Background
In the elderly population, hip fracture is the most common cause of unplanned admission to an acute orthopaedic ward1 and the second cause of hospital admission in general. The incidence of such fractures has been constantly increasing over the last 70 years and, if we are to believe the demographic projections, it will increase even further. The overall number of fractures, which was 1.6 million per year in 1990, should reach 4 million in 2025 and 7–21 million in 2050.2 This ‘orthopaedic epidemic’ raises major medical, economic and social problems and is a challenge in terms of public health, if we wish to promote prevention and develop the least costly and most effective mode of management.
The risk of hip fracture increases exponentially from the age of 60 and 75% of these fractures occur in women, who are at greater risk because of their longer lifespan and high prevalence of osteoporosis. Femoral neck fracture has many causal factors, associating osteoporosis and falls, the prerogative of ‘frail’ subjects. It is a hallmark of ageing, as it primarily affects persons with the highest comorbidity (29% have respiratory disorders, 55% have dementia and 68% have cardiorespiratory diseases), who make the greatest demands on home care structures and the most use of walking aids. Nursing home residents are three to four times more likely to be affected as they combine several risk factors (advanced age, low bone mass, impaired mobility, cognitive disorders).
subjects. It is a hallmark of ageing, as it primarily affects persons with the highest comorbidity (29% have respiratory disorders, 55% have dementia and 68% have cardiorespiratory diseases), who make the greatest demands on home care structures and the most use of walking aids. Nursing home residents are three to four times more likely to be affected as they combine several risk factors (advanced age, low bone mass, impaired mobility, cognitive disorders).
In spite of advances in surgery, anaesthesia and rehabilitative management, hip fracture still has a poor vital and functional prognosis. Depending on the studies, mortality ranges from 5 to 10% in the first month and one-third of elderly patients die within 1 year of fracture, whereas the expected annual mortality in a population of the same age is 10%.3 These figures have not changed for over 20 years. However, only one-third of these deaths are directly attributable to the fracture and in the remaining cases comorbid disorders are the explanatory factor. The criteria of poor prognosis are advanced age, male gender, poorly controlled comorbid conditions, cognitive disorders, low autonomy and institutionalization.
Proximal femoral fracture is a turning point for the worse in the life of the elderly person and it often leads to loss of independence and social decline, marked by admission to an institution. Only half of patients regain their earlier walking ability. The factors of a good functional prognosis are the absence of cognitive disturbances, the ability to walk unaided with a device prior to fracture, rich social contacts and pursuit of an activity outside the home. About 10–20% of patients remain dependent for their activities of daily living (ADL) and must be placed in a nursing home.
The costs relating to management of femoral neck fracture are high because of the length of hospital stay (2–5 weeks) and the costs incurred for subsequent care due to dependence. According to Dolan and Torgerson,4 they reach  20 000 for the first 2 years.
20 000 for the first 2 years.
It therefore seems necessary to reflect on multidisciplinary management as soon as the patient is admitted and on the implementation of surgical and rehabilitative strategies that are adapted to the elderly person’s specific needs if we wish to improve the outcome of these patients, who will be increasingly numerous due to lengthening life expectancy.
Diagnosis and Classification
Usually, the diagnosis of hip fracture poses few problems. After a fall from a standing position, the patient complains of pain causing functional disability. A characteristic deformity is observed, associating shortening and external rotation of the leg. Inability to raise the heel above the bed surface with the leg extended is a suggestive sign.
Diagnosis is confirmed by radiography. Anterior images of the pelvis should be obtained with the lower limbs in 10° internal rotation, with a lateral view and sometimes a third anteroposterior view centred on the affected hip in 10° internal rotation.3 However, it is often not easy to obtain satisfactory images because of the patient’s pain. In difficult cases, where there is a discrepancy between X-ray and clinical findings, fracture can only be excluded by radioisotope bone scan or magnetic resonance imaging (MRI) (the investigation of choice for non-displaced fractures). Bone scan seems to be less informative in this context, but it is easier to obtain within the short time needed for rapid initiation of treatment.
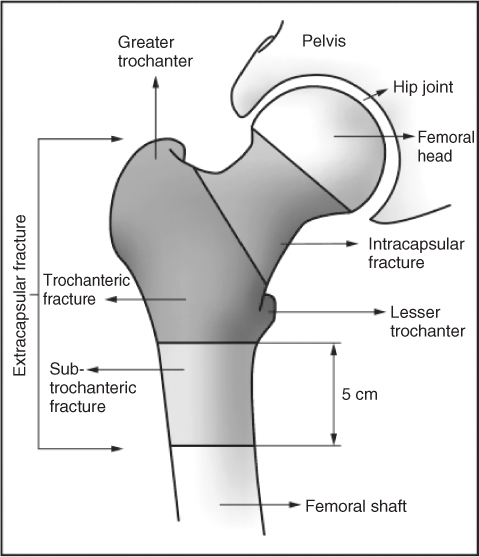
The radiological investigations allow the classification of the fractures according to the location of the fracture line and the degree of displacement, on which the choice of treatment depends. An anatomical and pathophysiological distinction is made between intra- and extracapsular fractures, whose prognoses differ (Figure 93.1).
Intracapsular fractures (45%) lie between the femoral head and the trochanters within the capsule, whether this is intact or not. They can lead to high-pressure haemarthrosis if the capsule remains intact after injury. These fractures may be displaced or non-displaced. The predominant risk is necrosis of the femoral head, secondary to vascular damage. The arterial branches that feed the femoral head are at risk of being lacerated or stretched by the displacement or may also collapse because of the increased pressure due to accumulation of blood caused by haemarthrosis in an intact capsule.
Extracapsular fractures are metaphyseal fractures that always heal. They often lead to major bleeding. They are divided into two groups:
- fractures of the greater trochanter (45%), which are stable if there is a single fracture line and unstable if there are several lines
- subtrochanteric fractures (5–10%), which lie within 5 cm distal to the lesser trochanter.
Preoperative Care
Analgesia
There is now a general consensus that pain needs to be managed in the emergency situation. Relief of pain reduces the neuroendocrine disturbances that follow the trauma, decreases the patient’s agitation that can lead to secondary displacement of the fracture site and makes preoperative investigations easier. Pain is judged by repeated self-assessment. A simple verbal scale (from 0, no pain, to 4, extreme pain) is preferable to the visual analogue scale in the elderly person, who may find it difficult to cooperate.
In general, level 1 analgesics (paracetamol) used alone do not adequately relieve pain. They should be prescribed in association with a level 2 analgesic (codeine) or a morphine derivative. As a parenteral approach is often necessary, the dose of morphine derivatives must be carefully titrated in these frail patients. Non-steroidal anti-inflammatory drugs (NSAIDs) are inadvisable in the elderly patient as the risk of haemorrhage is increased by stress and because of pre-existing renal failure.
Peripheral blocks have considerably improved pain management in femoral neck fractures. An iliac fascia block carried out as soon as the patient has been admitted to the emergency department allows them to be mobilized and prepared for surgery.
Preoperative Traction
Both skin and skeletal traction have been proposed in order to reduce pain and to facilitate fracture reduction. However, the studies available5 have not provided sufficient evidence of sedation of pain in the first 2 days after surgery {relative risk (RR) = 1.14 [95% confidence interval (CI), 0.89–1.46]} and RR = 1.02 (95% CI, 0.74–1.41)] or of easier fracture reduction at the time of surgery.
Electrolyte Balance and Blood Transfusion
In the elderly person with hip fracture, electrolyte imbalance is frequent and due to a variety of causes, such as renal failure, diabetes and diuretic medications. Patients are often dehydrated, either because they lay on the ground for several hours or because of preoperative fasting. These imbalances should be corrected, while taking into account the borderline tolerance of volume restoration in elderly patients.
Anaemia, particularly frequent in fractures of the greater trochanter, increases the mortality rate at 6 and 12 months, lengthens the duration of hospital stay and compromises the functional prognosis.6 The transfusion threshold is still difficult to establish, but it is generally accepted as 8–9 g dl−1 for elderly patients with no cardiovascular history and 10 g dl−1 for patients with poor tolerance or severe cardiovascular involvement.
Thromboembolic Prophylaxis
Following proximal femoral fracture, the risk of thromboembolism is increased. The incidence of proximal thrombosis is 27% and mortality due to pulmonary embolism is 1.4–7% in the first 3 months after surgery.7 In view of these figures, the absence of thromboprophylaxis may be considered as negligence. A Cochrane review of 31 studies (2858 participants) clearly demonstrated the efficacy of prophylactic treatment in reducing the incidence of deep venous thrombosis (DVT) and pulmonary embolism.8 The modalities of management, however, still remain to be defined: the respective roles of pharmacological and physical methods, optimal duration of treatment. Several therapeutic protocols are under discussion:
- Administration of unfractionated heparin or low molecular weight heparin versus placebo (15 trials, 1199 participants) significantly reduced the risk of DVT [RR = 0.60 (95% CI, 0.50–0.71)], but evidence regarding pulmonary embolism was inadequate. Low molecular weight heparins were not more effective than fractionated heparins.
- Low-dose aspirin appears likely to decrease the incidence of DVT and pulmonary embolism.
- Antivitamin K agents may also be given during the first 10 days after surgery if a target international normalized ratio (INR) of 2.5 (min.–max. 2.0–3.0) is maintained.
However, we need to be aware that use of anticoagulants or antiplatelet agents increases the number of haemorrhagic complications.
The optimal duration of treatment9 is still unclear. In general, it is continued for 14 days after surgery. The Seventh American College of Chest Physicians Conference on Antithrombotic and Thrombolytic Therapy10 recommended that heparin should be given for at least 10 days after surgery. However, it has been demonstrated that even with anticoagulation treatment, thrombosis occurs in 15–30% of patients at discharge and that 10–25% of patients develop thrombosis 3–4 weeks later; these thromboses are symptomatic in less than 10% of cases. Eriksson and Lassen11 showed that 4 weeks of heparin treatment reduced the incidence of pulmonary embolism compared with 1 week of treatment.
When surgery is deferred, initiation of anticoagulation treatment is recommended between admission and the surgical procedure.
Physical treatments have also been proposed. Mechanical pumping devices are more effective than no treatment [RR = 0.31 (95% CI, 0.12–0.51)] and they significantly reduce the risk of DVT and pulmonary embolism, but skin abrasions have been reported.8 As for compression stockings, it is difficult to reach a conclusion regarding their efficacy.
Lastly, it is important to note that no method makes it possible to reduce the number of fatal pulmonary embolisms, or the mortality after hip fracture.
In addition to specific treatments, it is therefore important to give a considerable place to general measures1 such as:
- combat against dehydration and excessive transfusion
- minimization of surgical delay and duration of the procedure
- early mobilization of the patient.
Minimizing Surgical Delay
The Royal College of Physicians’ guidelines12 recommend early surgery (within 24 h of admission). However, after analysis of 10 studies with a satisfactory level of proof, Beaupre et al.7 emphasized that divergent results were obtained when surgical delay was taken into account. With regard to post-surgical mortality, Grimes et al.,13 after adjustment for comorbid conditions, observed no differences between patients operated on after more that 96 h and those operated on within 48 h [HR = 1.01 (95% CI, 0.95–1.21)]. Conversely, Shiga et al.14 carried out a meta-analysis of five prospective and 11 retrospective studies which showed that operative delays of more than 48 h increase 30 day mortality by 41% and mortality at 1 year by 32%. Excess mortality is particularly high in patients aged <70 years with no comorbid conditions. Most authors15, 16 agree that early surgery decreases the risk of postoperative complications such as pressure ulcers, urinary infections, thromboses and pneumonia, but that it sometimes increases the risk of postoperative bleeding and prosthesis-related complications.16 Several authors also report that early surgery shortens hospital stay,15 encourages earlier resumption of walking and reduces pain.
These arguments favour early surgery for younger, clinically stable patients. In other cases, it is important that existing comorbidities should be rapidly controlled before considering surgery.
Prevention of Pressure Ulcers
Following hip surgery, 10–40% of patients develop a pressure ulcer. This complication increases the burden of care, risk of nosocomial infection and duration of hospital stay. The heel is particularly at risk due to increased pressure on the operated side (immobility of the patient) and on the uninvolved side, because the patient uses the heel as a pivot to move in bed. These mechanical factors are augmented by haemodynamic factors: decreased local blood flow due to elevation of the operated limb during the procedure, fluctuations in blood volume due to anaesthesia and blood loss and sometimes episodes of low blood flow rate related to the cement used in total hip replacement. In these circumstances, bilateral pressure ulcers are observed.17
Two studies7 assessed the preventive efficacy, in orthopaedic surgery, of foam or dynamic air mattresses and showed that their use reduced the incidence of pressure ulcers [RR = 0.34 (95% CI, 0.14–0.85) and RR = 0.20 (95% CI, 0.009–0.45)]. These means of prevention are effective above all for the sacrum and trochanter. A meta-analysis18 exclusively centred on the prevention of heel ulcers showed that special foam or dynamic air mattresses were superior to standard hospital mattresses. With regard to heel pads and mattress overlays, the evidence was inadequate to reach a conclusion regarding their efficacy.
Overall, rational use of preventive aids (mattresses, heel supports, mattress overlays) is recommended based on evaluation of the patient’s risk level using specific scales (see Chapter 126, The prevention and management of pressure ulcers).
Fracture Repair and Perioperative Care
Surgical Management
The majority of hip fractures are treated surgically, although conservative treatment, used before the advent of the first prostheses, may still be debated.
Conservative or Operative Treatment
Handoll and Parker, in a Cochrane review of five randomized trials (428 elderly subjects), compared surgical treatment and conservative treatment (traction and bed rest).19 A study of 23 patients with non-displaced intracapsular fractures showed a lower risk of non-union in surgically treated patients. The other trials relating to extracapsular fractures found no difference in mortality, medical complications or pain between the two treatment modalities, whatever the prosthesis or surgical technique used. However, deformity and limb shortening were less frequently observed with surgical treatment (better anatomical reduction), duration of hospital stay was shorter and functional results were better. Conservative treatment should be the exception today, reserved for patients with formal contraindications to surgery, those who refuse it or those who are at the end of life.
Operative Treatment
Undisplaced Intracapsular Fractures
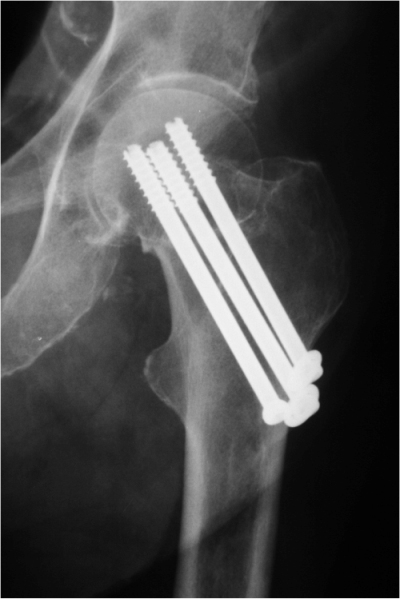
Only internal fixation is recommended, as it reduces the risk of displacement. The surgical procedure is simple and can be carried out by a percutaneous approach under local anaesthesia or peripheral block. Two or three screws are used in parallel (Figure 93.2) or a sliding hip screw (SHS). This technique has the advantages of being conservative and of making nursing care easier. Active mobilization of the hip and knee can rapidly be started.
Displaced Intracapsular Fractures
Two options are possible: internal fixation or prosthetic replacement. Each treatment carries specific complications.
Internal fixation is a shorter procedure, with less blood loss and less risk of infection; the main complications are non-union and avascular necrosis of the femoral head, requiring revision in 35–50% of cases.
Several types of prostheses may be used:
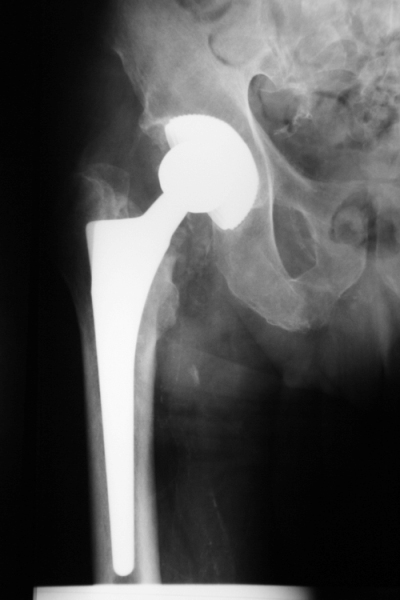
- Cervicocephalic hemiarthroplasty prostheses (Figure 93.3) of Moore or Thompson type replace only the femoral head. They are non-cemented and are inserted as a press-fit in cancellous bone.
- Bipolar hemiarthroplasty prostheses (Figure 93.4) have a femoral part with a mobile acetabular socket joint which is intended to protect the acetabulum and to delay the development of mechanical complications.
- Total prostheses (Figure 93.5), very widely used in the surgical treatment of coxarthrosis, replace the entire coxofemoral joint.
Prostheses may be cemented or uncemented. Randomized trials comparing cement with cementless devices are summarized in a Cochrane review.20 Cemented prostheses are less painful and the functional results are better, but with the drawback of a more lengthy and major surgical procedure (risk of cardiovascular collapse, toxic effects of cement). Mortality is not increased at 1 year.
A Cochrane review compared the two operative techniques (internal fixation and hip replacement) in the adult.21 The results did not differ in terms of mortality, but postoperative pain was less and the functional results were better after hip replacement. An observational study,22 based on the Norwegian register of hip fractures and including 1569 subjects aged over 70 years operated on for femoral neck fracture, stressed that patients who underwent bipolar arthroplasty had a better quality of life at 4 months than those treated by internal fixation. They had less pain and were more satisfied with the intervention. Arthroplasty also gives better results in severely demented patients. however, the superiority of prostheses is apparent essentially for the most modern bipolar prostheses (hydroxyapatite) and for cemented prostheses.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree