Major Concepts
Infection
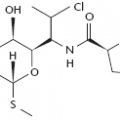
Helicobacter pylori is a spiral-shaped, mobile, gram-negative bacillus with two to seven flagella. These bacteria inhabit the human gastric mucosa, like the Campylobacter species they resemble. The bacteria produce a powerful urease enzyme that increases stomach pH by degrading urea into ammonia and carbonic acid, as well as several virulence factors. Other Helicobacter species also inhabit humans. These include H. cinaedi and H. fennelliae from the intestines or blood of homosexual men with proctitis, colitis, or HIV infection; infections with these bacteria result in bacteremia, fever, leukopenia and thrombocytopenia. H. westmeadii is also found in the blood of HIV-positive individuals. H. pullorum, H. canis, and H. rappini from chickens, cats, dogs, sheep, and mice cause diarrhea in humans as well.
Diseases
Infection with H. pylori is associated with several gastrointestinal (GI) tract diseases. Most persons with gastric or duodenal ulcers, chronic gastritis, intestinal metaplasia, gastric adenocarcinoma of the distal stomach, and gastric MALT lymphoma are infected with these bacteria. Treatments that eradicate the organisms decrease gastritis and ulcers and lower the risk of developing gastric malignancies. In contrast, due to H. pylori’s ability to increase gastric pH, infection appears to lower the chances of developing GERD, Barrett esophagus, and the highly pathogenic adenocarcinoma of the lower esophagus.
Immune Response
H. pylori infection promotes transit of neutrophils and lymphocytes into the gastric mucosa, where they produce several immune mediators, including Th1-related cytokines, chemokines, inflammatory cytokines, and regulatory cytokines. Regulatory cytokines may decrease protective immunity to the extent that the host is unable to completely eliminate the bacteria, resulting in lifelong infection. Vaccine attempts have been largely unsuccessful when tested in phase I clinical trails, but some promising work has been reported in the mouse model of infection. Protection in these animals is associated with the induction of Th1 immunity.
Setting
H. pylori is one of the most common bacterial species that infects humans, and it has done so for over 50,000 years. Developing areas of the world have high rates of infection, and colonization usually occurs during childhood. Persons from developed nations have much lower rates of infection that increase with age. Persons colonized early in life are more likely to develop gastric symptoms, while those infected later in life are more likely to present with duodenal ulcers instead. Infection rates and gastric diseases are decreasing in developed areas but not in developing regions. Socioeconomic factors such as crowding, proper hygiene, and access to treatment help determine prevalence in a given population. Within a given geographical area, the incidence of infection may differ greatly; this is true for the Native Alaskans and Canadian First Nation communities in comparison with the Caucasian population of the regions.
Protection
Bacteria are usually eradicated by a combination of agents that suppress acidity, a bismuth compound, and several antibiotics. While highly effective, the cost of such treatment may be not be affordable by many persons in developing regions. Research is being conducted to determine the utility of less costly and more readily available alternatives in the form of neutraceuticals.
Helicobacter pylori bacteria have inhabited the stomach mucosa of men, women, and children throughout the world since before the emergence of the human species from Africa. They are currently one of the most prevalent microorganisms of humans and are responsible for the majority of peptic ulcers and gastric cancer, yet they were not isolated until 1982 and their role in disease was not acknowledged until 12 years later after much dissention from the medical and scientific communities. In developing nations, most people are colonized with these bacteria before the age of 10 years, and 70% to 90% of the people are eventually infected. In developed countries, the rate of infection is much lower (20% to 50%) and increases with age. Colonization of children in developed countries (currently approximately 10%) is believed to have been more common several decades ago (40% to 60%) because infection rate has been linked to socioeconomic conditions—infection is higher among individuals living in larger families or crowded conditions, those raised in poorer or less hygienic conditions, smokers, and those who consume less fruit, and such conditions are less common in developed areas now than in the past. In developed nations, however, groups with higher incidence of infection persist, including Native Alaskans in the United States. Once infected, people usually remain infected throughout their lives unless treated or unless severe chronic gastritis occurs, killing the bacteria. H. pylori infection is classified as emerging not because of its actual entry into the human population but rather due to our relatively recent discovery of the link between these bacteria and a variety of gastroduodenal diseases.
