Over the past several decades, three novel human herpesviruses (HHVs) have been identified and designated HHV-6, HHV-7, and HHV-8. HHV-6 has since been designated as two distinct species, HHV-6A and HHV-6B. HHV-6 was first isolated from the white blood cells of patients with human immunodeficiency syndrome and lymphoproliferative disease in the 1980s. The virus was initially designated as human B-lymphotropic virus, but the name was changed to HHV-6 once it was identified to preferentially infect CD4 T-lymphocytes rather than B cells . While pursuing additional strains of HHV6, HHV-7 was identified, a virus closely genetically related to HHV-6. HHV-8, also referred to as Kaposi sarcoma (KS)–associated herpesvirus, was identified while researchers were searching for the etiology of KS. HHVs 6, 7, and 8, like the other members of the HHV family, are double-stranded DNA viruses that establish a latent, persistent infection after primary infection. All three viruses can manifest active infection and, in some cases, disease in immunocompromised patients, either owing to reactivation of latent infection or transmission of infection from donors.
HHV-6A and HHV-6B are members of the β subfamily of the HHV, along with cytomegalovirus (CMV). HHV-6A and HHV-6B are closely related but have distinct biologic, epidemiologic, and clinical features. Although the natural history of HHV-6A is unknown, HHV-6B infects most people before the age of 3 years. Primary infection is characterized by a febrile illness often accompanied by respiratory symptoms, diarrhea, and rash. In a large proportion of immunocompromised patients, HHV-6B reactivates, and reactivation has been associated with fever, rash, bone marrow suppression, pneumonitis, acute graft-versus-host disease (GVHD), and graft rejection. In allogeneic hematopoietic stem cell transplant (HSCT) recipients, HHV-6B is the most common cause of encephalitis.
HHV-7 is also a member of the β subfamily of HHVs. In the majority of the population, HHV-7 antibody becomes detectable during childhood, where it has been implicated as an alternative cause of roseola, pityriasis rosea, and nonspecific febrile illness. HHV-7 infection is common after solid organ transplantation (SOT) but is transient and usually not associated with any clinical symptoms. There are few studies that have investigated HHV-7–associated disease, but viremia has been associated with febrile syndromes, thrombocytopenia, acute myelitis, and liver allograft rejection in a small number of studies and case reports. More frequently HHV-7 has been detected as a co-infection with CMV, but further studies are needed to determine if HHV-7 infection affects CMV disease.
HHV-8, or KS-associated herpesvirus, is a γ-herpesvirus along with Epstein-Barr virus (EBV), and like EBV, it is an oncogenic virus. HHV-8 contains a large number of genes that are transduced from the host cellular genome, a process known as molecular piracy. These genes can induce angiogenesis and cell growth while avoiding immune detection. Infection with HHV-8 is less common than HHV-6 and HHV-7, but in endemic areas typically occurs in childhood. Owing to immunosuppression of CD8 + response and lack of humoral immunity, uncontrolled HHV8 replication can lead to neoplastic disease, including KS. HHV-8 is also a rare trigger of hemophagocytic lymphohistiocytosis (HLH), a disorder of immune regulation.
Epidemiology and risk factors
Human herpesvirus 6
The natural history of HHV-6A is unknown. In contrast, HHV-6B infects most children before the age of 3 years and is characterized by fever, respiratory symptoms, diarrhea, and rash. In 25% of patients it causes roseola, an acute febrile illness defined by a maculopapular rash appearing as the fever declines. HHV-6B primary infection is also associated with febrile seizures and possibly epilepsy. Most HHV-6B transmission events are thought to occur via shared saliva early in life. Congenital infection had been estimated to occur in approximately 1% of births, although this is now recognized to be mostly the result of inherited chromosomally integrated HHV-6.
After primary infection, HHV-6B can establish latency in mononuclear cells and serve as a reservoir for endogenous viral reactivation. HHV-6B reactivates in approximately 40% of SOT recipients, typically within 2 to 6 weeks after transplantation or after episodes of rejection when they are receiving increased immunosuppression. HSCT recipients are at greatest risk of reactivation during the peri-engraftment period and after diagnosis of GVHD due to treatment with immunomodulatory medications. Patients receiving cord blood transplant are at an especially increased risk of HHV-6B reactivation, with rates as high as 80% to 90%. HHV-6B has been associated with a number of important outcomes, particularly in allogeneic HSCT recipients, including encephalitis, bone marrow suppression, pneumonitis, GVHD, and mortality. The evidence supports a causal association between HHV-6B and encephalitis, an outcome that is rarely reported in non-HSCT recipients. , A more specific entity, HHV-6B posttransplant acute limbic encephalopathy, has been estimated to occur in 0.7% of adult donor HSCT recipients and 9.9% of cord blood transplant recipients in the United States.
Reactivation of HHV-6B has been reported in up to 52% of adults receiving cytotoxic chemotherapy, although the clinical significance remains poorly understood. In pediatric patients, one study found that the incidence of HHV-6 DNA detected in blood rose from 17% at time of diagnosis to 37% during chemotherapy and was associated with fever.
The preferential target cell for HHV-6 is CD4 + lymphocytes; however, cellular host cells include CD8 + T lymphocytes, natural killer (NK) cells, macrophages, megakaryocytes, glial cells, and epithelial cells. HHV-6A and -6B establish latency by integrating into the telomere regions of the host chromosomes. When this occurs in a germ cell, it can result in chromosomally integrated HHV-6 (ciHHV-6), which can occur in an estimated 1% of the population. Affected individuals have the HHV-6 genome present in every cell of their body. As a result, affected individuals have persistently detectable HHV-6 viral DNA in tissues, blood, and cerebrospinal fluid (CSF). In addition, viral transcripts and antigens have been demonstrated in immunocompetent and immunocompromised patients with inherited ciHHV-6. , More recently, the majority of congenital infections have been shown to be due to ciHHV-6.
When ciHHV-6 is not recognized, it can lead to inappropriate treatment of patients. It is important to note that detection of viral DNA does not correlate with symptoms or signs of disease in patients with ciHHV-6. However, there is some evidence that ciHHV-6 can lead to active viral infection and symptomatic disease in severely immunocompromised patients.
Human herpesvirus 7
Most people become seropositive for HHV-7 at a slightly later age than HHV-6B, typically by 5 years of age. Transmission of HHV-7 is similar to other HHVs, typically through shared saliva. HHV-7 exhibits selective tropism for CD4 + cells, using the CD4 cell receptor for entry. HHV-7 has been described as slower to replicate than HHV-6 and less lytic, with the cytopathic effects similar to HHV-6 but less pronounced. Salivary glands are the major identified site of persistence and replication.
Similar to HHV-6B, HHV-7 may reactivate in SOT recipients. HHV-7–seropositive pediatric patients have been shown to have a 20% to 60% incidence of HHV-7 DNA detection 2 to 6 weeks after transplant. Most reactivation is brief with minimal viremia. Specific risk factors for reactivation have not been clearly defined. Primary infection can also occur in SOT recipients who were seronegative before transplantation. HHV-7 infections are rarely symptomatic in SOT recipients, but rare cases of tissue-invasive disease have been reported and are often associated with other viral infections, including CMV or EBV.
Human herpesvirus 8
HHV-8 has a broad cellular tropism, including infection of B cells, endothelial cells, macrophages, and epithelial cells. Similar to HHV-6 and HHV-7, primary infection is most often through saliva and can be transmitted from caregivers to children through premastication. It can also be spread through infusion of contaminated blood products. HHV-8 seropositivity rises throughout adolescence and varies geographically. HHV-8 seropositivity is lower in North America compared with countries where it is considered endemic. In Israel, 9% of children and up to 18% of adults are seropositive compared with less than 5% of human immunodeficiency syndrome–negative adults in the United States. HHV-8 seropositivity occurs more often in children whose parents are seropositive, with maternal seropositivity being the most important risk factor.
KS has only rarely been reported in HSCT recipients. KS lesions in transplant recipients can develop as the result of reactivation of latent virus or via transmission of the virus or KS lesions from the allograft. In SOT recipients, most KS (80%) appears to result from reactivation of latent virus. The incidence of KS varies geographically and is dependent on local seroprevalence of HHV-8. KS affects less than 1% of transplant recipients in the United States and has been reported as low as 0.1% in central Europe. In areas of high seroprevalence, KS can account for the majority of posttransplant malignancies . In posttransplant recipients who were previously positive for HHV8, increased immunosuppression can lead to of development of lesions and progression of disease, but no specific regimen is associated with increased risk. The risk of disease decreases with time after transplant. In addition to KS, HHV-8 has also been associated with other malignancies, including primary effusion lymphoma and multicentric Castleman disease, a B-cell lymphoproliferative disease. HHV-8 can also be a trigger for HLH.
Clinical manifestations
HHVs can have direct and indirect sequelae. Indirect sequelae have been described as immunomodulatory effects that may increase risk of co-infections with other viruses, specifically CMV, and/or potentially lead to outcomes such as GVHD and organ rejection. HHV-6B infection has been identified in several studies as a significant risk factor for symptomatic CMV disease in both liver and kidney transplant recipients. In the following text we discuss the clinical manifestations for HSCT recipients, SOT recipients, and oncology patients specifically.
Hematopoietic stem cell transplant
The majority of HHV-6B reactivation episodes in HSCT recipients are asymptomatic, transient, do not impact overall survival, and do not require antiviral treatment. HHV-6 has been commonly associated with fever and rash after transplantation, and common hematologic effects associated with HHV-6B infection include delayed platelet engraftment and leukopenia. HHV-6 has also been associated with pneumonitis and hepatitis. There is strong evidence that HHV-6B causes encephalitis, particularly after allogeneic HSCT. In most reports and studies of HHV-6B encephalitis, it is defined as encephalopathy without another cause identified. HHV-6B encephalitis in HSCT recipients presents with symptoms that commonly include confusion and altered consciousness. Other symptoms may also include seizures, amnesia, and syndrome of inappropriate antidiuretic hormone secretion. Laboratory findings may include mild CSF pleocytosis and elevated protein. Distinct imaging findings are medial temporal lobe changes on brain magnetic resonance imaging (MRI). HHV-6B–associated posttransplant acute limbic encephalitis is defined by anterograde amnesia, syndrome of inappropriate antidiuretic hormone, mild CSF pleocytosis, temporal electroencephalogram abnormalities, and MRI hyperintensities in the limbic system.
HHV-7 reactivation is rarely associated with clinical symptoms, although it has been suggested that HHV-7 also can be associated with higher CMV viral loads and delayed clearance of viremia.
HHV-8 reactivation or primary infection after HSCT has rarely been reported in the absence of malignant disease. Studies of the natural history of viral reactivation after HSCT are lacking; other than malignancy, the frequency and outcome of viral reactivation has not been well described. Clinical symptoms described include fever, rash, hepatitis, and bone marrow failure. HHV-8 has rarely been reported to cause KS in HSCT recipients. Symptoms of KS in HCT recipients can include graft failure and pancytopenia in addition to skin lesions. The median time of onset has been reported as 8.5 months after HSCT, and diffuse disease developed in 50% of these patients, with mortality rates reported up to 70%.
Solid organ transplant
The most common clinical syndrome of HHV-6B infection in SOT recipients is a nonspecific febrile illness occasionally associated with rash. HHV-6B infection can also have marrow-suppressive effects, including chronic myelosuppression, but this is more frequently seen in HSCT recipients, as described earlier.
HHV-6B has also been associated with significantly higher mortality after liver transplant and has been linked to a higher risk of invasive fungal infections after transplant, likely owing to immunomodulatory effects. HHV-6B has been associated with increased severity of hepatitis C recurrence in positive recipients but is not clearly an independent risk factor for recurrence. This may be clinically relevant as hepatitis C mismatch transplants are increasing.
HHV-7 viremia has been detected after transplant and has been considered as a possible cofactor in CMV disease after SOT. In one study, renal transplant recipients in whom both CMV and HHV-7 were detected had more severe CMV disease. HHV-7 has also been reported in association with pneumonia and bronchiolitis obliterans in a lung transplant recipient.
HHV-8 can lead to KS in SOT recipients, and the disease can be rapidly fatal if not identified in a timely fashion. HHV-8 can also be inciting factor for development of HLH. In addition, nonneoplastic lesions have been associated with HHV-8, including cytopenias and hepatitis.
Oncology
Owing to multimodal treatment with chemotherapy, risk of reactivation persists throughout treatment, peaking during times of intense immunosuppression. Similar to HSCT recipients, reactivation often occurs as a co-infection with CMV and EBV. Most HHV6 and EBV reactivations in the first 100 days of chemotherapy are subclinical. Severe HHV-6 disease is rare, but detection of HHV-6 DNA is more commonly associated with fever, lymphopenia, rash, and hepatic dysfunction.
More studies are needed to determine the frequency of reactivation of HHV-7 in patients with oncologic malignancies and receiving chemotherapy and the clinical impact. Severe disease is rarely reported.
HHV-8 has been linked to several lymphoproliferative diseases, including KS and multicentric Castleman disease, plasmablastic lymphoma, and primary effusion lymphoma in oncology patients. Patients with chronic blood disorders or underlying immune dysfunction have been described at greater risk of developing malignancy from this virus, and HHV-8 is considered a predisposing factor for several malignancies.
Disease prophylaxis/prevention
Small studies exploring the utility of antiviral prophylaxis or preemptive therapy with ganciclovir or foscarnet for HHV-6B have been performed in SOT and HSCT recipients with variable results. Although these antiviral agents may reduce the rate or delay HHV-6B reactivation, evidence is lacking to support prophylaxis or preemptive monitoring and treatment aimed at preventing HHV-6B–associated disease.
Preemptive testing for HHV-7 and HHV-8 viremia is not routinely recommended after transplant. Antiviral prophylaxis does not appear to alter the appearance of HHV-7. ,
Primary infection with herpesviruses can be acquired through sexual activity, contaminated blood products, or close nonsexual contact owing to active shedding in saliva. Patients at risk should be encouraged to limit any high-risk behaviors, including practicing safe sex and avoidance of premastication.
Diagnosis
Human herpesvirus 6
Direct viral detection is the preferred method for identifying HHV-6B after transplantation. Viral serologic test results are not helpful given the high prevalence of latent infection, limitations in the available assays, and the immunocompromised state of the targeted patient population. Detection of viral nucleic acids also allows differentiation between HHV-6A and HHV-6B.
Detection of viral DNA by PCR may reflect active or latent infection, depending on the specimen tested. Quantitative viral DNA PCR obtained on noncellular samples such as serum, plasma, or CSF has been shown to correlate with active viral replication and is the most studied and widely available method available. Quantitative assays also allow for the potential of risk assessment as higher viral loads have been more predictive of encephalitis in some studies. Quantitative assays may also help determine trends over time. If whole blood samples are used, it is important to have established thresholds for significance levels owing to the presence of latent virus in peripheral blood mononuclear cells. Reverse transcriptase PCR on whole blood might be the best indicator for active viral replication. However, this test is not commercially available and has also not been studied to determine its ability to predict clinical outcomes.
Detection of HHV-6B in CSF in a patient with acute encephalopathy is generally considered diagnostic of HHV-6B encephalitis in the absence of another etiology of encephalopathy. In a small percentage of patients, HHV-6 has been detected in the CSF in the absence of symptoms. Patients with acute encephalopathy without a clear etiology should have serum or plasma and CSF tested for HHV-6B, and empiric antiviral therapy should be initiated while results are pending. It is important to note that detection of virus in blood or CSF may underestimate tissue-level disease. Despite clearance from CSF or blood, virus may persist in tissue for a prolonged time. CSF findings and results from brain imaging can help in the diagnosis of HHV-6B encephalitis. CSF studies in patients with HHV-6 encephalitis generally demonstrate mild pleocytosis and elevated protein levels. Brain MRI findings consistent with HHV-6B encephalitis include medial temporal lobe changes, typically described as well-circumscribed, hyperintense, nonenhancing lesions involving the medial and temporal lobes, especially the hippocampus.
Persistent high levels of HHV-6 in blood, with or without treatment, should raise suspicion for ci-HHV6. Diagnosis of ci-HHV6 can be confirmed with fluorescence in situ hybridization analysis demonstrating the virus integrated in the chromosome, or alternatively, by testing tissues that would not normally have detectable HHV-6, such as hair follicles. However, these methods are not widely available. More recently, digital droplet PCR methods have been developed for detection of ciHHV-6. In this case, the ratio of viral to human genomes at 1:1 is highly suggestive for the presence of ci-HHV6.
HHV-6 quantitative PCR (serum or plasma) should be performed for the following groups of patients:
- 1.
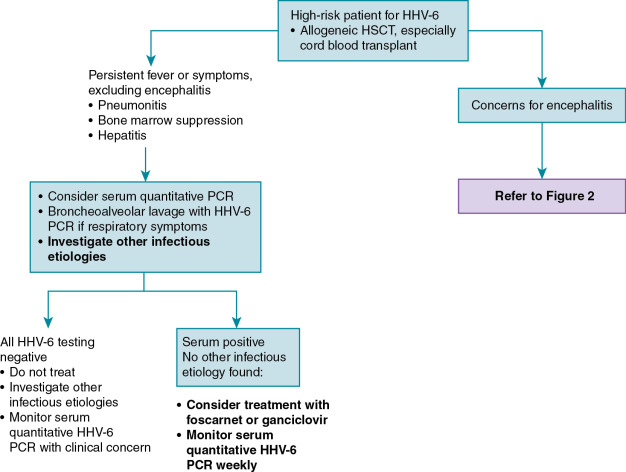
Posttransplant or severely immunocompromised patients with encephalopathy or encephalomyelitis. CSF should also be obtained for HHV-6 testing ( Fig. 20.1 ).