Major Concepts
Symptoms
Babesiosis is an emerging infectious disease among people living in temperate areas of the world. Though often asymptomatic in younger healthy individuals, this illness may be very serious or fatal in immunocompromised persons. People at high risk for severe disease include those who lack a spleen, are over the age of 50 years, or are immunosuppressed. Illness in these persons may lead to development of high fever, pulmonary edema, hemolytic anemia, hemoglobin in the urine, renal failure, disseminated intravascular coagulation, adult respiratory distress syndrome, and multiorgan failure.
Infection
Most cases of babesiosis result from infection with Babesia divergens (in Europe), B. microti (in the northeastern United States), or Babesia isolate type WA-1 (in the western United States). Infection with B. divergens leads to the most severe pathology. Babesia species are parasitic protozoa belonging to the phylum Apicomplexa. Several species produce lethal infections in animals, including cattle, horses, and dogs. Apicomplexa includes several other genera of closely related human and animal pathogens such as Theileria (in cattle), Plasmodium (which causes malaria in humans and animals), and Eimeria (in birds). These parasites have significant negative effects on the economy and agriculture of affected regions. Babesia protozoa are transmitted to humans by deer ticks, and pathology is magnified by coinfection with Borrelia burgdorferi (the causative agent of Lyme disease), which is transmitted by the same species of tick. In addition to the domestic animals listed, several mammals in the wild (white-footed mice, mule deer, bighorn sheep, voles, and shrews) serve as hosts and potential reservoir species.
Immune Response
Several elements of the host immune response are protective, including IgG antibodies, NK cells, macrophages, and CD4+ Th1 helper lymphocytes. These last, however, may interfere with defense against Lyme disease, which relies on a Th2 lymphocyte response. Other elements of the immune system such as IgM antibody and complement may in fact worsen babesiosis.
Protection
Preventive measures for babesiosis are similar to those used for erhlichiosis and Lyme disease. They involve decreasing host contact with infected ticks or tick removal prior to the introduction of the infective form of the parasite to the vertebrate host.
Babesiosis (also known as piroplasmosis) is a potentially serious illness resulting from infection of erythrocytes with a parasitic protozoan belonging to one of several species of Babesia. These intracellular parasites are similar to the causative agents of malaria in humans, and the disease induced by Babesia is usually similar to a mild case of malaria. Among individuals with decreased immune responses, however, the illness is much more severe and may even prove fatal. Hundreds of cases of babesiosis have been identified since it was first reported in humans in the late 1950s; in New Jersey alone, 189 cases were noted between 1989 and 2004, and in New York, 560 cases were recorded between 1986 and 2001. This illness is found in scattered locations around the world, including portions of the United States that are home to deer ticks, one of the disease vectors. Some areas of the country in which the parasite is endemic include islands off of the Atlantic Coast (Nantucket, Block Island, and Shelter Island), eastern Long Island, Maine, upstate New York, southern Connecticut, Massachusetts, Rhode Island, New Jersey, Wisconsin, Minnesota, Missouri, California, and Washington. Mexico has reported cases of infection, as have European countries, including France, Ireland, Scotland, Spain, Switzerland, Sweden, Russia, and Yugoslavia. Infection with various Babesia species has also occurred in China, Taiwan, Japan, Korea, Egypt, South Africa, Mozambique, and the Canary Islands.
Babesiosis is one of the most common infections of free-living animals worldwide and is problematic for agriculture. Babesia bovis causes a severe disease in cattle known as Texas cattle fever (redwater fever). The effects of this and similar diseases on livestock severely diminish food availability and economic health in some regions of the world. Other species of Babesia cause serious disease in horses and dogs (discussed later in this chapter). The freed lioness Elsa, featured in the film Born Free, succumbed to Babesia infection.
Babesia species were first described by the Romanian scientist Viktor Babes¸ in 1888, who found them in the erythrocytes of cattle. Babesiosis may, however, have been noted much earlier as the plague of the Egyptian cattle described in Exodus. Infection of humans with Babesia divergens was first noted in 1957 in a 33-year old asplenic (lacking a spleen) farmer in Yugoslavia who had grazed his herd of infected cattle in a tick-infested field. A number of cases were detected over the next 20 years in Russia. Most individuals with symptomatic infection have lost their spleens. In these people, disease is severe and symptoms include fever, hemolytic anemia, and hemoglobin in the urine and renal failure resembling malarial blackwater fever. In the United States, human babesiosis was first recognized in California, and later, a separate species, Babesia microti, was found to cause human illness on Nantucket, off the coast of Massachusetts (Nantucket fever) in the mid-1960s and 1970s. Some areas not known to be endemic were found on closer examination to have widespread infection that is mounting over time due to a combination of increased tick prevalence and range, better surveillance and reporting of infection, and greater awareness of the disease. These areas include south and central New Jersey, where 2 cases were reported in 1994 and 48 in 2004. A third species, Babesia isolate type WA-1, was discovered to be the cause of an acute malaria-like disease in Washington in 1991. In 1991 and 1993, isolate type CA-1 was found in California. This isolate is closely related to, but distinct from, type WA-1. Isolate type MO-1 caused a fatal disease in a 73-year-old splenectomized man in Missouri in 1992. Type MO-1 is similar to B. divergens in Europe, although this individual had never traveled outside of the United States and rarely left his home state.
Babesiosis is an arthropod-borne disease caused by infection of erythrocytes with one of three species of Babesia (piroplasms). Given the cellular location and the appearance of the parasites, babesiosis may be mistaken for malaria. Some 25% of infections in adults and 50% of those in children are asymptomatic or resolve without treatment. Nevertheless, babesiosis is a potentially severe or even fatal condition. In the United States, the mortality rate is about 5%, but in Europe, 42% of the infected become comatose and die. Babesiosis in the United States and in Europe are caused by different species of parasite. Furthermore, most of the European cases occur in asplenic individuals, who may be at greater risk in that the spleen is a major organ of the immune system in which many B lymphocytes, which produce antibodies, and phagocytic macrophages reside. Its removal thus results in immunosuppression.
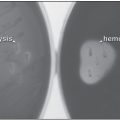
The incubation period ranges from 1 to 8 weeks. The symptoms of babesiosis include persistent fever as high as 41°C (105.8°F), intense sweating, shaking chills, malaise, depression, sensitivity to light, stiffness of the neck, cough, shortness of breath, pulmonary edema, nausea, vomiting, abdominal pain, bone pain, rigors, myalgia, headache, fatigue, hypotension, and hepatosplenomegaly. Laboratory findings may include thrombocytopenia and high levels of serum transaminase, alkaline phosphatases, unconjugated bilirubin, and lactic dehydrogenase. Jaundice may result from hemolytic anemia, which lasts from days to several months. Severe renal symptoms include hemoglobin in the urine (released from lysed red blood cells) and renal failure. Other extremely serious disease manifestations include disseminated intravascular coagulation, adult respiratory distress syndrome, and multiorgan failure.
In individuals without clinical signs of infection, parasitemia (presence of parasites dividing in the blood) persists for months or years. Symptoms may resume after a year of an asymptomatic parasitemia. Although serious disease manifestations can occur in previously healthy persons, immunocompromised individuals, including those without a spleen (particularly true for infection with B. divergens), older individuals (over the age of 50 years), and those receiving immunosuppressive drugs during chemotherapy for cancer or to prevent rejection of transplanted organs, are at increased risk of developing severe symptoms after infection. In areas with large or rising numbers of HIV-infected persons, this infection may become more problematic as persons with inapparent infections with Babesia lose immune functions during the course of HIV disease progression. The increase in the elderly population may also affect the numbers of susceptible individuals. Other conditions that weaken the immune response, such as diabetes, have also been associated with higher risk for symptomatic babesiosis.
Coinfection of a person with another tickborne microbe, Borrelia burgdorferi, may occur. This bacterial spirochete causes Lyme disease, and dual infection increases the severity of both conditions. Infection with Borrelia persists longer in coinfected persons, and they are more likely to develop persistent postinfection fatigue. Surveys of deer ticks in endemic areas often detect the presence of both microbes in individual ticks. In the United States, 20% of humans with Babesia infection are coinfected with Borrelia. Ehrlichia species and Anaplasma species are also transmitted by deer ticks in the United States. The former infect white blood cells, as is the case for Theileria species. These tickborne infections are discussed in other chapters.
In addition to humans, Babesia species cause serious illness in animals, including some domestic livestock of agricultural importance and some species of birds. Dogs, cattle, and horses may develop disease. Among dogs, B. canis and B. gibsoni are the most common disease-causing species. Racing greyhounds and pitbulls are particularly affected by these species. Illness in canines may be acute, hyperacute, or chronic. During the acute form, dogs may develop fever, jaundice, hemoglobinuria, anemia, or death. Infection may be transmitted between dogs by biting. Theileria equi (Babesia equi) and B. caballi are the species found in horses, while B. bovis, B. divergens, B. bigemina, and B. major infect cattle. In horses, T. equi may cause acute tickborne hemolytic anemia that progresses into a chronic carrier state. This illness leads to reduced oxygen-carrying capacity and poor performance of racehorses. B. bigemina, the cattle pathogen, may have the most impact on the economy of Europe and other major cattle-producing countries. In the infected cattle, 30% to 45% of the erythrocytes may be parasitized and then destroyed. In addition to the symptoms seen in humans, infected cattle may be unable to rise and may experience severe dehydration, diarrhea that is followed by constipation, lower than normal body temperature, and reduced levels of oxygen in the brain, leading to behavioral changes. They have very rapid heart rates with extremely loud cardiac sounds that can be heard even from a distance of several feet. Toxemic shock may subsequently result in death. In addition to domestic animals, this protozoan may also parasitize water buffalo and wild ruminants, such as reindeer, in other regions of the world.
Table 25.1 Tickborne diseases of humans
| Disease | Microbe | Tick |
| Babesiosis | Babesia divergens, B. microti | Deer tick (Ixodes scapularis, I. ricinus) |
| Ehrlichiosis | Ehrlichia chaffeensis, E. ewinigii | Lone star tick (Amblyomma americanum) |
| Anaplasmosis | Anaplasma phagocytophilum | Deer tick (I. scapularis), western black-legged tick (I. pacificus) |
| Lyme disease | Borrelia burgdorferi | Lone star tick (A. americanum) |
| Southern tick-associated rash illness | Borrelia lonestari | Lone star tick (A. americanum) |
| Rocky Mountain spotted fever | Rickettsia rickettsii | American dog tick (Dermacentor variabilis), Rocky Mountain wood tick (D. andersoni) |
| Tularemia | Francisella tularensis | Dog tick (D. variabilis), Rocky Mountain wood tick (D. andersoni), Lone star tick (A. americanum) |
| Tickborne relapsing fever | Borrelia parkeri, Borrelia hermsii | Soft ticks (Ornithodoros parkeri, Ornithodoros hermsii) |
| Colorado tick fever | Colorado tick fever virus | Wood ticks (D. andersoni) |
Table 25.2 Babesia species and their hosts
| Babesia Species | Animals Infected |