In 1875 and 1889, spiral bacteria were discovered in gastric ulcers and gastric aspirations and a potential role in causing peptic ulcers was first postulated. These and other findings of similar bacteria in gastric mucosa of dogs, cats, and monkeys were largely ignored, however, until 1979 and 1982 when two Australian researchers began the lengthy process of altering long-held views concerning gastric disease. At that time, infection with the spiralbacteria was suggested to lead to gastric disorders by Robin Warren, and following up on this hypothesis, the bacteria were successfully cultured and isolated by Barry Marshall. The bacteria were initially named Campylobacter pyloridis but were reclassified as Helicobacter pylori in 1989. Although Marshall and Warren’s work presented strong evidence that the bacterial infection caused conditions such as chronic gastritis and peptic ulcers, the scientific community preemptively rejected their findings because they contradicted conventional knowledge that taught that ulcers were due to stress and dietary factors and urged bed rest and bland food for ulcer sufferers, treatment modalities that did nothing to prevent ulcer recurrence. The validity of their claims was eventually proved by human volunteers ingesting the spiral bacteria and subsequently contracting peptic ulcers that were later cured by the eradication of the bacteria. In 1994, Marshall and Warren’s claims were substantiated by the National Institutes of Health, and persons throughout the world suffering from peptic ulcers and chronic gastritis were able to be cured by a relatively quick and simple treatment regimen. The dedication of these scientists in the face of firm opposition by most physicians and researchers has improved the quality of many persons’ lives. In recognition of their efforts, Warren and Marshall received the Nobel Prize in Medicine or Physiology in 2005. Recently, additional members of the Helicobacter genus have been discovered in domestic animals. Several of these species also infect humans’ stomach, intestines, gallbladder, and blood and are associated with gastrointestinal diseases, leading to the suggestion that infection of animals may lead to zoonotic transmission to humans.
H. pylori infection was also found to cause cancers, such as distal gastric adenocarcinomas and gastric MALT lymphomas. Eradication of H. pylori in Alzheimer’s disease patients was also found in one study to lead to increased cognitive and functional status two years later. Infection has been suggested to play a causal role in a subset of individuals with autoimmune thrombocytopenic purpura as well because antibodies against the bacteria’s urease B protein are cross-reactive with a glycoprotein found on human platelets and inhibited the aggregation of these cells. Interestingly, the bacteria have also been postulated to play a protective role against the development of gastroesophageal reflux disease, Barrett esophagus, and adenocarcinoma of the lower esophagus.
Almost all persons infected by H. pylori develop chronic gastric inflammation; however, many never develop any corresponding symptoms. Other infected persons do suffer from one or more upper abdominal disorders.
Peptic Ulcer Disease
The origin of peptic ulcer disease has long been a matter of contention. Certain peptic ulcers are known to be caused by aspirin and other nonsteroidal anti-inflammatory drugs, excessive alcohol use, or other illnesses such as Crohn’s disease or Zollinger-Ellison syndrome. But the cause of approximately 80% of ulcers was unknown until it was discovered that H. pylori bacteria were almost always present in such ulcers. Eradication of the bacteria dramatically decreased the rate of ulcer recurrence, which had been greater than 30% in the first year in patients continuing acid-suppressive therapy without killing the bacteria.
Most people who are infected with H. pylori (90% of those in developed regions) do not develop peptic ulcers. Ulcers occur more readily in individuals infected by cagA+ strains of H. pylori and strains that produce more vacuolating cytotoxin (described in the discussion of the causative agent). Environmental and genetic factors also affect the chances that an infected person will develop an ulcer. These factors include cigarette smoking, having blood type O, and certain major histocompatibility class II antigens. Ulcer location may be a function of age of infection, for people living in developing regions where colonization generally occurs during childhood tend to produce gastric ulcers, whereas people living in developed regions where colonization occurs later in life have a higher prevalence of duodenal ulcers. Alterations in gastric acid production may lead to the production of duodenal gastric metaplasia, in which the duodenal epithelium cells assume a more gastriclike morphology, enhancing the ability of H. pylori to colonize this region. The presence of duodenal gastric metaplasia and infection with H. pylori is associated with increased risk of developing duodenal ulcers.
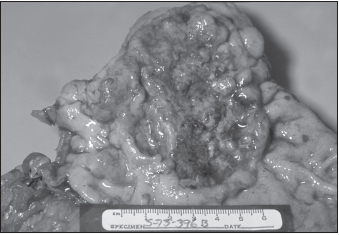
Gastric Cancer
Chronic inflammatory responses directed against H. pylori lead to long-term destruction of the normal gastric mucosal architecture (chronic gastritis) as the gastric glands that secrete “gastric juice” are lost and replaced by fibrotic and intestinal metaplastic cells differing in histological type (intestinal metaplasia). The gastric glands are responsible for the secretion of the digestive enzyme pepsin, hydrochloric acid, intrinsic factor (required for vitamin B12 absorption and red blood cell production), and the mucus that protects the mucosal cells lining the stomach from acid-related damage. Chronic gastritis and intestinal metaplasia increase the risk for gastric cancer by 5- to 90-fold, depending on their severity and the type of metaplasia. Individuals whose metaplastic cells are similar to colon epithelium have a higher risk than those whose cells are similar to small intestinal epithelium. People infected with H. pylori are most likely to develop the inflammatory conditions that cause gastric cancer, and infection with these bacteria is linked to cancer of the distal stomach. Because of the link between H. pylori infection and gastric cancer, the World Health Organization’s International Agency for Research on Cancer classified these bacteria as a class I carcinogen in 1994. As socioeconomic conditions have improved over the past six decades in developed countries, the rate of infection with H. pylori and the prevalence of gastric cancer have decreased from 30 cases per 100,000 persons per year to 5 cases per 100,000. Perhaps the decreasing incidence of H. pylori infection in developing countries will have a similarly positive effect on gastric cancer occurrence. As with peptic ulcers, cagA+ strains of bacteria cause more severe inflammation and are associated with a higher risk for developing gastric cancer.
Stomach acidity may play a role in the development of gastric cancer. H. pylori typically inhabits and causes cancer in the distal portions of the stomach where the pH is in the range 5–6 because this region of the stomach is away from the acid-producing parietal cells. If acid production is decreased by either the use of acid-suppressive medications or destruction of parietal cells by atrophic gastritis, the higher pH may allow H. pylori to inhabit more proximal portions of the stomach or penetrate more deeply into gastric pits. Persons with gastric ulcers have lower levels of acid production than those with duodenal ulcers and have a fourfold higher risk of developing gastric cancer.
Gastric MALT Lymphoma
Gastric MALT lymphoma is the result of large numbers of lymphocytes entering into the stomach and forming a solid mass. (MALT refers to mucosal-associated lymphoid tissue—collections of immune cells in mucous-producing regions, such as the Peyer’s patches of the intestine.) Lymphocytes are not typically found in the stomach mucosa in the absence of infection by bacteria such as H. pylori. When these bacteria do infect the stomach, lymphocytes, usually B cells, enter the gastric epithelium and form lymphoid follicles. This may form the basis of the finding that almost all individuals with gastric lymphomas are also infected by H. pylori and that a one-week course of bacterial eradication leads to a 70% rate of complete remission of the lymphoma.
Association with Other Diseases
Hypertrophic Protein-Losing Gastritis
Hypertrophic protein-losing gastritis is characterized by chronic gastritis with giant folds in the stomach wall, protein loss in the stomach, and hypoalbuminemia (low levels of albumin, the most prevalent blood protein). Although the cause of this condition remains unknown, treatment that eradicates H. pylori leads to significant improvement.
Gastroesophageal Reflux Disease (GERD), Barrett Esophagus, and Adenocarcinoma of the Lower Esophagus
Recent evidence suggests that the incidence of gastroesophageal reflux disease (GERD) and its complications of Barrett esophagus and adenocarcinomas of the lower esophagus may be decreased by H. pylori infection. During GERD, the acidified food or liquid contents of the stomach travel backward into the lower esophagus, possibly leading to irritation. Approximately 40% of the population of the Western world experiences symptoms of GERD (heartburn, belching, nausea, vomiting, sore throat, difficulty swallowing) in a given month. Barrett esophagus is a metaplastic alteration of the esophageal epithelium that occurs in 10% to 20% of individuals with GERD and is about twice as common in males as in females. Barrett esophagus results from attempts to repair acid-induced damage to the lower esophagus in which the normal esophageal lining of stratified squamous epithelium is replaced by the more acid-resistant columnar epithelium, which has a greater tendency to undergo malignant transformation. It is a predisposing factor for adenocarcinoma of the lower esophagus, a particularly pathogenic malignancy whose incidence is rapidly increasing in the United States. This cancer has a poor prognosis, with a three-year survival rate of 20%. The recent decrease in rates of H. pylori infection in developed countries has been paralleled by an increase in the prevalence of adenocarcinomas of the lower esophagus. Eradication of these bacteria also increases the incidence of GERD. The ability of H. pylori to raise stomach pH by decreasing acid production together with the activity of its urease enzyme (discussed further later in this chapter) may help protect the host against GERD and its complications. CagA+ strains appear to be most protective in decreasing incidence of Barrett esophagus and adenocarcinoma of the esophagus.
Helicobacter pylori
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree