI can show leptomeningeal and/or pachymeningeal enhancement on postcontrast T1WI. Contrast administration is essential for proper imaging and if findings are present in the setting of known WM, Bing-Neel syndrome should be considered.
Multiple Myeloma
Multiple myeloma is the most common primary malignancy of bone, and accounts for approximately 10% of hematologic malignancies. Myeloma results from abnormal monoclonal proliferation of plasma cells. It is one of the plasma cell dyscrasias, along with monoclonal gammopathy of unknown site, plasmacytoma, WM, and primary amyloidosis, among others. Myeloma can occur anywhere but does have a predilection for vertebral involvement. Abnormal plasma cells infiltrate the bone marrow in a variety of focal and diffuse patterns.
The International Staging System uses serum Beta 2 microglobulin and albumin to grade disease from I to III. Myeloma also can be characterized from low grade to high grade, according to the percentage of marrow infiltration seen histologically. Durie and Salmon is another commonly used staging scheme, which initially used both plain radiography and clinical/laboratory findings to stage disease from 1 to 3. This system has been adapted to include MRI and FDG-PET findings, both of which are more sensitive for focal lesion detection, termed the Durie-Salmon Plus staging system.
Meningeal and spinal cord involvement by multiple myeloma is rare and presents only in the most advanced disseminated cases of this disease. No specific imaging pattern is noted. The following discussion pertains to vertebral/epidural disease.
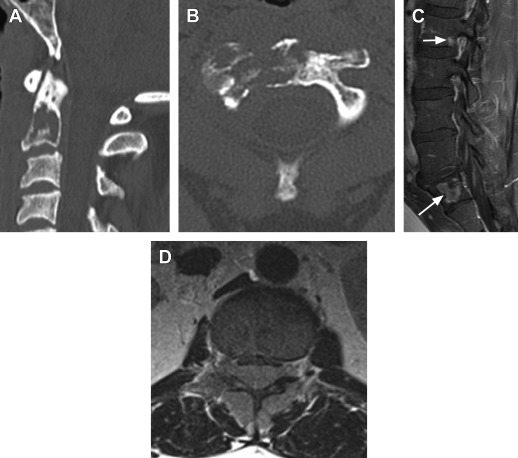
Computed tomography and radiography
Findings vary from diffuse abnormalities, such as generalized osteopenia or a permeative appearance, to discrete focal lesions. Permeative involvement can be geographic or more diffuse. Focal lesions are generally purely lytic. The abnormal plasma cells strongly stimulate osteoclastic activity; for this reason, bone scintigraphy is of little use in myeloma. The classic appearance is that of a well-circumscribed, ellipsoid, often-subcortical lucency, referred to as a “punched-out” lesion ( Fig. 6 ). Untreated lytic lesions will not have a corticated margin. CT can detect lesions when plain radiographs are normal. Even CT, however, may appear normal, particularly with low-grade disease. Multiple compression fractures may be seen, which when coupled with an osteopenic appearance of myeloma, variably mimic benign osteoporotic fractures.

Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree