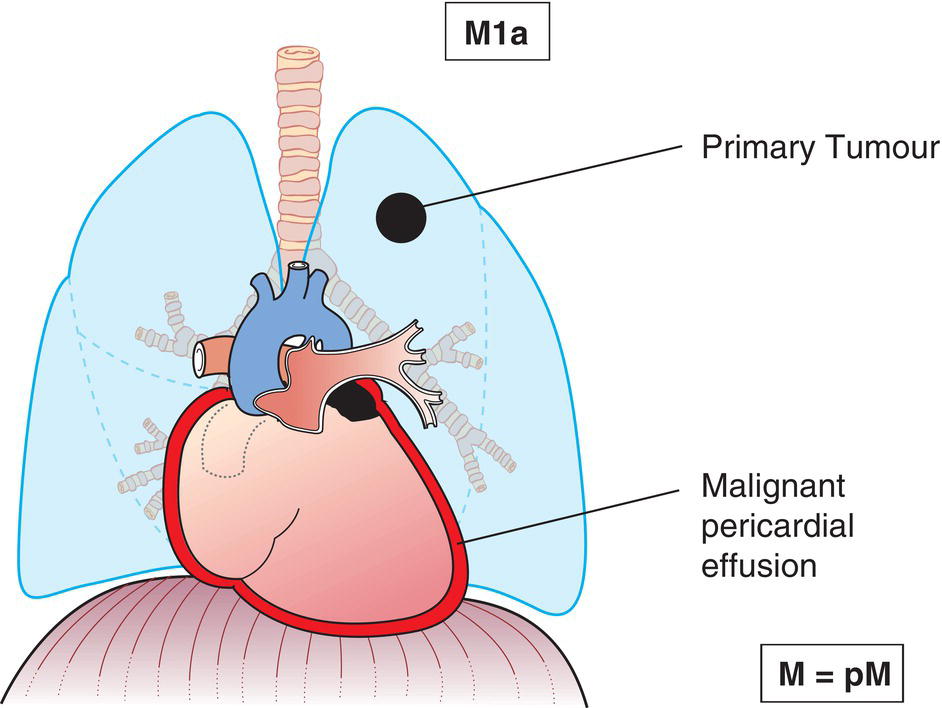
The classification applies to carcinomas of the lung, including non‐small cell carcinomas, small cell carcinomas and bronchopulmonary carcinoid tumours. It does not apply to sarcomas and other rare tumours. There should be histological confirmation of the disease and division of cases by histological type. The regional lymph nodes are the intrathoracic nodes (mediastinal, hilar, lobar, interlobar, segmental and subsegmental), scalene and supraclavicular lymph nodes. In tumour masses, grey colour means part‐solid/non‐invasive tumour; black colour means solid/invasive tumour. Notes 1 The uncommon superficial spreading tumour of any size with its invasive component limited to the bronchial wall, which may extend proximal to the main bronchus, is also classified as T1a. 2 T2 tumours with these features are classified T2a if 4 cm or less, or if size cannot be determined, and T2b if greater than 4 cm but not larger than 5 cm. 3 Most pleural (pericardial) effusions with lung cancer are due to tumour. In a few patients, however, multiple microscopical examinations of pleural (pericardial) fluid are negative for tumour, and the fluid is non‐bloody and is not an exudate. Where these elements and clinical judgement dictate that the effusion is not related to the tumour, the effusion should be excluded as a staging element. The pT and pN categories correspond to the T and N categories. Note pM0 and pMX are not valid categories.
LUNG (ICD‐O C34)
Rules for Classification
Anatomical Subsites
Regional Lymph Nodes
TNM Clinical Classification
T – Primary Tumour
TX
Primary tumour cannot be assessed, or tumour proven by the presence of malignant cells in sputum or bronchial washings, but not visualized by imaging or bronchoscopy
T0
No evidence of primary tumour
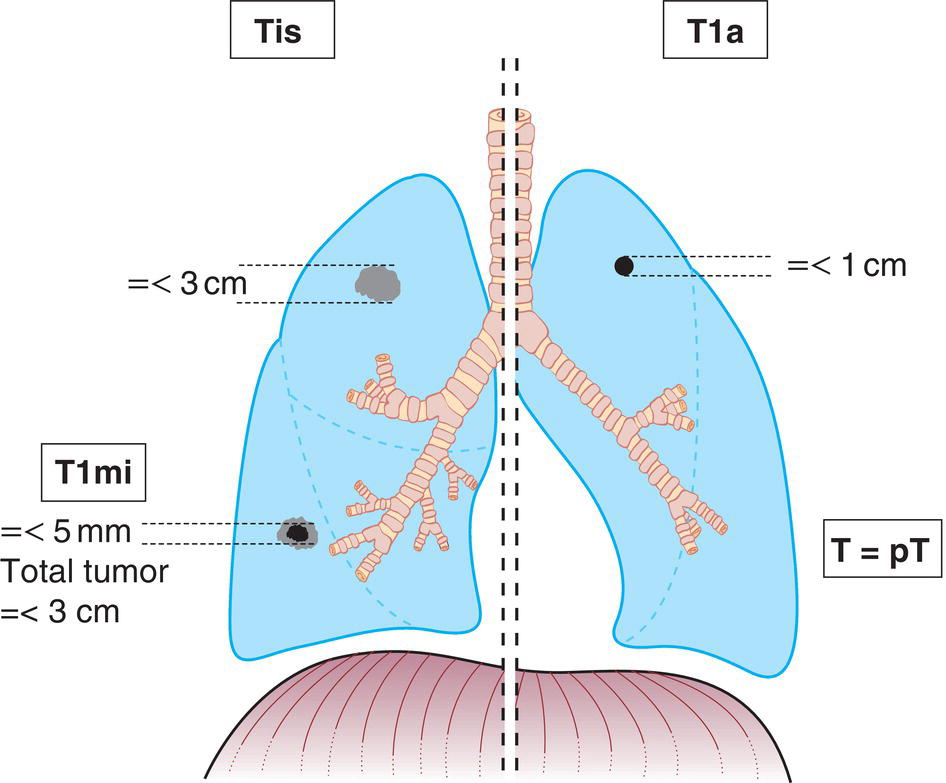
Tis (AIS)
Adenocarcinoma in situ (Fig. 266)
Tis (SCC)
Squamous cell carcinoma in situ
T1
Tumour 3 cm or less in greatest dimension, surrounded by lung or visceral pleura, without bronchoscopic evidence of invasion more proximal than the lobar bronchus (i.e., not in the main bronchus)1
T1mi
Minimally invasive adenocarcinoma (Fig. 266)
T1a
Tumour 1 cm or less in greatest dimension (Fig. 266)
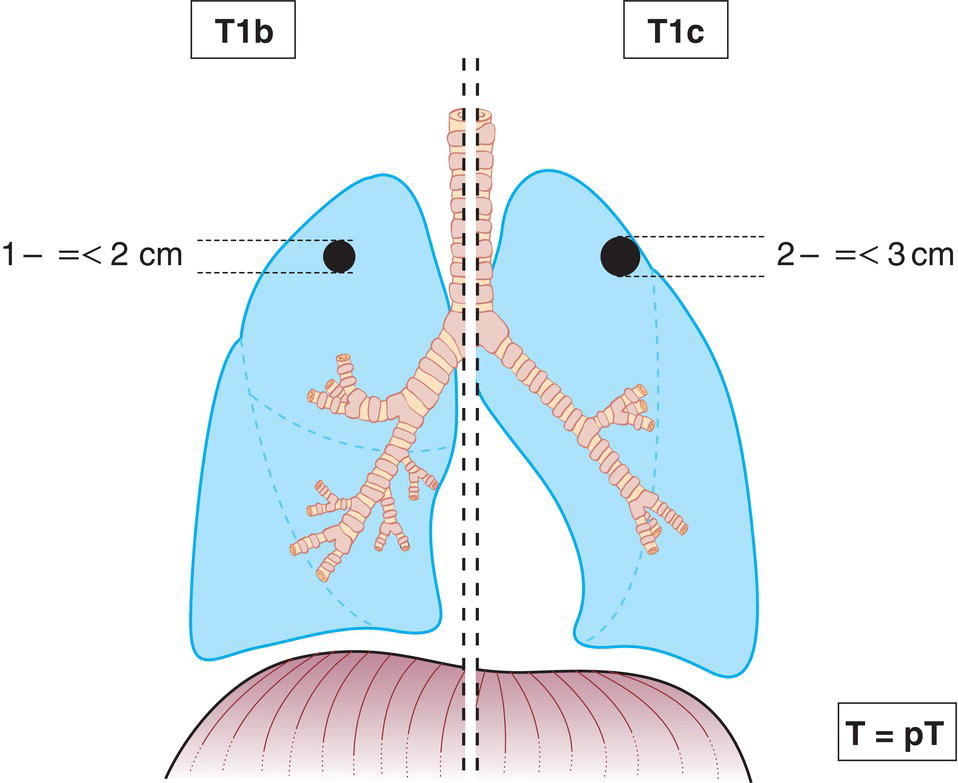
T1b
Tumour more than 1 cm but not more than 2 cm in greatest dimension (Fig. 267)
T1c
Tumour more than 2 cm but not more than 3 cm in greatest dimension (Fig. 267)
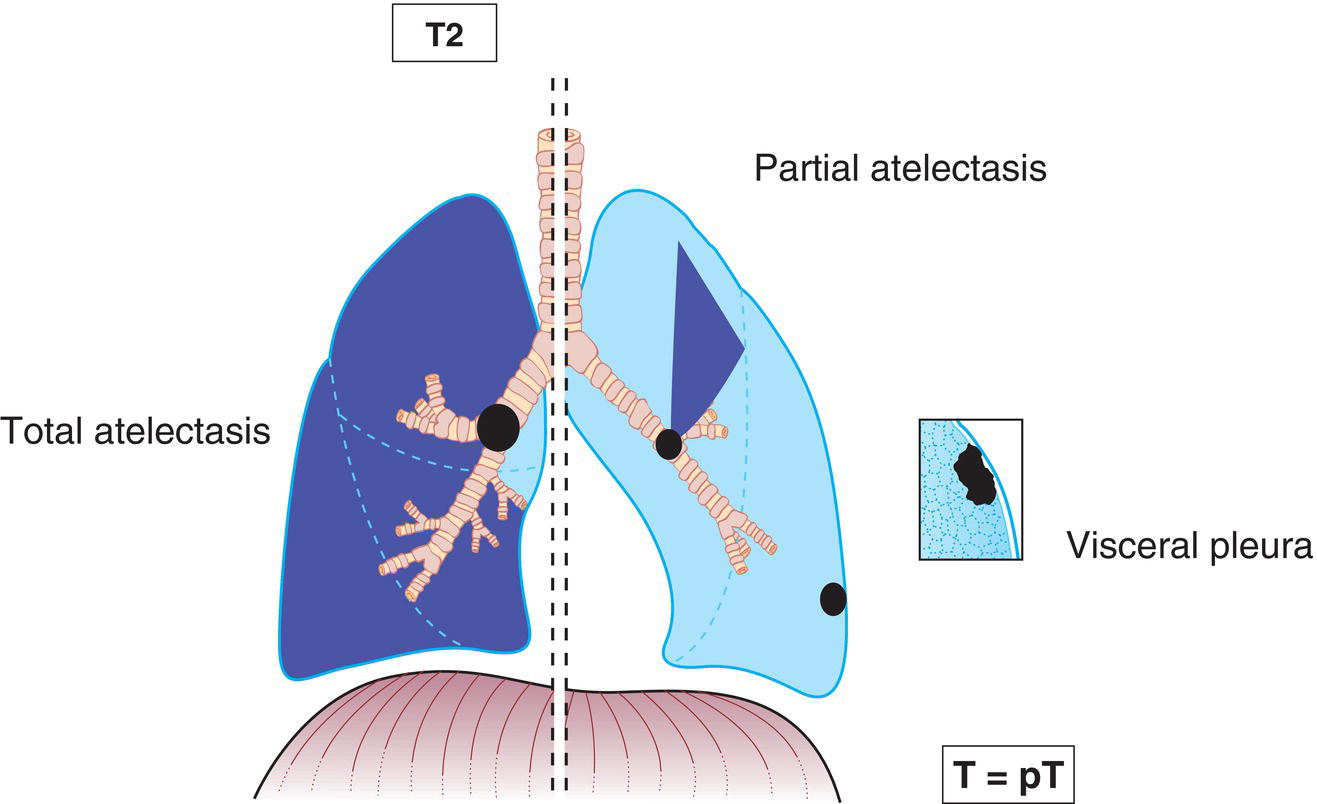
T2
Tumour more than 3 cm but not more than 5 cm; or tumour with any of the following features:2
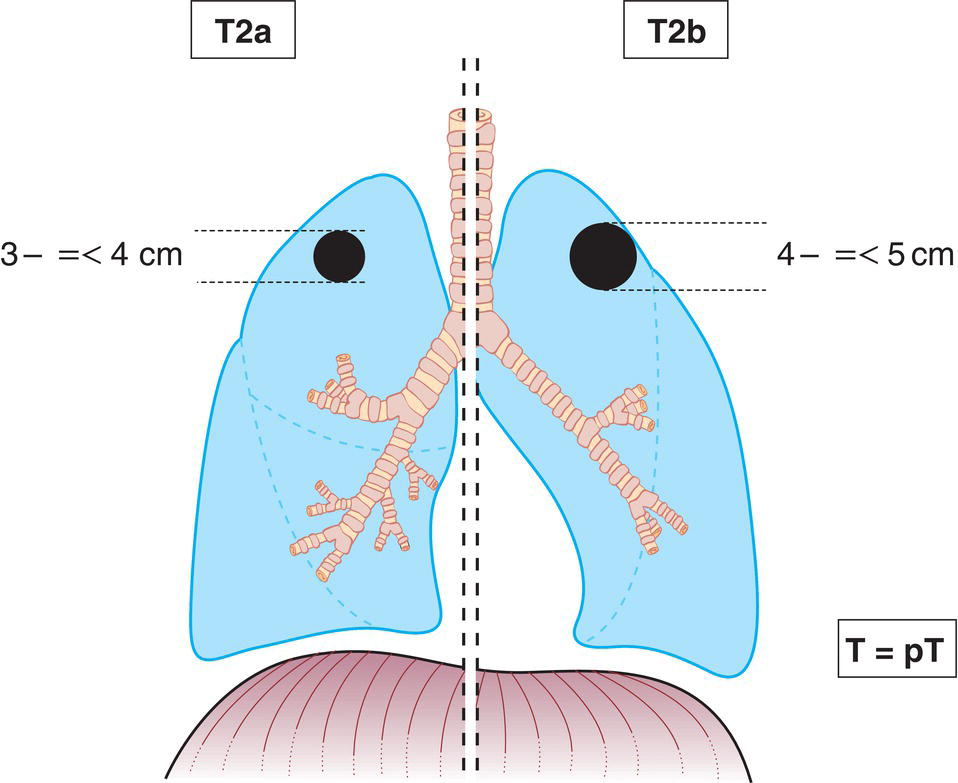
T2a
Tumour more than 3 cm but not more than 4 cm in greatest dimension (Fig. 269)
T2b
Tumour more than 4 cm but not more than 5 cm in greatest dimension (Fig. 269)
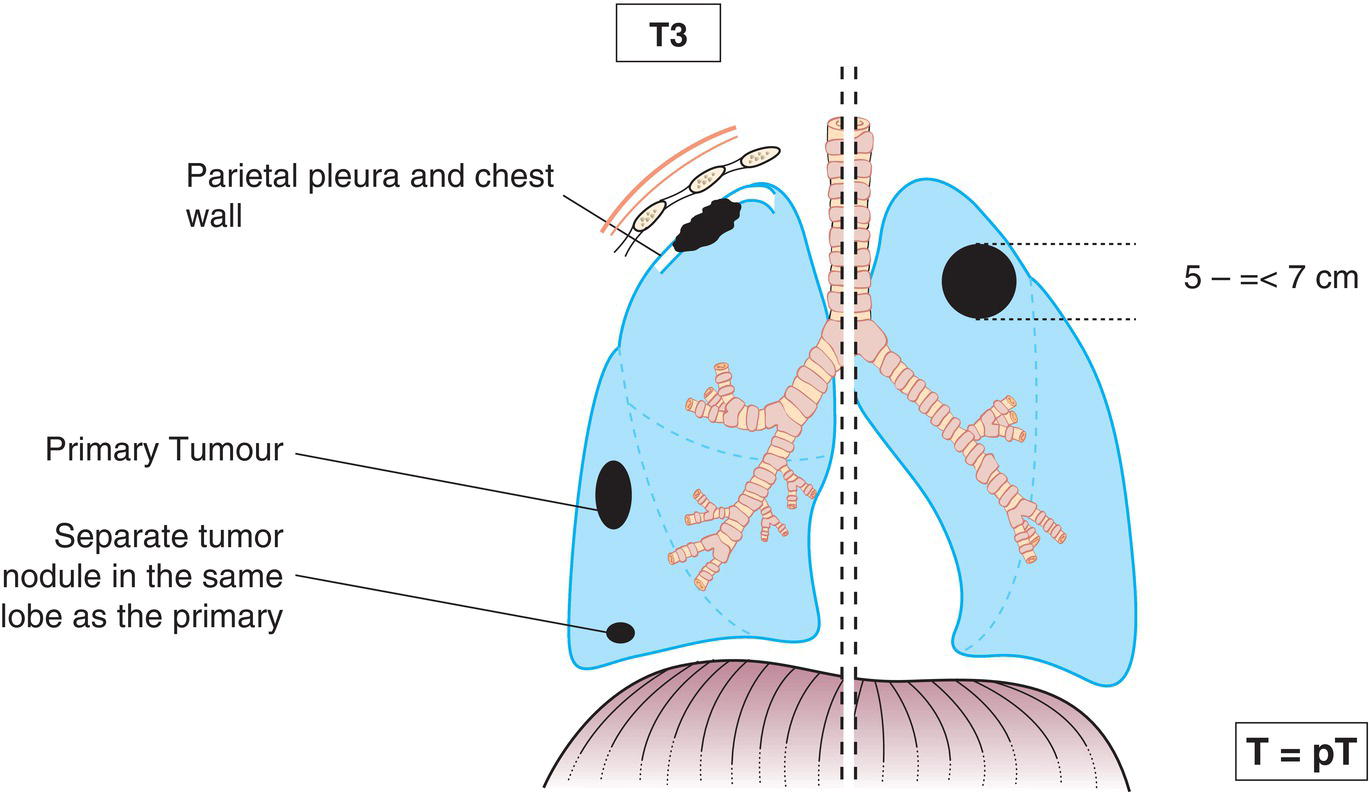
T3
Tumour more than 5 cm but not more than 7 cm in greatest dimension or one that directly invades any of the following: chest wall (including superior sulcus tumours), phrenic nerve, parietal pericardium; or associated separate tumour nodule(s) in the same lobe as the primary (Fig. 270)
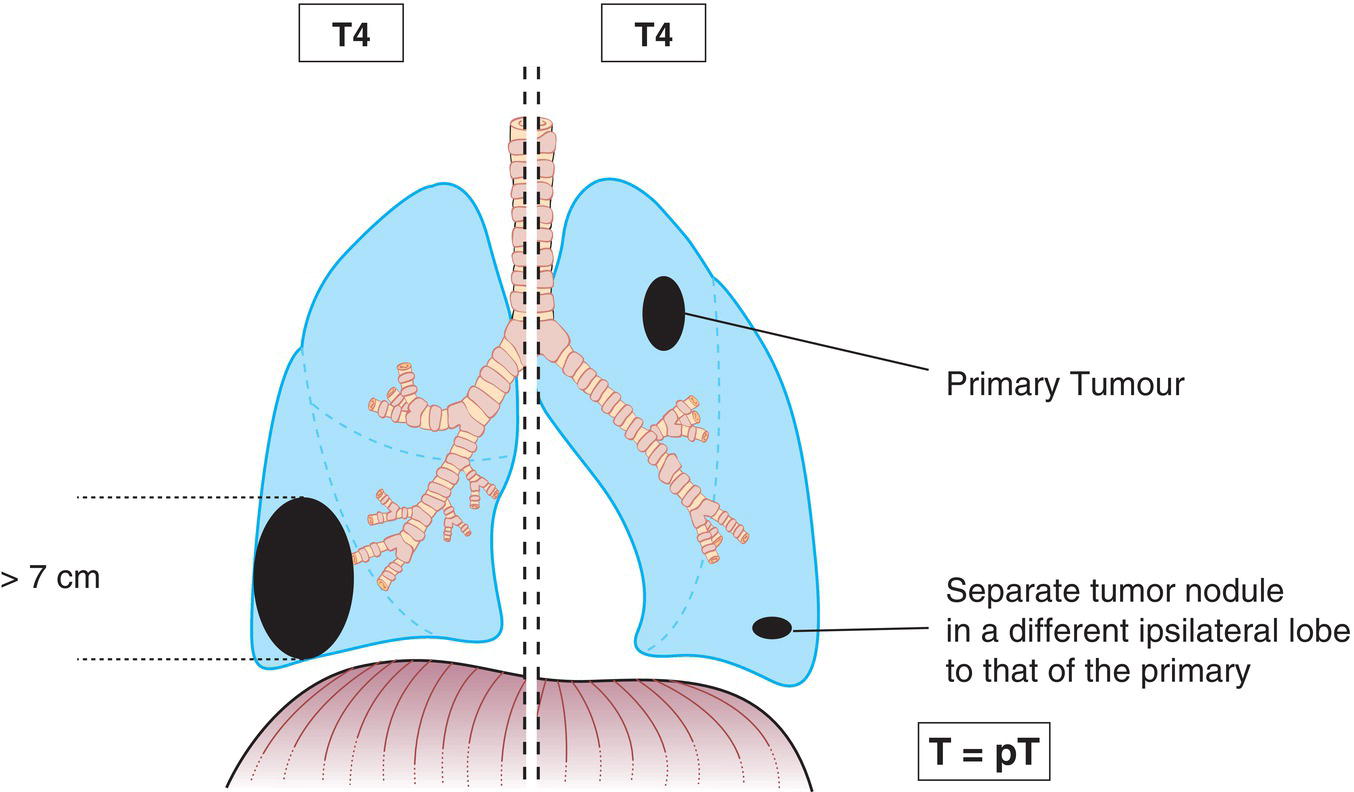
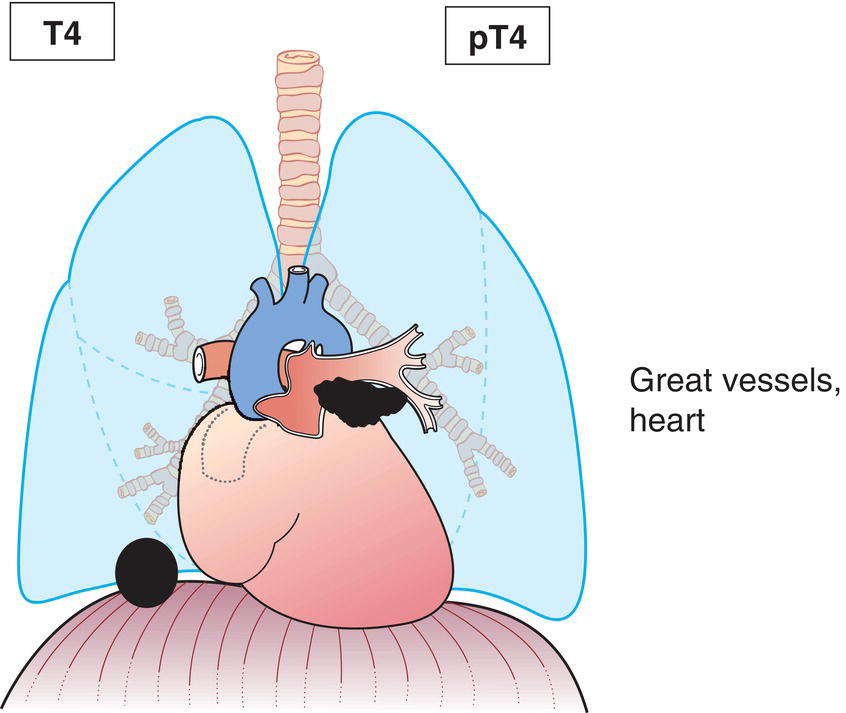
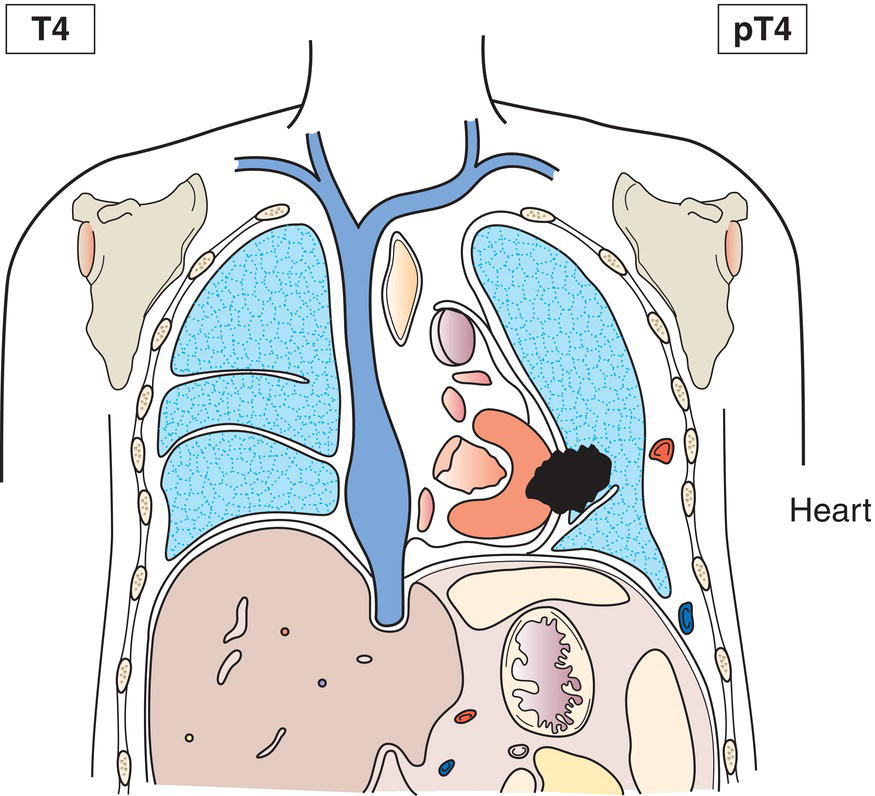
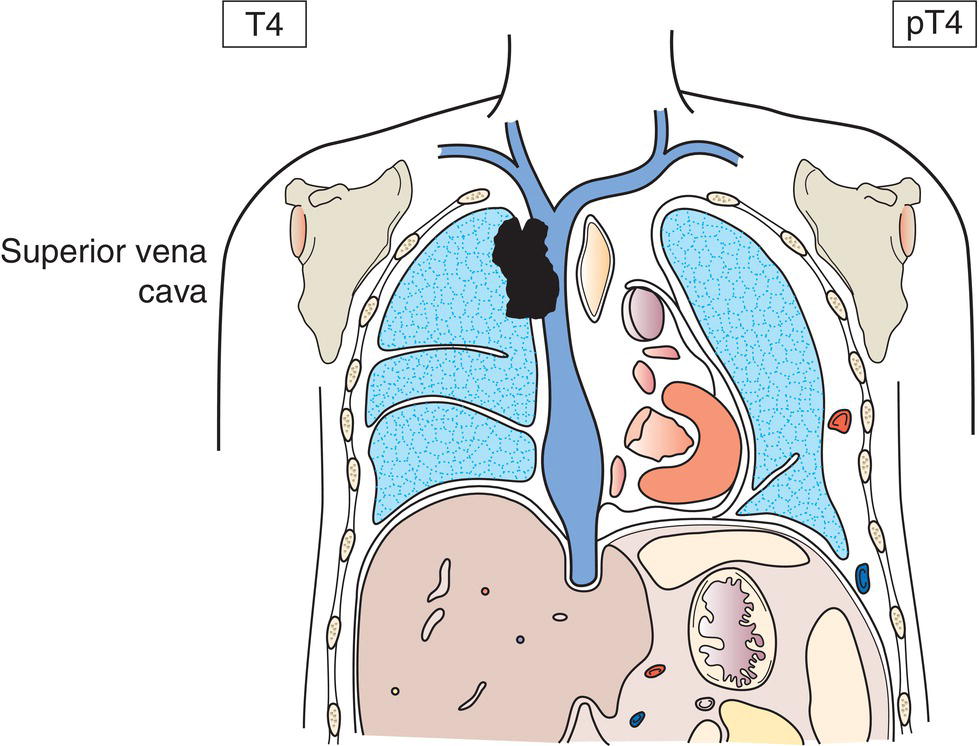
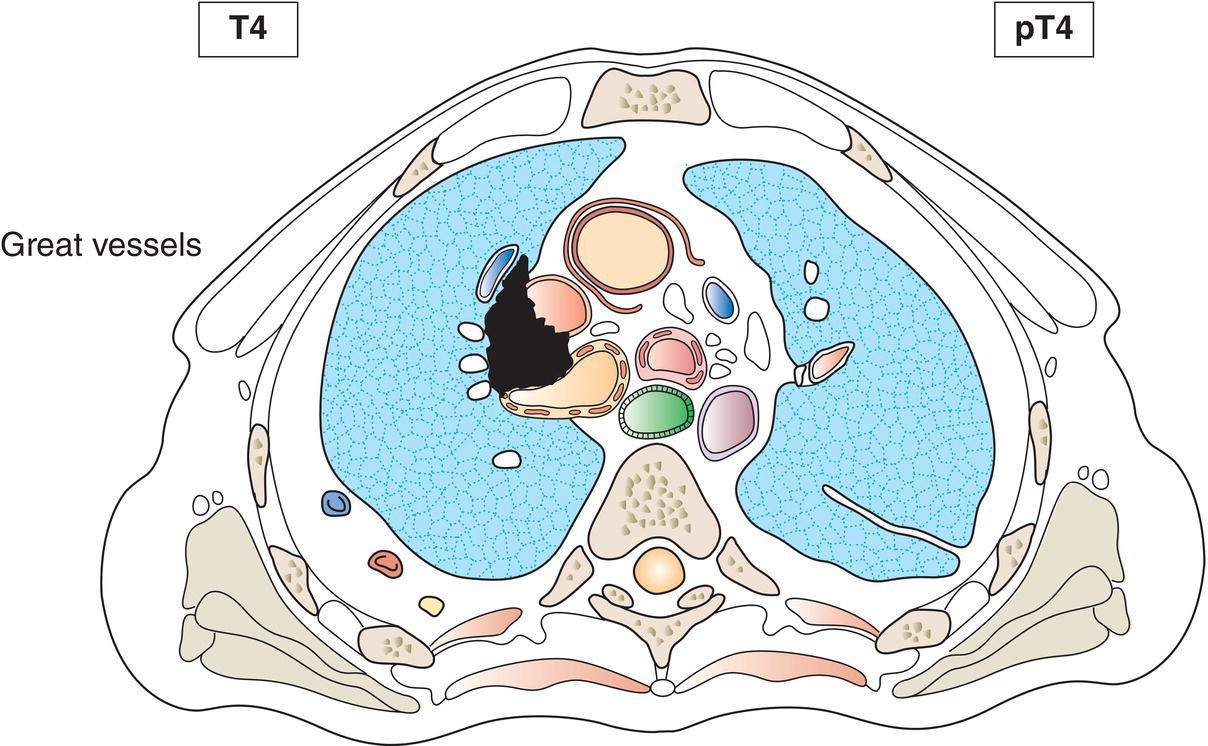
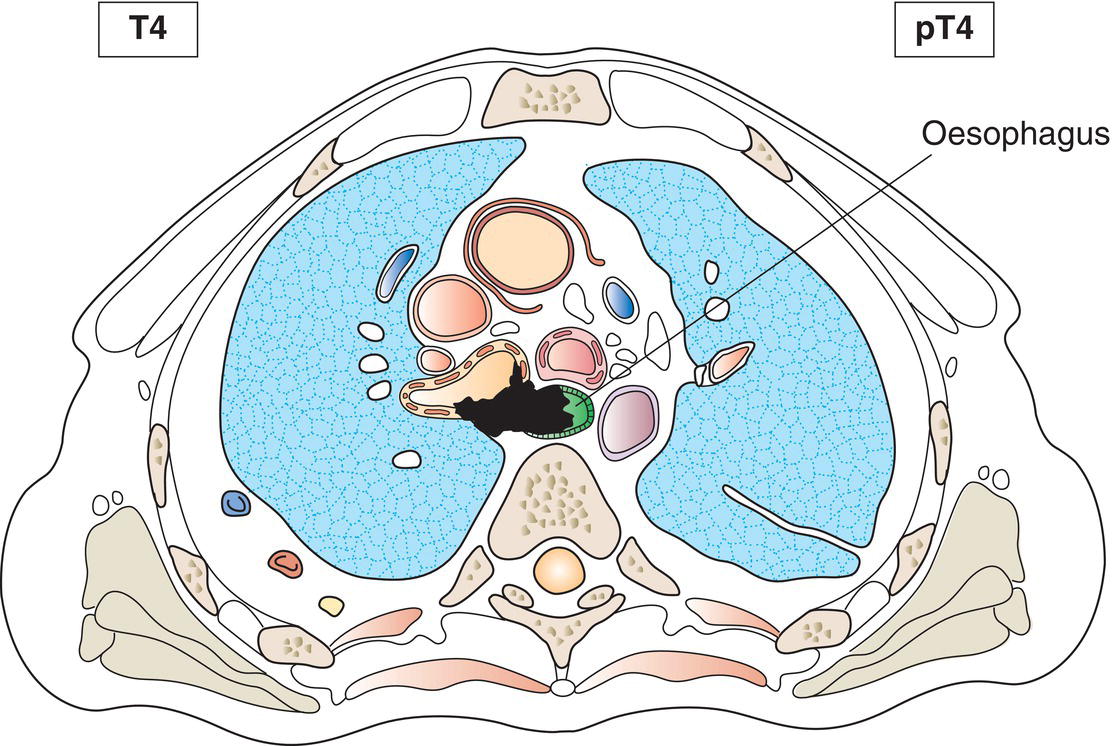
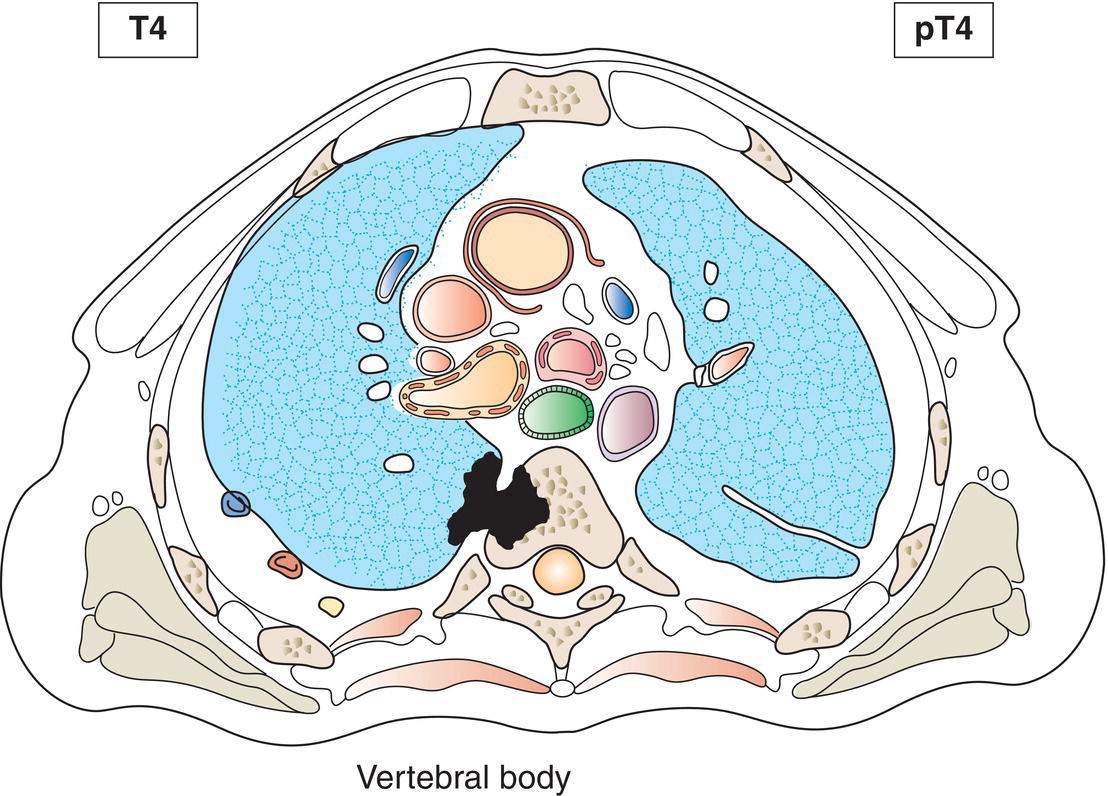
T4
Tumours more than 7 cm (Fig. 271) or one that invades any of the following: diaphragm (Fig. 272), mediastinum, heart (Figs. 272, 273), great vessels (Figs. 272, 274, 275), trachea, recurrent laryngeal nerve, oesophagus (Fig. 276), vertebral body (Fig. 277), carina; separate tumour nodule(s) in a different ipsilateral lobe to that of the primary (Fig. 271)
N – Regional Lymph Nodes
NX
Regional lymph nodes cannot be assessed
N0
No regional lymph node metastasis
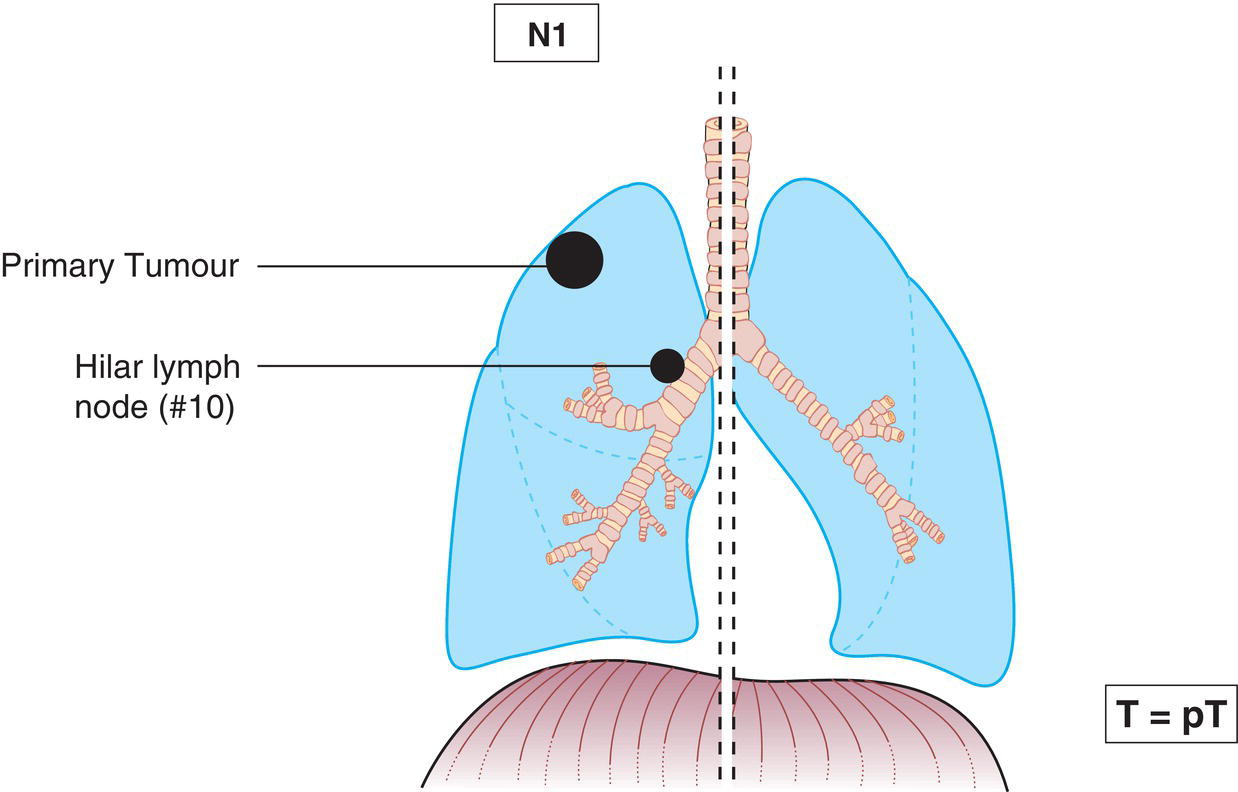
N1
Metastasis in ipsilateral peribronchial, ipsilateral interlobar and/or ipsilateral hilar lymph nodes and Intrapulmonary nodes, including involvement by direct extension (Figs. 278, 279)
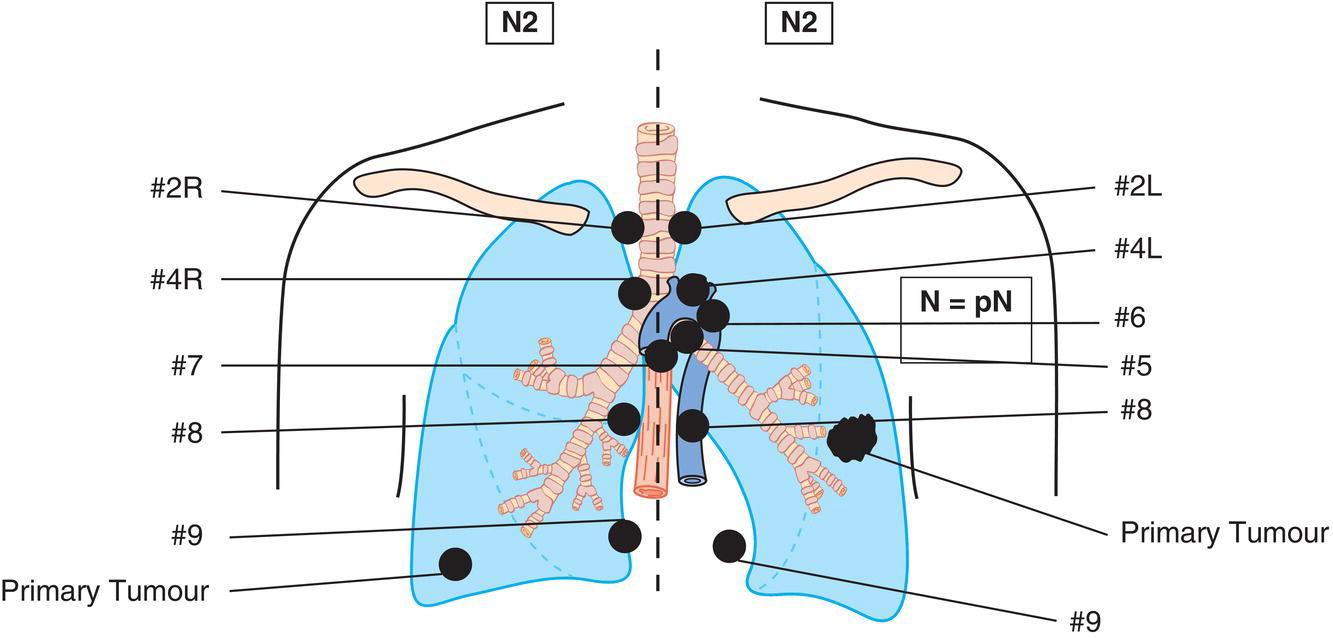
N2
Metastasis in ipsilateral mediastinal and/or subcarinal lymph node(s) (Fig. 280)
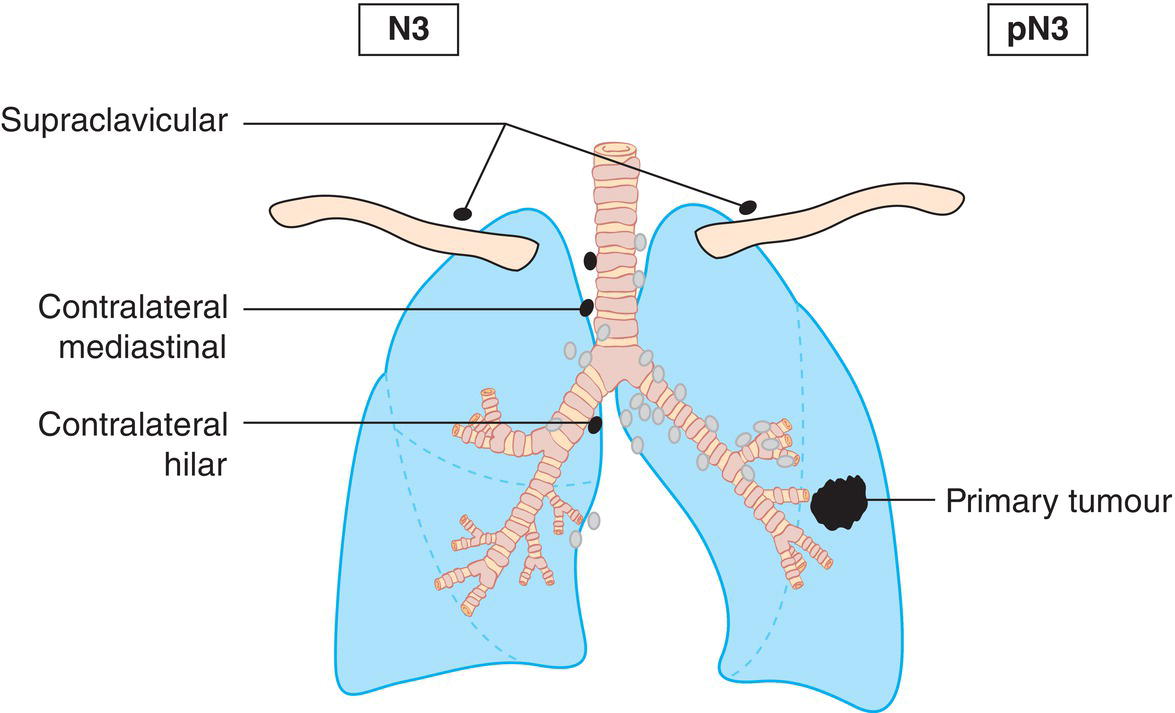
N3
Metastasis in contralateral mediastinal, contralateral hilar, ipsilateral or contralateral scalene, or supraclavicular lymph node(s) (Fig. 281) 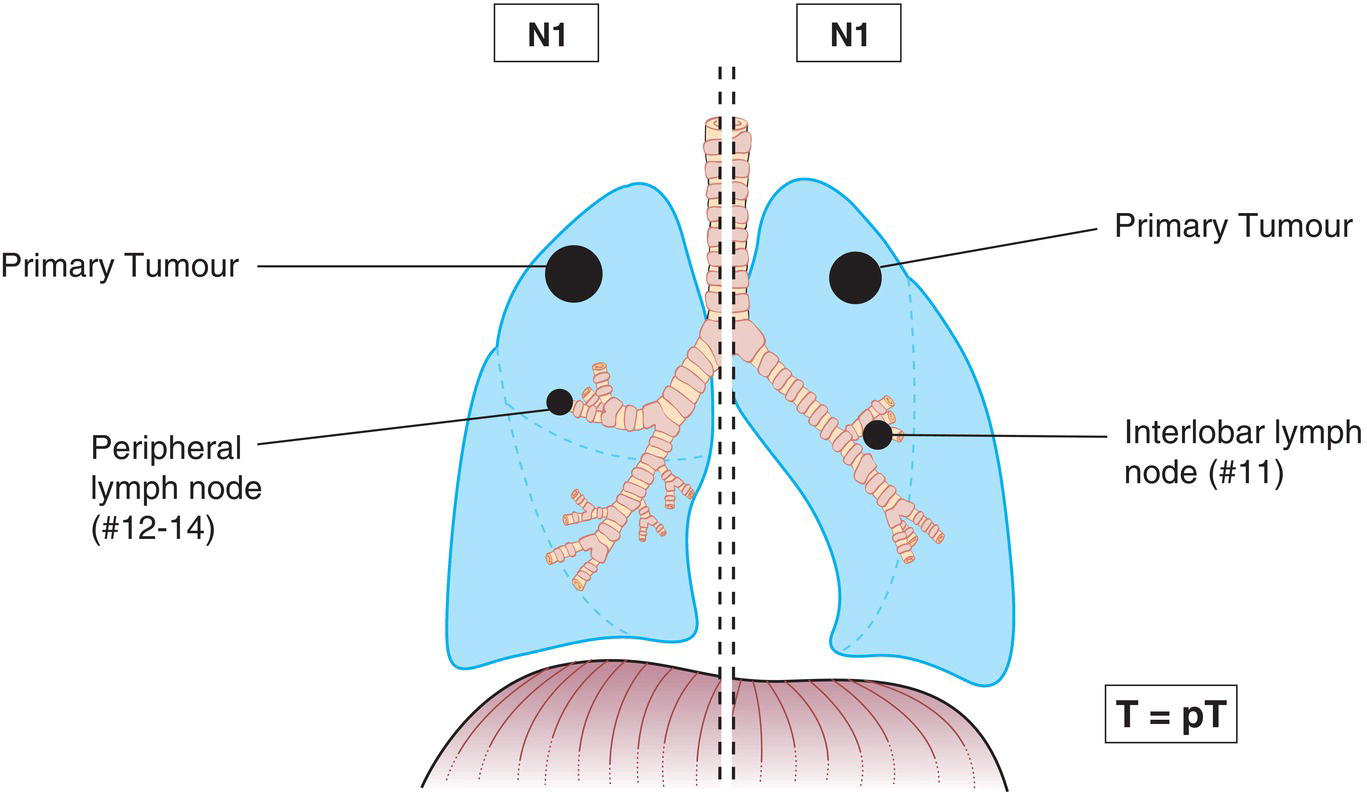
M – Distant Metastasis
M0
No distant metastasis
M1
Distant metastasis
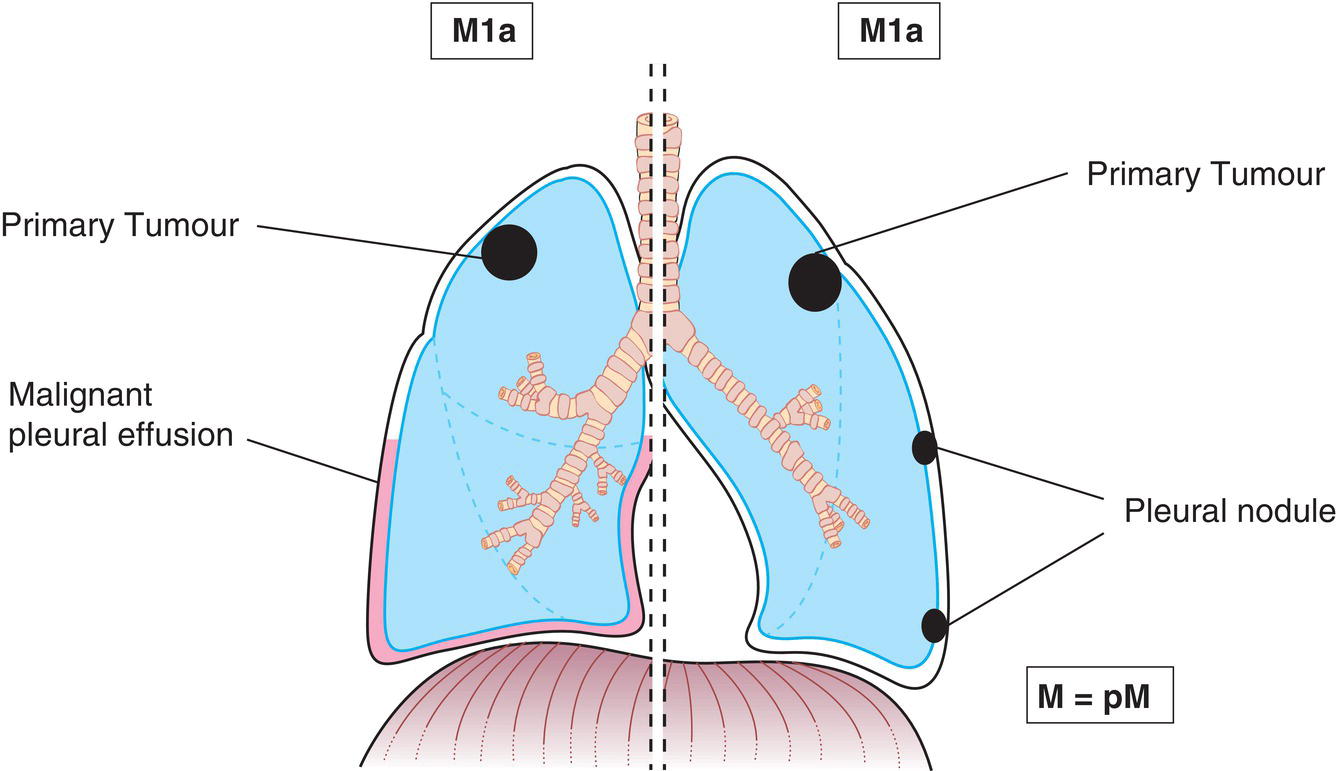
M1a
Separate tumour nodule(s) in a contralateral lobe (Fig. 282); tumour with pleural or pericardial nodules or malignant pleural (Fig. 283) or pericardial effusion (Fig. 284)3
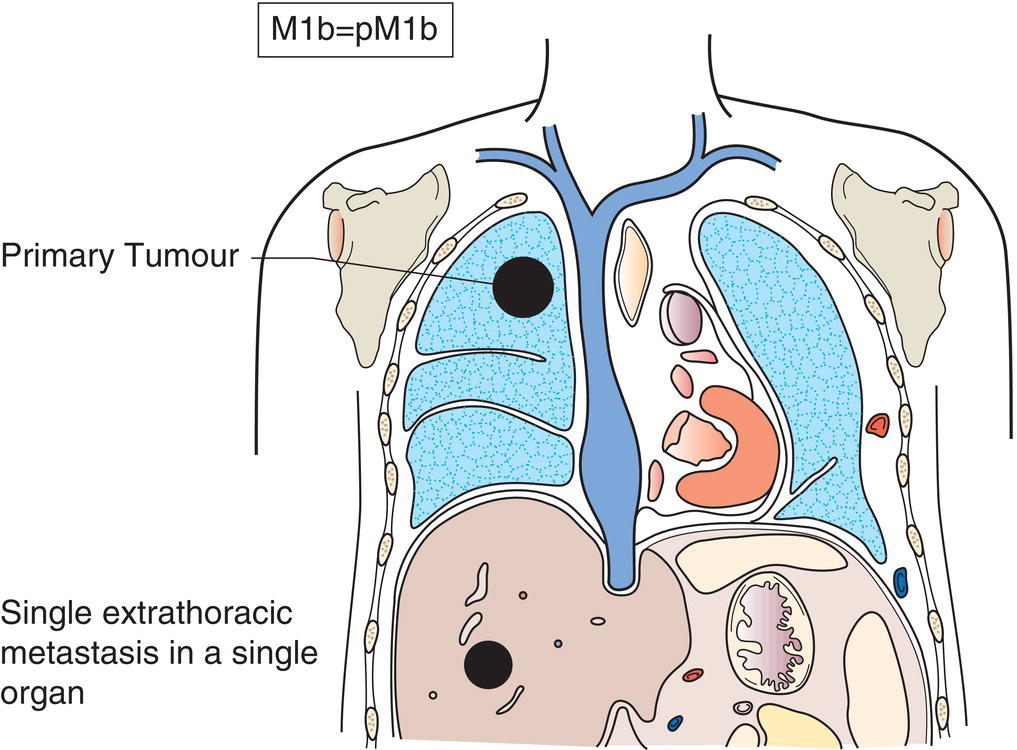
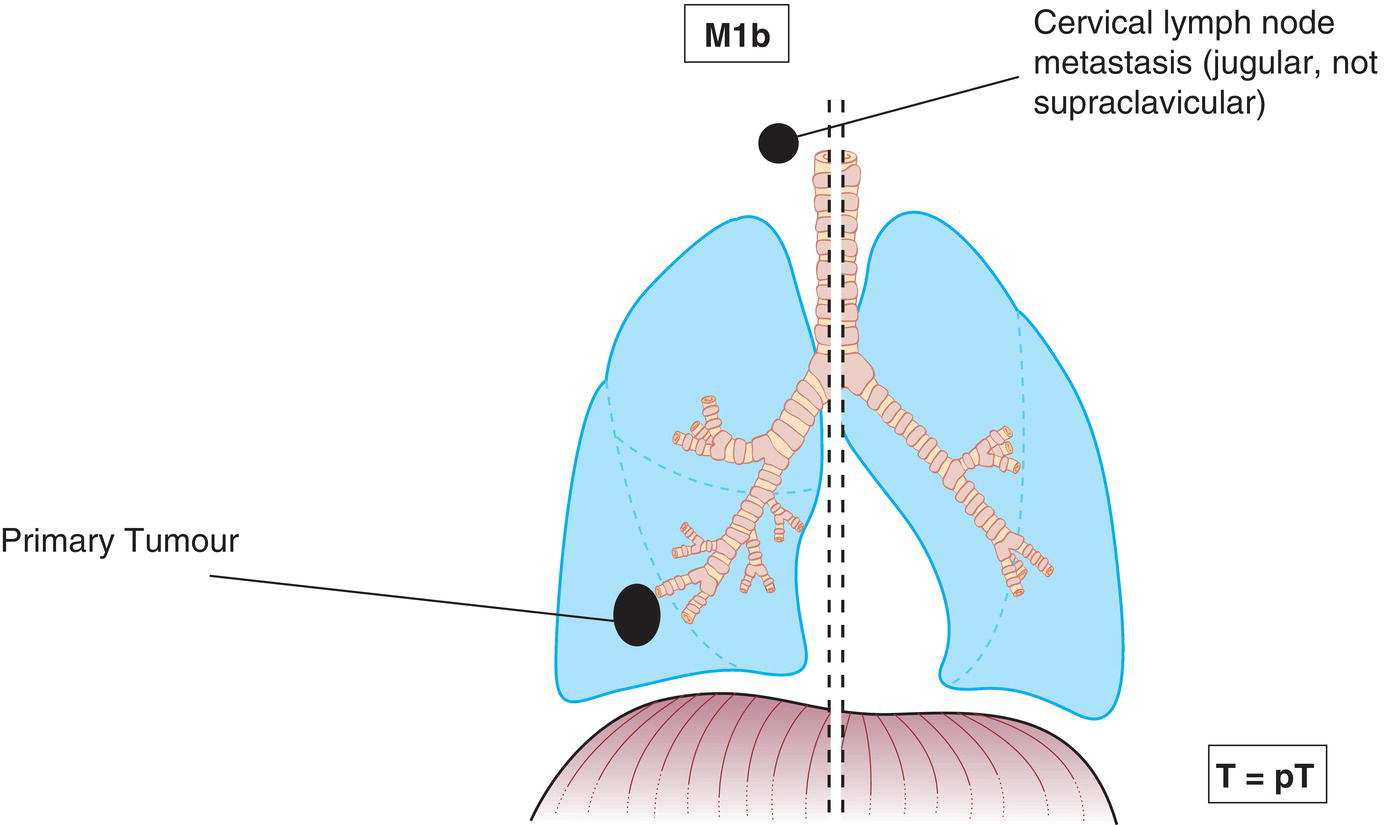
M1b
Single extrathoracic metastasis in a single organ (Figs. 285, 286)
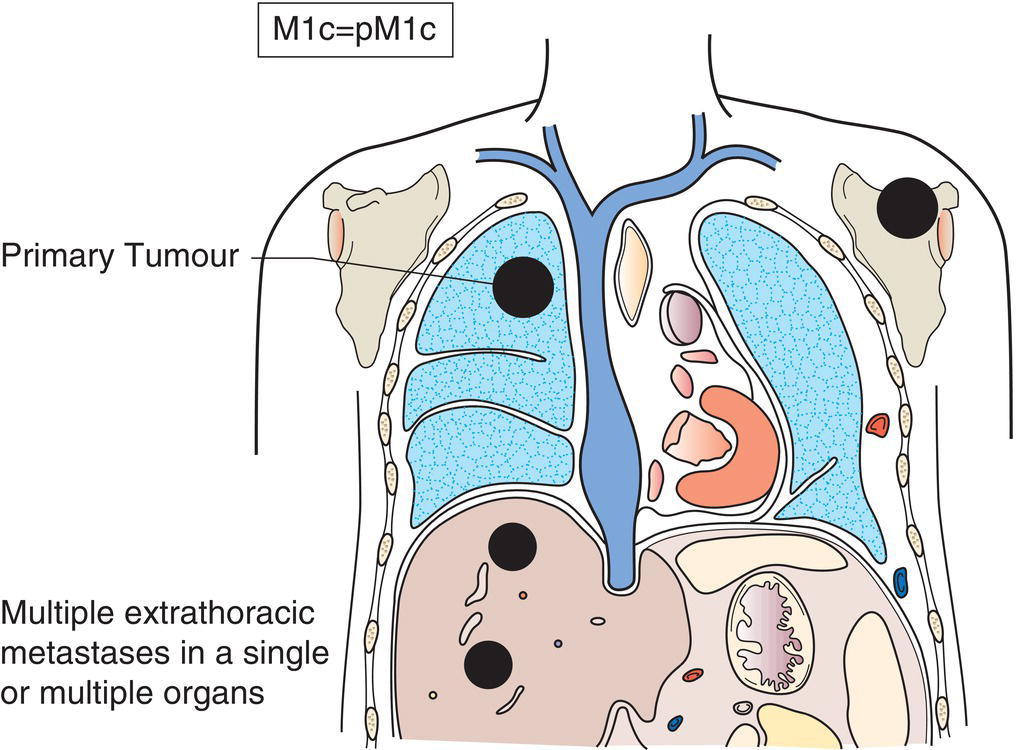
M1c
Multiple extrathoracic metastases in a single or multiple organ(s) (Fig. 287) 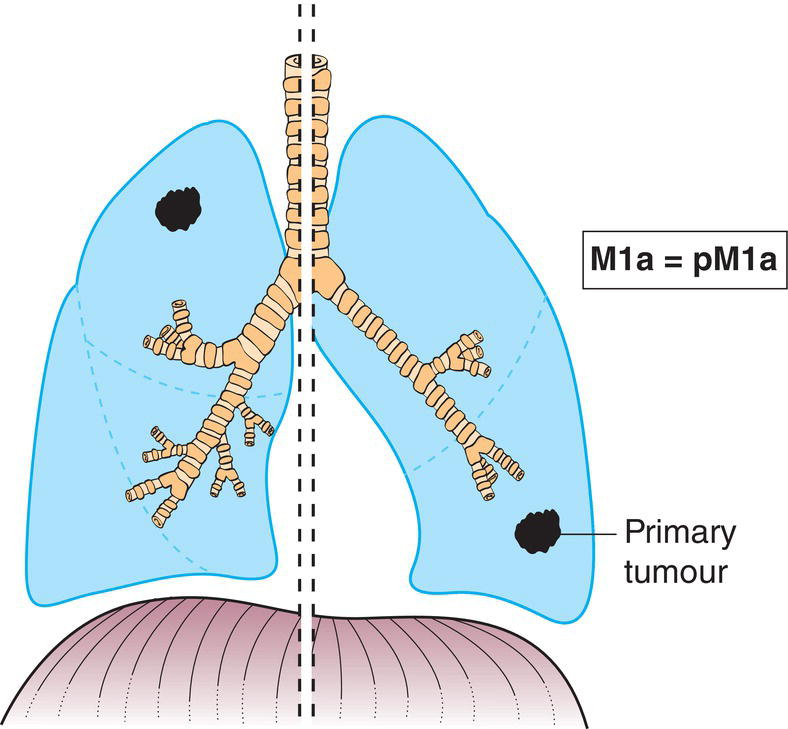
pTNM Pathological Classification
pM1
Distant metastasis microscopically confirmed
pN0
Histological examination of hilar and mediastinal lymphadenectomy specimen(s) will ordinarily include 6 or more lymph nodes/stations. Three of these nodes/stations should be mediastinal, including the subcarinal nodes, and three from N1 nodes/stations. Labelling according to the IASLC chart and table of definitions given in the TNM Supplement is desirable. If all the lymph nodes examined are negative, but the number ordinarily examined is not met, classify as pN0.
Summary
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree