HL is characterized by a few scattered neoplastic HRS cells that account for 0.1% to 10% of the total cell population of the tumor infiltrate. Most of the infiltrate is composed of nonneoplastic background inflammatory cells (histiocytes, plasma cells, lymphocytes, eosinophils, neutrophils) and fibrosis that develop as a result of cytokines. HL must be differentiated from several subtypes of NHL with similar morphologic characteristics (T-cell-rich large B-cell lymphoma and anaplastic large cell lymphoma) and from benign lymphoid hyperplasia with a similar cellular composition (e.g., infectious mononucleosis, progressive transformation of GCs).
36 In addition, less common variants of HL (e.g., lymphocyte depleted and syncytial variants) may overlap morphologically with nonhematopoietic malignancies, such as carcinomas and sarcomas. With the advent of widely available immunohistochemical staining, the latter entities are usually easy to exclude.
Definition of Histologic Subtypes
The current WHO histologic classification of HL is largely based on the Rye modification of the Lukes and Butler classification schema. The WHO classification
13 recognizes two major subtypes of HL—classical HL (cHL) (
Figs. 22.1a and
22.2a) and nodular lymphocyte-predominant HL (nLPHL) (
Figs. 22.1b and
22.2b)—based on their histology and immunohistochemical staining pattern (
Tables 22.2 and
22.3). For example, the HRS cells in nLPHL are usually mononuclear with markedly convoluted and lobated nucleus (“popcorn cells”), thin nuclear membrane, pale chromatin, and one-to-several small basophilic nucleoli (
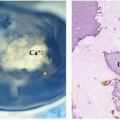
Fig. 22.1b). These HRS variants are also called lymphocytic and histiocytic (L&H) cells. In contrast, the HRS cells of cHL are typically large (≥15 to 45 µm in diameter), with abundant slightly basophilic cytoplasm, two nuclei or two nuclear lobes, and prominent eosinophilic large nucleoli (
Fig. 22.1a).
cHL is further subdivided into four histologic subtypes based on the tissue architecture, the presence of fibrosis, and the features of the associated inflammatory infiltrate (
Table 22.2). Historically, prognosis for some of the categories of HL was linked to the ratio of lymphocytes to abnormal cells. Since the development of highly curative treatment regimens, however, all histologic subtypes of HL are equally responsive to treatment.
In all four subtypes of cHL, the HRS cells are B cells with clonal immunoglobulin heavy-chain rearrangement but lack many immunohistochemical evidence of B-lineage differentiation. The HRS cells are negative for leukocyte common antigen (CD45), B-lineage antigens (such as CD19, CD20, CD79a, OCT2, BOB1, and J chain), and BCL6. In a limited number of cases (10%-20%), the cHRS cells may express CD20 or CD79a with variable intensity. Of the B-cell-specific antigens detected by immunohistochemistry, PAX5/BSAP is the most useful as 98% of cHL cases have dim expression of PAX5 in the HRS cells. HRS cells retain molecules important in B-T-cell interactions, such as CD80, CD86, and MHC class II, and often express molecules typically upregulated in plasma cells (CD138 and MUM-1).
37,38 HRS cells characteristically coexpress the non-B-cell-specific CD15 (LeuM1) and CD30 (Ki-1) antigens. Finally, in a minority (2%) of cHL cases, the HRS cells show a cytotoxic T-lymphoid immunophenotype that may be associated with a B-cell genotype or harbor T-cell receptor beta gene rearrangements.
37,39,40Unlike cHL, nLPHL have HRS cells that consistently show immunophenotypic evidence of B-lineage differentiation and express CD45, CD20, CD79a, J chain, OCT2, and BOB1, in addition to PAX5. Furthermore, HRS cells of nLPHL lack expression of non-B-cell antigens CD15 and CD30, typically seen in cHRS.