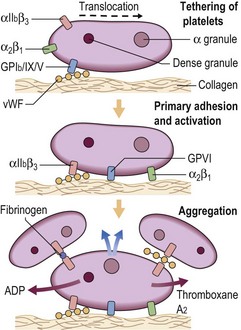
6 Following damage to a blood vessel there is immediate vasoconstriction to slow blood flow and reduce the risk of exsanguination. The break in the endothelial cell barrier leads to the recruitment of platelets from the circulation to form an occlusive plug. Platelets interact both with the vessel subendothelial matrix (platelet ‘adhesion’) and with each other (platelet ‘aggregation’) (Fig 6.1). The first step in this process, adhesion, does not require platelet metabolic activity. It does, however, lead to the ‘activation’ of platelets.
Haemostasis
The role of platelets
 the glycoprotein (GP) Ia/IIa complex (α2β1 integrin) and glycoprotein (GP) VI which are receptors for collagen
the glycoprotein (GP) Ia/IIa complex (α2β1 integrin) and glycoprotein (GP) VI which are receptors for collagen
 the GPIb/IX/V complex, a receptor for vessel wall von Willebrand factor (vWF) and thrombin
the GPIb/IX/V complex, a receptor for vessel wall von Willebrand factor (vWF) and thrombin
 the GPIIb/IIIa complex (αIIbβ3 integrin), which is an agonist-induced receptor for fibrinogen and vWF (vWF is discussed in more detail on p. 74).
the GPIIb/IIIa complex (αIIbβ3 integrin), which is an agonist-induced receptor for fibrinogen and vWF (vWF is discussed in more detail on p. 74).
Oncohema Key
Fastest Oncology & Hematology Insight Engine