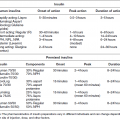
Chapter 9 Evanthia Lalla, DDS, MS; Dana Wolf, DMD, MS; and Ira B. Lamster, DDS, MMSc Diabetes mellitus is estimated to affect 371 million people worldwide [1]. Approximately half of these individuals remain undiagnosed and a very large number of individuals are at-risk. In the United States, approximately 8.3% of the total population has diabetes and about a quarter of those affected are undiagnosed [2]. Type 2 diabetes is a preventable disease, and so are its complications, yet in most countries primary prevention is minimal. Early diagnosis is a particular problem for type 2 diabetes, in which there is a long asymptomatic period [3] and where diagnosis usually occurs when patients present to healthcare providers with signs, symptoms, or even complications of the disease [4]. Early identification of affected individuals may lead to earlier intervention and a subsequent decrease in the significant morbidity and mortality associated with diabetes. In this chapter, we will first briefly review a number of the screening recommendations that exist in the medical community and then review in more detail screening models that have incorporated oral findings to identify individuals with diabetes mellitus. We will also discuss the potential for a more active role by dentists in diabetes screening and the barriers that exist to implementation of a more active role. In 2003, the World Health Organization and the International Diabetes Federation held a meeting on the topic of screening for type 2 diabetes. The aims of the meeting were to review the evidence for the usefulness of screening for early detection of type 2 diabetes and to make recommendations relevant to health care policy, action, and future research. At that time, the organizations found no direct evidence that earlier detection of type 2 diabetes has an impact on health outcomes. They did, however, find direct evidence that the incidence of diabetes can be reduced in high-risk individuals who may be identified via diabetes screening. Additionally, they acknowledged that screening may help raise disease awareness. The meeting report addressed a number of issues surrounding screening such as cost-effectiveness, sensitivity, and specificity of the screening test; the psychological and social effects of testing; and the ability of the health care system to intervene if the disease is identified. Rather than put forward specific screening recommendations, the report urged health authorities and professional organizations to formulate their own screening protocols for type 2 diabetes. The American Diabetes Association (ADA) currently recommends screening to detect type 2 diabetes in asymptomatic individuals of any age who are overweight or obese and have one or more additional risk factors for diabetes (Table 9.1) [4]. The recommended test is either a hemoglobin A1c (HbA1c), a fasting plasma glucose (FPG), or a two-hour oral glucose tolerance test. In the absence of any risk factors for diabetes, the ADA recommends testing for diabetes starting at age 45 with repeat testing at three-year intervals if the results are normal. Because the incidence of type 2 diabetes has increased dramatically over the last ten years, especially in minority populations, the ADA also recommends testing overweight children and adolescents who have two or more additional risk factors for diabetes. They recommend that testing be initiated at age 10 or at onset of puberty, and repeated every three years if results are negative. Table 9.1 Risk factors for type 2 diabetes mellitus. The U.S. Preventive Service Task Force recommends screening for type 2 diabetes in asymptomatic adults with sustained blood pressure greater than 135/80 mm Hg [5]. This recommendation is based on the fact that in individuals with diabetes and hypertension, lowering blood pressure below conventional targets reduces the incidence of cardiovascular events and associated mortality. Dental care facilities represent, for a number of reasons, alternative health care settings to detect unrecognized diabetes in a large segment of the population. First, as reviewed in detail in Chapter 6, multiple studies have demonstrated that diabetes adversely affects periodontal status [6], and that these effects appear to operate early in life [7, 8], suggesting that periodontitis may be one of the earliest complications of diabetes. There are also other oral manifestations of diabetes [9] (reviewed in Chapter 8), and patients with undiagnosed disease may be seen in the dental office with diabetes-related oral signs or symptoms. Second, according to the Centers for Disease Control and Prevention, nearly 70% of American adults have seen a dental provider in the preceding year, and health-care utilization patterns indicate that individuals tend to seek routine and preventive dental care more frequently than routine and preventive medical care [10, 11]. Lastly, dental patients often return for multiple non-emergent and recall/maintenance visits during which dental professionals can assess risk factors, advise on healthy lifestyle, perform or order blood screening tests, refer to a physician for diagnostic testing and treatment, and follow up on outcomes. The concept of screening for diabetes in the dental office is not new [12–16], since the link between diabetes and periodontitis has been known for many decades. The first large-scale effort to systematically assess whether dental findings can contribute to the identification of people with undiagnosed diabetes was published in 2007 [17]. The study used National Health and Nutrition Examination Survey (NHANES) III data to develop a predictive equation that could determine the probability of undiagnosed diabetes using patient-reported information and periodontal clinical parameters routinely assessed in the dental office. The analyses performed revealed that individuals with family history of diabetes, self-reported hypertension and high cholesterol, and clinical evidence of periodontal disease bear a probability of 27–53% of having undiagnosed diabetes, with Mexican-American men exhibiting the highest probability and white women the lowest. These findings suggested that the dental office could provide an opportunity to identify individuals unaware of their diabetic status. Three subsequent reports [18–20], all using NHANES data, approached the same concept in different ways and confirmed the potential for a role of dental professionals in diabetes identification. The first report (reviewed in more detail in Chapter 7) showed that periodontal disease at baseline is an independent predictor of incident diabetes [18]. Although conflicting data are available [21] and this topic warrants further investigation, the result of this study supports the use of periodontal parameters in the identification of diabetes risk. The second of these studies aimed to compare the proportion of subjects who would be recommended for screening according to ADA guidelines between dental patients with and without periodontitis. Additionally, the authors assessed whether at-risk individuals with periodontitis had visited a dental professional recently, and thus would have had a screening opportunity [19]. The findings indicated that more than 60% of those without periodontitis and more than 90% of those with periodontitis met ADA guidelines for diabetes screening. Of those at-risk with periodontitis, 50% had seen a dentist in the past year and 60% in the past two years. The third study [20] suggested that dental care providers should consider using a clinical guideline that includes the following parameters as predictors: waist circumference, age, self-reported oral health, self-reported weight and race/ethnicity, as well as any additional information on periodontal status and family history of diabetes. Although, arguably, some of these parameters are not easy to determine in a dental care setting, the proposed algorithm had good performance characteristics, corroborating the notion that the dental visit provides an important potential venue for this type of screening. The first study that collected data de novo to assess the performance of targeted identification protocols for unrecognized prediabetes and diabetes in dental patients was published in 2011 [22]. Importantly, detection of prediabetes was part of the study design as well. Prediabetes often precedes type 2 diabetes and has emerged as a serious health concern because it independently places individuals at risk for serious micro- and macro-vascular complications [23]. In the study, 601 individuals who presented for care at a dental school clinic and had never been told they have prediabetes or diabetes were recruited. To target those at some level of risk for diabetes, the inclusion criteria encompassed being at least 40 years old if non-Hispanic white or at least 30 years old if Hispanic or non-white, and self-report of at least one diabetes risk factor (family history of diabetes, hypertension, high cholesterol, or overweight). This resulted in 535 subjects who then received a periodontal examination and a point-of-care fingerstick HbA1c test, which provided additional variables to be used in the prediction models. Subjects were asked to return following an eight-hour fast for a venipuncture FPG test, the result of which was used as the study outcome to signify potential diabetes or prediabetes, per ADA guidelines at the time. In total, out of 506 subjects who returned for the FPG test, 182 were identified with an abnormal result: 21 (4.2%) potentially diabetic (FPG at least 126 mg/dL), and 161 (31.8%) prediabetic (FPG = 100–125 mg/dl). Performance characteristics of simple models to identify dysglycemia (FPG at least 100 mg/dl) using variables that are readily available in any dental care setting were evaluated and optimal cut-offs for each variable in a given model were identified. A model including only two dental variables (number of missing teeth and percent of teeth with deep periodontal pockets) had an estimated area under the receiver operating characteristic curve (AUC) of 0.65. The addition of the point-of-care HbA1c test improved the AUC to 0.79 (p < 0.001). The presence of at least 26% teeth with deep pockets or at least four missing teeth correctly identified 73% of true cases; the addition of a point-of-care HbA1c of at least 5.7% increased correct identification to 92%. Because not all practitioners and/or patients will opt for a blood test in the dental setting, the finding that the use of just two dental variables provides high sensitivity is of significant merit. Indeed, both predictive models presented in this study have sensitivity similar to what has been reported for diabetes risk assessment approaches tested in medical settings [24], and because of their simplicity they have great potential for adoption. Interestingly, no diabetes prediction model has been universally accepted for use in medical settings, and it has been suggested that recalibration of algorithms might be necessary when models are applied to different populations [25]. A limitation of the study described above is that models were developed and assessed in a population that is predominantly Hispanic. Testing to assess external validity of these algorithms in diverse patient populations is needed. More recently, additional studies exploring the notion of screening for undiagnosed diabetes in dental settings have been published. First, the early concept of using gingival blood for screening [12, 14–16, 26] was revisited in a highly vulnerable population in India [27], where almost half of the subjects tested had elevated blood glucose levels, suggestive of diabetes. Unfortunately, this report failed to provide critical information about the dental/periodontal status of the population and the specifics and performance characteristics of the screening approach used making the findings hard to interpret.
Identification of dental patients with undiagnosed diabetes
Medical models for diabetes screening
Non-modifiable
Modifiable
Diabetes identification in dental care settings
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree