Herpes simplex virus (HSV) types 1 and 2 (HSV-1 and -2) and varicella-zoster virus (VZV) comprise the human α-herpesviruses, a subfamily of enveloped, double-stranded DNA viruses defined in part by the ability to be transmitted and replicate in mucoepithelial surfaces and to establish latent infection in sensory ganglia of the nervous system. Infection with HSV is common, with serologic evidence of HSV-1 infection in about 48% and HSV-2 infection in about 12% of 14- to 49-year-old people living in the United States. The incidence of infection with either serotype has declined in the United States in the past decade. However, globally the prevalence is quite high with an estimated 3.7 billion people infected with HSV-1 and 0.4 billion with HSV-2. VZV causes the formerly common childhood disease known as chickenpox. A live-attenuated vaccine protecting against VZV disease has been available in the United States since 1995, with a Centers for Disease Control and Prevention recommendation for 2 doses since 2006. This has led to dramatic decreases in VZV cases.
Both HSV and VZV uniformly establish latency in neuronal cells and periodically reactivate to cause cutaneous, or less commonly, neurologic or disseminated disease. Clinically silent HSV reactivation is far more common than previously recognized and the long-term consequences of this are not yet fully understood. Clinical recurrences typical manifest as painful eruptions of grouped vesicles. These are generally self-limited but may be associated with variable levels of viral DNA detected in the blood using quantitative polymerase chain reaction (PCR) assays (referred to as DNAemia). VZV reactivation, which occurs less frequently than HSV reactivation, presents clinically as zoster or shingles and manifests as a painful, dermatomal vesicular rash. Zoster is most common in adults older than 60 years or in immunocompromised patients, including transplant recipients. Zoster-associated pain can persist well beyond the duration of the rash and may occur in the absence of rash. Transmission of VZV is less common with zoster than with primary varicella, reflecting lower viral loads, but may contribute to an increasing proportion of varicella cases in the postvaccine era. Both wild-type and the vaccine strain (vOka) of virus may reactivate, although reactivation occurs far more frequently with wild-type viral strains. Moreover, a new subunit protein vaccine (Shingrix, GlaxoSmithKline) provided 97% protection against zoster and was approved by the U.S. Food and Drug Administration at the end of 2017 for adults older than 50 years. Thus the overall incidence of shingles, which has already decreased with the implementation of the live vOka vaccine for primary varicella and zoster, will undoubtedly continue to decline with the introduction of this new and highly effective subunit protein zoster vaccine.
Herpes simplex virus in transplant and oncology
Epidemiology and risk factors
There are limited data on the epidemiology of HSV infection in pediatric oncology or transplant patients. In the general population, the most recent large-scale U.S studies indicate a prevalence of approximately 27% for HSV-1 and less than 1% for HSV-2 among 14- to 19-year-olds. Rates of HSV-1 infection are likely higher in developing countries. HSV clinical disease is more common in stem cell transplant (SCT) patients than in cancer and solid organ transplant (SOT) patients, reflecting the greater net state of immunosuppression. HSV disease may develop in up to 80% of HSV-seropositive SCT patients without prophylactic antiviral treatment. In contrast to other herpesviruses such as CMV or Epstein-Barr virus, in which the donor is often the source of infection, HSV disease almost always reflects reactivation of latent virus in the recipient and/or primary community-acquired infection. Donor-derived HSV infection is rare because the virus, which is latent in sensory neuronal cells, is rarely transferred, except in unusual instances in which a donor has significant DNAemia and/or disseminated HSV disease. Reactivation of latent HSV may occur in HSV-seropositive SOT recipients who are not receiving antivirals for CMV prophylaxis.
Specific triggers for HSV reactivation independent of immune status include stress, ultraviolet light exposure, and disruption of the epithelial barrier. A quantitative or functional reduction in cellular, humoral, or innate (natural killer cells) immune responses also increases the risk of HSV reactivation. Notably, neutropenia alone has not been recognized as a trigger.
Clinical manifestations
HSV manifests clinically as oropharyngeal, nasolabial, ocular, esophageal, pulmonary, genital, and less commonly, meningoencephalitis or disseminated disease. Oncology patients and transplant recipients are at risk for more severe and prolonged symptoms with each of these diseases and are at greater risk for viral dissemination compared with immunocompetent hosts. The duration and severity of disease and likelihood of clinical recurrences are affected by the net state of immunosuppression. ,
The most common clinical syndrome associated with primary or recurrent HSV is gingivostomatitis. , HSV is readily detected in oral secretions during episodes of stomatitis, but it may also be detected in absence of symptoms, complicating the interpretation of causality. An important, but relatively uncommon, complication of herpes stomatitis is Stevens-Johnson syndrome. Local dissemination of primary oral HSV or reactivation of virus from the trigeminal ganglia may lead to ocular disease, including keratitis or uveitis, with potentially devastating outcomes.
HSV-associated esophagitis may occur in the setting of mucositis, a common sequela of chemotherapy, radiation therapy, and/or graft-versus-host disease (GVHD). Nasogastric tubes may also disrupt the epithelial barrier and promote viral spread to the esophagus. Esophagitis may be polymicrobial with HSV, CMV and Candida species being detected. Early endoscopic findings include vesicles, which may progress to diffuse mucosal necrosis.
Pulmonary infection has been recognized more frequently in the past decade, reflecting the advent of molecular testing. In a study of 45 adult SOT patients with pneumonia, 19 (42.2%) had positive results for HSV-1 PCR in bronchoalveolar lavage (BAL) samples and 11 (24.4%) of these were diagnosed with HSV-1 pneumonia; a definitive case was defined as one in which HSV was the only pathogen identified in the BAL and consistent pathology was present. The HSV viral loads in the cases ranged between 10 3 and 10 7 copies/mL. CT findings of HSV-1 pneumonia are relatively nonspecific and may include bilateral ground-glass attenuation or airspace consolidation.
Disseminated disease, which is uncommon outside the neonatal period, may occur in transplant patients. Typical sites of dissemination include the liver, lungs, adrenal glands, or central nervous system and may manifest as pneumonitis, hepatitis, or meningoencephalitis. Primary HSV has also been identified as a rare trigger for hemophagocytic lymphohistiocytosis in immunocompromised hosts, including oncology patients.
Diagnosis
Detection of HSV-specific antibodies by serology identifies whether a patient is infected and at risk for viral reactivation. However, seropositivity does not preclude superinfection with a related viral strain or different serotype. Screening for HSV serotype-specific immunoglobulin (Ig) G is universally recommended for HSCT but is performed more selectively for oncology patients or as part of the SOT pretransplant evaluation. There is no role for IgM testing as it may be elevated in response to viral reactivation and thus does not accurately identify primary infection. The persistence of maternal antibodies in younger infants can complicate interpretation of serologic test results.
Detection of HSV DNA by PCR has emerged as the diagnostic test of choice for disease and has replaced viral culture or antigen detection methods at most centers. However, the detection of HSV DNA in secretions does not differentiate shedding from disease and must be interpreted carefully. This is particularly important when assessing for HSV pneumonia with oropharyngeal swabs or BAL. Higher viral load in the setting of a compatible clinical presentation supports causality, but the gold standard for invasive disease requires tissue for pathology.
More recently, commercially available assays to detect HSV DNA in the blood (DNAemia) have been recommended for the diagnosis of neonatal HSV disease. The frequency and clinical significance of DNAemia in other clinical settings, including primary or recurrent disease or asymptomatic viral reactivation in either immunocompetent or immunosuppressed hosts, has not been defined. Several studies explored the utility of routine screening for HSV DNA in the blood in SCT patients with variable results. In one study of adult allogeneic SCT recipients who were receiving acyclovir prophylaxis, HSV DNA was detected in weekly obtained blood samples during the first 100 days after transplant in more than 20% of patients, even in the absence of symptomatic disease. However, a retrospective study of more than 500 pediatric SCT patients found that routine PCR screening for HSV or VZV DNA in the blood rarely detected either virus. The authors concluded that targeted testing in patients with mucocutaneous lesions, neurologic symptoms, unexplained fever, or elevated liver enzyme levels may be more appropriate than routine surveillance testing, but no controlled studies have evaluated whether DNAemia warrants antiviral therapy.
Culture-based and immunofluorescent methods of detecting HSV may still have a role for diagnosis of disease in certain settings. Many clinical laboratories continue to use direct detection of HSV with fluorescent antibodies and microscopic analysis to diagnose skin infections, though the availability of PCR-based analyses of samples from skin lesions is increasing. HSV is readily recovered in cell culture from many sites except for cerebrospinal fluid and blood, although culture may take up to 5 days for the virus to grow.
Viral culture, rather than PCR diagnostics, is also important for antiviral resistance testing. Clinically significant infections with acyclovir-resistant HSV strains are more commonly described in immunocompromised patients. Numerous mutations in the thymidine kinase ( TK ) gene or, less commonly, DNA polymerase, are associated with resistance to acyclovir, rendering it difficult to diagnose resistance using sequencing-based methods. Phenotypic resistance testing using a culture-based plaque-reduction assay is the current gold-standard but can take several weeks to obtain a result. A high index of suspicion for development of resistance and empiric changes in antivirals is clinically recommended while resistance test results are pending.
Suppressive therapy and treatment
Suppressive therapy.
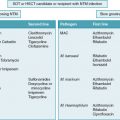
Suppressive therapy, designed to limit replication of reactivating virus, with the nucleoside analog acyclovir or its prodrug, valacyclovir, is recommended by many experts for select transplant and oncology patients who are not receiving ganciclovir or valganciclovir for CMV prophylaxis and are at risk for severe HSV disease ( Table 19.1 ). HSV phosphorylates acyclovir or ganciclovir to the monophosphate, which is further phosphorylated by host cellular kinases to generate acyclovir or ganciclovir triphosphate. The latter are incorporated into replicating viral DNA, leading to premature chain termination. Notably, CMV kinases do not efficiently phosphorylate acyclovir; thus acyclovir is relatively specific for HSV and VZV.
| Population | Drug | Dose b | Duration | References |
|---|---|---|---|---|
| Oncology Patients | ||||
| HSV-seronegative | No prophylaxis recommended | Styczynski et al. | ||
| HSV-seropositive | Acyclovir c | 250 mg/m 2 or 5 mg/kg IV q12 h OR Up to 200 mg PO tid to 800 mg PO bid | 3-5 weeks after start of chemotherapy | Styczynski et al. |
| Valacyclovir | Up to 500 mg PO bid | 3-5 weeks after start of chemotherapy | Styczynski et al. | |
| Famciclovir | Up to 500 mg PO bid | 3-5 weeks after start of chemotherapy | Styczynski et al. | |
| HSV-seropositive leukemia patients undergoing induction or reinduction treatment | Acyclovir | 250 mg/m 2 IV q8 h | Up to 30 days after start of chemotherapy | Saral et al., Freifeld et al. |
| Stem Cell Transplantation Patients | ||||
| HSV-seropositive recipient | Acyclovir c | 750 mg/m 2 IV daily | At least until engraftment, longer if ongoing GVHD treatment | Styczynski et al. |
| Valacyclovir | Up to 500 mg PO bid | Styczynski et al. | ||
| Famciclovir | Up to 500 mg PO bid | Styczynski et al. | ||
| HSV-seropositive, allogenic or autologous SCT recipient | Acyclovir | 250 mg/m 2 IV q8 h | D−3 through D+18 | Freifeld et al. |
| Solid Organ Transplantation Patients | ||||
| HSV-seropositive recipient not receiving CMV antiviral prophylaxis | Acyclovir c | 30-80 mg/kg PO divided tid OR 5 mg/kg IV q8 | At least to D+30, longer if clinical recurrences or if immunosuppression escalated for treating rejection | Wilck et al., Red Book |
| Valacyclovir | 15-30 mg/kg PO tid | Wilck et al. | ||
a Transplant patients not receiving CMV antiviral prophylaxis and highly suppressed oncology patients.
b Dose should be decreased in patients with renal impairment.
c Oral acyclovir has lower bioavailability than valacyclovir; valacyclovir is generally preferred if oral drug is given.
Rates of HSV disease in oncology patients may be reduced with suppressive therapy during periods of intense chemotherapy ; however, there have been surprisingly few randomized clinical trials to evaluate the efficacy of suppressive therapy in this population. In a study conducted in the early 1980s, 29 HSV-seropositive adults with acute leukemia receiving chemotherapy participated in a randomized, double-blind, placebo-controlled trial of acyclovir starting 4 days after their initial chemotherapy. Culture-positive HSV disease developed in 11 of 15 patients who received placebo compared with none of the 14 patients who received acyclovir ( P <.001). Based on these data, suppressive therapy is often recommended, particularly among patients with higher-than-usual risks, including treatment with alemtuzumab (Campath), a monoclonal antibody that binds CD52 on the surface of mature lymphocytes, or other therapies associated with significant suppression of T-cell immunity. B-cell suppression alone with therapies such as rituximab has not been associated with an increased risk of HSV. Some guidelines also support the use of acyclovir in patients at risk for mucositis, although there are limited supporting data.
The risk of HSV disease after SCT is greater than in patients with cancer, leading to universal recommendations for serologic screening and suppressive therapy in seropositive SCT recipients from the start of conditioning through at least neutrophil engraftment and/or until the CD4 + T-cell count is more than 200 cells/μL. , Acyclovir or valacyclovir is also considered during treatment for GVHD, but there are more limited data to support these recommendations. The recommended duration of antiviral treatment in SCT patients depends on the duration and intensity of immunosuppression. There is also some controversy regarding dosing. Lower doses may be effective and are less likely to cause or exacerbate neutropenia or anemia, although concerns about lower acyclovir dosing contributing to resistance have been raised. The renal toxicity attributed to intravenous (IV) acyclovir results from crystallization of drug in the kidneys and can be prevented by IV hydration and slower infusion rates.
