8 Head and neck cancer
Aetiology
The important aetiological factors in squamous cell carcinomas of the head and neck include:
Pathogenesis and pathology
SCC is thought to develop in a stepwise progression from squamous metaplasia to dysplasia, through carcinoma-in-situ to invasive squamous cell carcinoma. These histological changes are accompanied by molecular alterations which disrupt the regulation of cell proliferation, by inactivating tumour suppressor genes and activating oncogenes.
The majority (90%) of malignant tumours of the head and neck are squamous cell carcinomas. The WHO classification of head and neck cancers is outlined in Box 8.1.
Anatomy
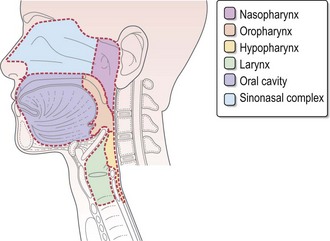
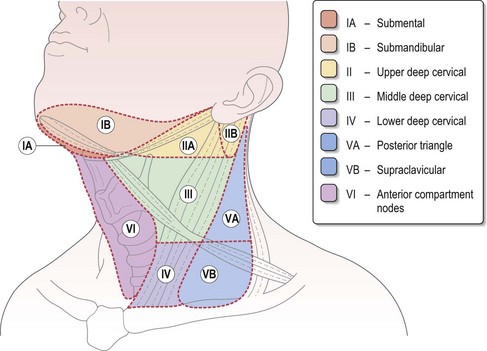
Figure 8.1 shows the anatomical sites in the head and neck. Figure 8.2 demonstrates the anatomical levels of neck nodes and the typical regional lymphatic drainage for head and neck subsites, which are important in planning surgery and radiotherapy. In the unoperated neck, the pattern of lymph node drainage is relatively predictable for different tumour subsites. The risk of occult lymph node metastasis varies according to the primary site and the size of the primary tumour. Clinical assessment of this risk of cervical nodal metastasis dictates subsequent decisions on inclusion of lymph node groups within a neck dissection or radiotherapy target volume during the definitive treatment.
Evaluation of patients with head and neck cancer
Important features in the history for head and neck cancer patients are:
Investigations and staging
The objectives of the clinical assessment of a patient with a suspected head and neck cancer are:
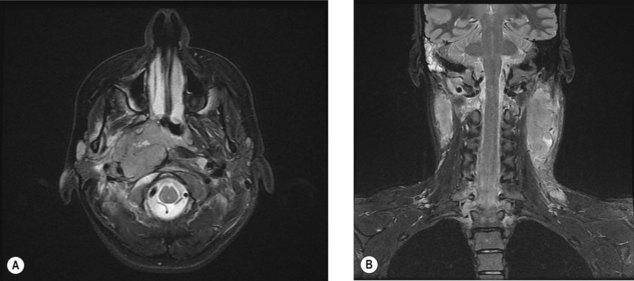
Imaging
Staging
TNM staging is based on the primary tumour size and/or extent, regional lymph node metastasis and distant metastatic spread (Box 8.2).
Box 8.2
A general TNM staging of head and neck tumour
| Stage I | T1N0M0 | tumour of ≤2 cm |
| Stage II | T2N0M0 | tumour of >2–4 cm |
| Stage III | T3N0M0 | tumour of >4 cm |
| T1–3N1M0 | ipsilateral single node ≤3 cm | |
| Stage IV | T4N0–1M0 | involving adjacent structures |
| Any T N2M0 | ipsilateral single node >3–6 cm (N2a) | |
| ipsilateral multiple nodes <6 cm (N2b) | ||
| contralateral or bilateral nodes <6 cm (N2c) | ||
| Any T N3M0 | nodes >6 cm | |
| Any T, any N, M1 | Distant metastasis |
Management of head and neck cancers
Pre-treatment assessment
Management of head and neck cancers is complex, and needs a multidisciplinary approach. All patients require assessment of performance status, dentition, swallowing and nutrition. Dental assessment is important in minimizing late side effects of radical radiotherapy such as dental caries and osteoradionecrosis. Maintaining adequate nutrition is a challenge in patients with head and neck cancer. Patients who are malnourished or at risk of becoming malnourished need dietetic assessment and often intervention is needed. All patients with locally advanced head and neck cancer need a swallowing and language therapy (SALT) assessment prior to radical treatment. Patients are encouraged to stop smoking and minimize alcohol intake during radiotherapy.
Principles of treatment
Early stage disease (stages I–II/T1–2N0M0)
Early stage disease is usually managed with either surgery or radiotherapy. The choice of treatment is based on location of tumour and anticipated morbidity. Radiotherapy results in a local control rate of 85–95% for T1 and 70–85% for T2 lesions. Treatment of the neck should be considered in addition to the treatment to the primary site. Node negative head and neck cancers with a >15–20% risk of occult cervical node metastasis (all cancers except <2 cm lesions in oral cavity and T1 glottic cancers) need elective management of neck nodes – either by a neck dissection or neck irradiation. The level(s) of nodes to be treated depends on the primary site of tumour and T stage, and the choice of treatment modality depends on the treatment of the primary site (Box 8.3).
Box 8.3
Recommended elective node treatment in stage I–II (T1–2N0) head and neck cancer
| Primary site | Nodal irradiation in N0 disease | Selective node dissection in N0 disease |
|---|---|---|
| Oral cavity: | ||
| T2 well lateralized | Ipsilateral level I–II | I–III |
| T2 reaching midline | Bilateral level I–III | |
| Oropharynx: | ||
| T1 Tonsil | Ipsilateral Ib–II | II–IV |
| T2 lateralized tonsil | Ipsilateral Ib–IV | |
| All other N0 | Bilateral Ib–V | |
| Larynx: | ||
| T1–2 Glottic | No nodal radiotherapy | II–IV and if extends below glottis, II–V |
| T1/2 Supraglottic | Bilateral level Ib–III | |
| All other N0 | Bilateral Ib–V | |
| Hypopharynx: | ||
| All N0 | Bilateral I–V | II–V |
| Nasopharynx: | ||
| T1N0 squamous carcinoma | No neck irradiation | – |
| All N0 | Bilateral I–V |