Concerns about development of acyclovir resistance during suppressive therapy have not been supported by the limited number of randomized controlled clinical studies. For example, a retrospective study comparing 30 days versus 1 year or longer of antiviral suppressive therapy found that prolonged antiviral therapy was associated with lower rates of viral resistance and significantly decreased rates of HSV disease. As noted earlier, most resistance maps to the gene for thymidine kinase, the viral protein responsible for acyclovir phosphorylation, but mutations in viral DNA polymerase have also been described.
HSV is generally less of a concern in SOT than SCT, and experts vary on recommendations for routine donor or recipient screening and on whether seropositive recipients should receive suppressive therapy. One exception is the rare scenario when a donor has documented HSV at the time organs are harvested. There are few studies on acyclovir suppressive therapy in SOT recipients. One recent Swiss study of 2781 SOT recipients assessed the impact of CMV prophylaxis on rates of HSV or VZV infections. Overall, 1264 (45%) patients received antiviral prophylaxis, primarily ganciclovir or valganciclovir. The incidence of HSV 1 year after transplant was 3.0% (95% confidence 2.2 to 4) in patients receiving antiviral prophylaxis versus 9.8% (95% confidence interval 8.4 to 11.4), in patients without prophylaxis.
Treatment.
IV acyclovir or oral (PO) valacyclovir are the primary drugs for treatment of HSV disease and the choice of IV versus PO depends largely on severity of disease and the ability to tolerate oral therapy. PO acyclovir has relatively poor bioavailability, requiring more frequent dosing, and is less commonly recommended ( Table 19.2 ). Valacyclovir, which is rapidly absorbed, is converted to acyclovir by a hepatic hydrolase. Approximately 55% of an orally administered dose of valacyclovir is available as acyclovir. Pharmacokinetics may be affected by liver disease. Maintaining a high suspicion for HSV disease in the correct clinical context is important, as earlier initiation of treatment can improve outcomes. As with CMV and Epstein-Barr virus, a reduction in immune suppression, if feasible, is also recommended as part of HSV treatment. Steroids have been administered to patients with HSV encephalitis or severe corneal disease as an adjunctive antiinflammatory therapy, but randomized clinical trials to establish benefit have not been completed.
| Population | Drug | Dose a | Duration | References |
|---|---|---|---|---|
| Oncology or SCT Patients | ||||
| Severe mucocutaneous or visceral disease | Acyclovir | 250 mg/m 2 or 5 mg/kg IV q8h | Styczynski et al. | |
| Pneumonia, meningitis, or encephalitis | Acyclovir | 500 mg/m 2 or 10 mg/kg IV q8h | 14-21 days | Styczynski et al. |
| Milder disease | Acyclovir b | 200-400 mg PO 5 times daily | 10 days | Styczynski et al. |
| Valacyclovir | 500 mg PO bid | 10 days | Styczynski et al. | |
| Famciclovir | 500 mg PO bid | 10 days | Styczynski et al. | |
| Acyclovir-resistant virus | ||||
| Foscarnet | 60 mg/kg IV q12h OR 40 mg/kg IV q8h | 7-21 days or until complete healing | Styczynski et al. | |
| Acyclovir-resistant and foscarnet-resistant virus | ||||
| Cidofovir | 5 mg/kg IV once weekly for 2 weeks, then once every 2 weeks, combined with probenecid and IV hydration | Styczynski et al. | ||
| Optional topical treatment for accessible cutaneous lesions | Trifluridine 5% ophthalmic solution | q8h | Styczynski et al. | |
| Cidofovir gel 0.3 or 1% | Once daily | |||
| Solid Organ Transplantation | ||||
| Disseminated, visceral, extensive mucocutaneous disease, or encephalitis/meningitis | Acyclovir | 10-20 mg/kg IV q8h | 14-21 days | Wilck et al. |
| Milder mucocutaneous disease | Acyclovir | 5-10 mg/kg IV q8h | 5-7 days or until complete healing of the lesions (can transition to PO when improving) | Wilck et al. |
| Acyclovir b | 80 mg/kg PO divided 3-5 times daily, up to 1000 mg/day | 5-7 days or until complete healing of the lesions | Wilck et al. | |
| Valacyclovir | 20 mg/kg per dose PO twice daily, up to 1000 mg/dose | Wilck et al. | ||
| Famciclovir | 500 mg PO bid (adult dose) | Wilck et al. | ||
| Acyclovir-resistant virus | Same recommendations as for oncology and SCT patients | Wilck et al. | ||
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree